Understanding Piles (Hemorrhoids): Causes, Diagnosis, and Treatment Options
Piles, also commonly known as hemorrhoids, are a very common condition affecting millions of people worldwide. While often uncomfortable and sometimes painful, they are usually not serious and can often be managed effectively. This article explores what piles are, why they happen, how they are diagnosed, and the various treatment options available.
What are Piles (Hemorrhoids)?
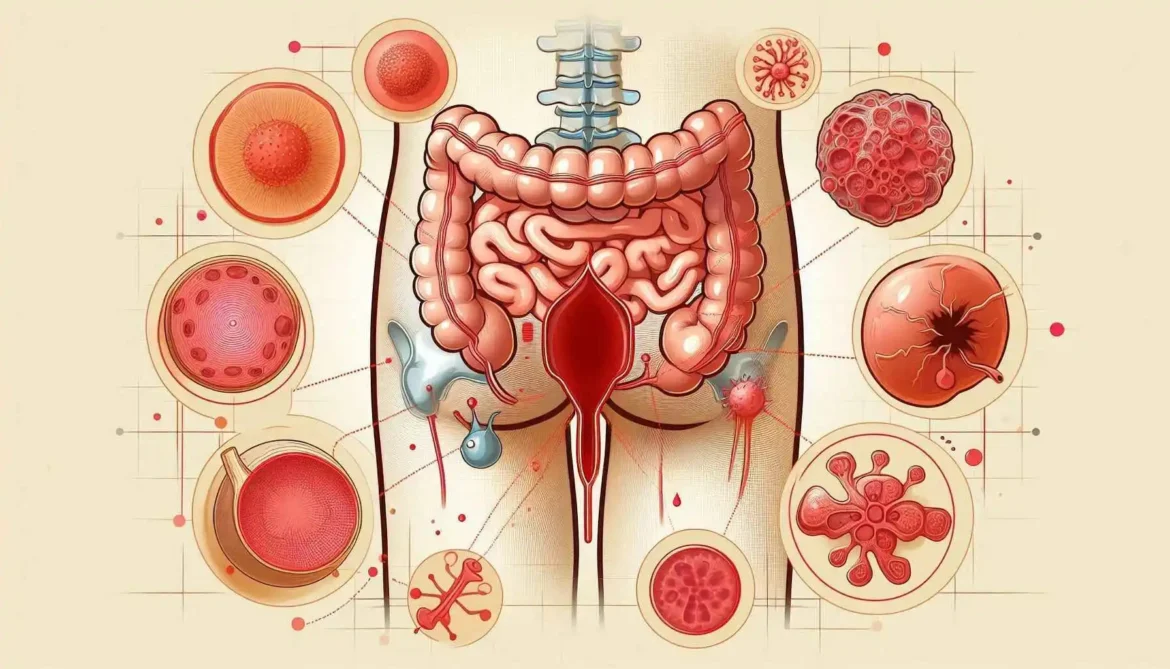
Piles are swollen and inflamed veins located in the lower rectum and anus. These veins are part of the normal anatomy of the area, acting as cushions of blood vessels that help control bowel movements. However, when excessive pressure or other factors cause these veins to stretch, swell, and become irritated, they can develop into piles.
Piles are generally classified into two main types:
- Internal Piles: These occur inside the rectum and are usually painless because there are fewer pain-sensing nerves there. The most common symptom is painless bleeding during bowel movements, where bright red blood may appear on the stool, toilet paper, or in the toilet bowl. If an internal pile enlarges, it may prolapse (protrude) outside the anus, which can then cause pain and discomfort.
- External Piles: These occur under the skin around the anus, where there are more pain-sensing nerves. External piles can cause itching, pain, swelling, and a hard lump around the anus when a blood clot forms inside (thrombosed external hemorrhoid), which can be very painful.
- Unveiling the Types: Internal vs. External Piles
- Piles are broadly classified into two main types, depending on their location within the anorectal region: internal piles and external piles. Understanding this distinction is crucial because it influences the symptoms experienced and the treatment approaches.
| Feature | Internal Piles | External Piles |
| Location | Inside the rectum, above the dentate line | Under the skin around the anus, below the dentate line |
| Nerve Endings | Fewer pain-sensitive nerve endings | Abundant pain-sensitive nerve endings |
| Visibility | Not usually visible, unless prolapsed | Visible as bulges around the anus |
| Pain Level | Generally less painful, often painless bleeding | Generally more painful, especially thrombosed external piles |
| Symptoms | Rectal bleeding, prolapse, mucus discharge, itching | Pain, itching, swelling, bleeding, difficulty cleaning |
Causes of Piles
Piles develop when there is increased pressure in the veins in the lower rectum and anus. Several factors can contribute to this increased pressure:
- Straining during bowel movements: This is one of the most common causes, often due to constipation or diarrhea.
- Chronic constipation or diarrhea: Both conditions can lead to excessive straining or frequent toilet trips.
- Pregnancy: The growing uterus puts pressure on the veins in the pelvis, and hormonal changes can also relax the supporting tissues.
- Sitting for long periods: Especially sitting on the toilet, as this can put pressure on the anal veins.
- Obesity: Excess body weight can increase pressure in the pelvic area.
- Heavy lifting: Can cause temporary pressure build-up.
- Low-fiber diet: This often leads to constipation and straining.
- Aging: Tissues supporting the veins in the rectum and anus can weaken with age.
- Family history: There may be a genetic predisposition in some cases.
Recognizing the Signs: Common Symptoms of Piles
The symptoms of piles can vary depending on the type and severity. Being aware of these symptoms can help us seek timely attention and manage the condition effectively.
Common Symptoms Include:
- Rectal Bleeding: Usually painless, bright red blood, often seen on toilet paper, in the toilet bowl, or streaking the stool.
- Pain or Discomfort: Pain may be present, especially with external piles or thrombosed piles. Discomfort, aching, or a feeling of pressure in the anal area is also common.
- Itching: Irritation and inflammation can cause itching around the anus.
- Swelling or Lumps: You might feel or see soft lumps around the anus, especially with external piles. Prolapsed internal piles can also be felt as lumps outside the anus.
- Mucus Discharge: Internal piles can sometimes produce mucus, leading to anal leakage or a feeling of incomplete bowel emptying.
- Fecal Soiling: In severe cases, prolapsed piles can make it difficult to clean the anal area properly, leading to soiling and discomfort.
Diagnosing Piles
Diagnosing piles usually involves a physical examination and discussion of symptoms.
- Medical History and Symptoms: The doctor will ask about your symptoms, including bleeding, pain, itching, swelling, and bowel habits.
- Physical Examination: The doctor will visually inspect the anus to check for external piles or prolapsed internal piles.
- Digital Rectal Exam (DRE): The doctor may insert a gloved, lubricated finger into the rectum to feel for internal piles. Internal piles that are not prolapsed are often too soft to be felt but the exam can rule out other issues.
- Anoscopy, Proctoscopy, or Sigmoidoscopy: If symptoms like bleeding are present, or if the doctor suspects internal piles or wants to rule out other causes of bleeding, they may use an instrument to visualize the inside of the rectum or lower colon.
- Anoscope: A short tube inserted a few inches into the anus.
- Proctoscope: A slightly longer tube.
- Sigmoidoscope: A flexible tube used to examine the lower part of the colon (sigmoid colon).
It’s important to seek medical advice for any rectal bleeding, as this symptom can also be caused by other conditions, some of which are more serious.
Treatments for Piles
Treatment for piles depends on their size, severity, and type (internal or external). Treatment approaches range from simple lifestyle changes to medical procedures and surgery.
1. Lifestyle and Home Remedies (Often for mild cases):
- Increase Fiber Intake: Eating a high-fiber diet (fruits, vegetables, whole grains) and considering fiber supplements can soften stools and reduce straining.
- Drink Enough Fluids: Staying well-hydrated helps prevent constipation.
- Avoid Straining: Don’t hold your breath or push hard during bowel movements.
- Don’t Sit Too Long: Avoid prolonged sitting on the toilet.
- Regular Exercise: Helps prevent constipation and improves overall health.
- Sitz Baths: Soaking the anal area in warm water for 15-20 minutes several times a day can relieve pain and itching.
- ** Topical Treatments:** Over-the-counter creams, ointments, pads, or suppositories containing hydrocortisone, witch hazel, or lidocaine can temporarily relieve pain, itching, and swelling.
2. Minimally Invasive Procedures (Often for persistent or larger internal piles):
These are typically performed in a doctor’s office or clinic.
- Rubber Band Ligation: One or two small rubber bands are placed around the base of an internal pile to cut off its circulation. The pile withers and falls off within about a week. This is one of the most common procedures for internal piles.
- Sclerotherapy: A chemical solution is injected into the internal pile to shrink it by scarring.
- Infrared Coagulation: Heat is used to shrink the internal pile by causing scarring.
- External Hemorrhoid Thrombectomy: If a painful blood clot forms in an external pile, an incision can be made under local anesthetic to remove the clot, providing quick relief.
3. Surgical Procedures (For large, severe, or unresponsive piles):
Surgery is typically reserved for large or severe piles, or those that haven’t responded to other treatments.
- Hemorrhoidectomy: Surgical removal of the piles. This is a highly effective procedure but can be associated with significant post-operative pain and a longer recovery period.
- Stapled Hemorrhoidopexy: This procedure uses a stapling device to reposition prolapsed internal piles and reduce their blood supply. It can be less painful than traditional hemorrhoidectomy but has a different set of potential risks and is not suitable for all types of piles.
Prevention is Key: Lowering Your Risk of Piles
While piles can be a recurring issue for some, adopting preventive measures can significantly reduce your risk of developing them or experiencing flare-ups.
Preventive Strategies to Incorporate into Your Lifestyle: