Rare Birth Defects: What Families Need to Know About Encephalocele and CNS Development
The journey of human development, from a single cell to a fully formed infant, is nothing short of a biological miracle. In most cases, this intricate process unfolds flawlessly. Sometimes, however, there are interruptions in this delicate sequence. One such rare and complex condition is an encephalocele. As we delve into this topic, it’s our goal to provide a clear, comprehensive, and informational overview of this neural tube defect. We will explore what it is, its underlying causes, the symptoms to look for, and the modern medical approaches used for diagnosis and treatment.
What Exactly Is an Encephalocele? A Comprehensive Overview
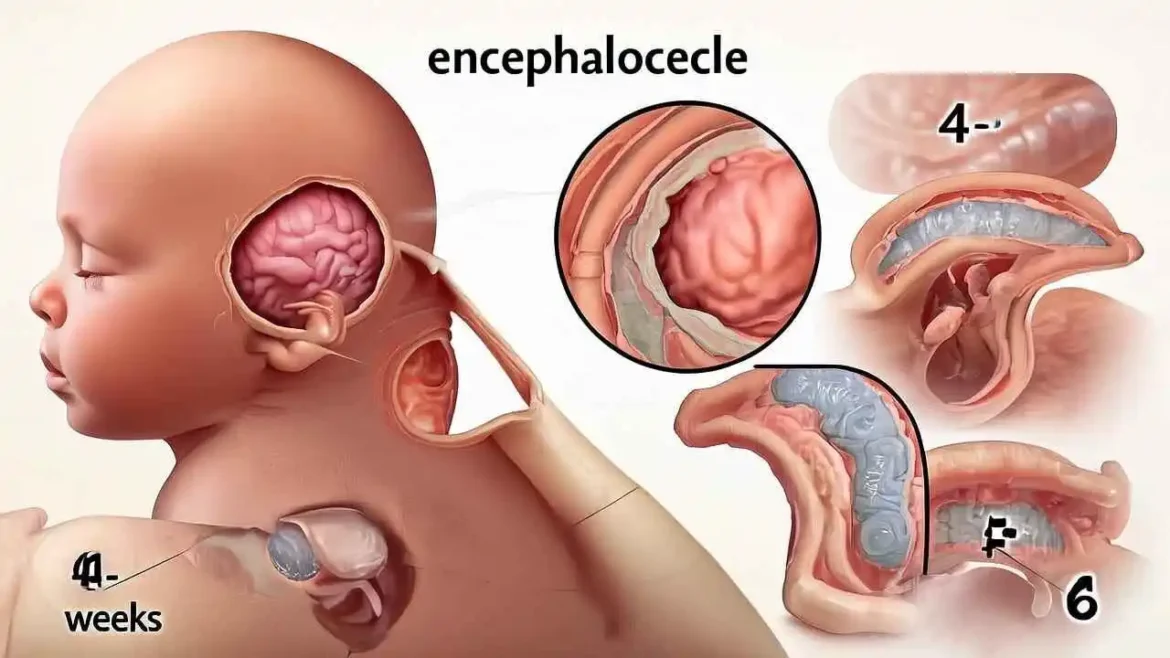
At its core, an encephalocele is a rare and complex type of neural tube defect (NTD). The neural tube is a crucial structure in a developing embryo that eventually forms the brain and spinal cord. It begins as a flat sheet of cells that is supposed to fold and close, much like a zipper, by the third or fourth week of pregnancy to encase the developing central nervous system. When this “zipper” fails to close completely, defects can arise.
An encephalocele is a specific defect where this closure is incomplete, leaving an opening in the skull. Through this abnormal opening, brain tissue, along with the protective membranes that cover it (meninges) and cerebrospinal fluid (CSF), protrudes, forming a sac-like bulge. This sac is most often found on the back of the head (the occipital region) but can occur anywhere along the midline of the skull, including the top (parietal), front (frontal), or even between the forehead and nose (nasofrontal).
The severity of the condition depends heavily on the size and location of the opening and, most importantly, the amount and type of brain tissue contained within the sac.
Classifying Encephaloceles: Location and Content
To better understand the prognosis and treatment, encephaloceles are classified by two main criteria:
- By Location:
- Occipital: The most common type, located on the back of the skull. These are often associated with vision problems and hydrocephalus (an accumulation of fluid in the brain).
- Frontoethmoidal: Occurring at the front of the skull, near the forehead and nose. These are more common in Southeast Asia and can affect the face, eyes, and respiratory passages.
- Parietal: Located on the upper back part of the skull, between the frontal and occipital regions.
- Nasal: A rare type where the protrusion occurs through the nose.
- By Content:
- Meningocele: The sac contains only meninges and cerebrospinal fluid. Brain tissue remains inside the skull. This is a less severe form with a generally better prognosis, as vital brain tissue is not displaced.
- Meningoencephalocele (or Encephalocele): The sac contains brain tissue in addition to the meninges and CSF. This is the more common and more severe form, as the displaced brain tissue is often non-functional and its absence from the skull can lead to significant neurological issues.
Causes and Risk Factors
The exact cause of an encephalocele is often unknown, but it is believed to be multifactorial, resulting from a combination of genetic and environmental factors. A key risk factor for all neural tube defects is a deficiency in folic acid (a B vitamin) before and during the very early stages of pregnancy. Other potential risk factors may include certain medications, maternal infections, or exposure to specific environmental toxins, though these links are less defined.
Diagnosis: Before and After Birth
Encephaloceles are often diagnosed before birth during routine prenatal screenings:
- Prenatal Ultrasound: A detailed ultrasound can reveal the sac-like protrusion from the skull.
- Maternal Blood Tests: Elevated levels of alpha-fetoprotein (AFP) in the mother’s blood can indicate a neural tube defect.
- Fetal MRI: If an encephalocele is suspected, a fetal MRI can provide a more detailed image of the sac’s contents, helping doctors determine how much brain tissue is involved.
If not detected prenatally, the encephalocele is immediately apparent at birth as a visible sac on the infant’s head. Postnatal MRI or CT scans are then used to assess the defect in detail.
Treatment: The Surgical Approach
The primary treatment for an encephalocele is surgery, typically performed within the first few months of life. The goals of the surgery are to:
- Gently place the viable protruding brain tissue back into the skull.
- Excise the non-functional tissue and the sac.
- Repair the opening in the skull with a bone or synthetic graft to protect the brain.
This complex procedure requires a multidisciplinary team, including a pediatric neurosurgeon and a craniofacial plastic surgeon.
Prognosis and Long-Term Outlook
The long-term outlook for a child with an encephalocele is highly variable and depends on several critical factors:
- The presence of brain tissue in the sac: This is the most significant factor. If little or no brain tissue is involved (a meningocele), the child may have a normal life with few or no complications.
- Location of the encephalocele: Occipital encephaloceles, for example, are often linked to more severe neurological deficits.
- Associated conditions: Many children with encephaloceles also develop hydrocephalus, which requires the surgical placement of a shunt to drain excess fluid. Other potential challenges include developmental delays, intellectual disabilities, seizures, vision problems, and issues with motor coordination.
Even with successful surgery, children often require ongoing support from physical therapists, occupational therapists, and speech-language pathologists to reach their full potential. While an encephalocele presents a serious medical challenge, early diagnosis and advanced surgical intervention have significantly improved the outcomes for many affected children.
Classifying Encephaloceles by Location
The location of the skull defect is the primary way we classify encephaloceles. Each type can present unique challenges and is associated with different outcomes.
| Type of Encephalocele | Location on the Skull | Prevalence & Notes |
| Occipital | At the back of the head. | This is the most common type in Western countries, accounting for approximately 75% of cases. |
| Frontoethmoidal | At the front of the head, near the forehead and nose. | More common in Southeast Asia. This type can be external or internal (nasal encephalocele), sometimes causing breathing difficulties. |
| Parietal | On the top or upper side of the head. | A less common location, often associated with other craniofacial abnormalities. |
| Basal | At the base of the skull, often protruding into the nose or throat. | These are not visible externally and can be challenging to diagnose. They may present with respiratory issues or meningitis. |
A Deeper Look: Classifying Encephaloceles by Location
An encephalocele is a rare type of neural tube defect characterized by the protrusion of brain tissue and meninges (the membranes covering the brain) through a congenital opening in the skull. The location of this skull defect is the primary way we classify these conditions, as it profoundly influences the clinical presentation, associated health risks, surgical approach, and overall prognosis for the patient. Each type presents a unique set of challenges for diagnosis and treatment.
A detailed breakdown of the main types of encephaloceles based on their anatomical location.
1. Occipital Encephalocele
- Location on the Skull: At the posterior aspect of the head, originating from a defect in the occipital bone.
- Prevalence & Notes: This is, by a significant margin, the most common type of encephalocele diagnosed in Western countries (North America and Europe), accounting for approximately 75-80% of all cases. The sac can vary dramatically in size, from a small, subtle lump to a large protrusion containing a significant portion of the brain’s occipital and cerebellar lobes. The contents of the sac are critical for prognosis; if it contains only cerebrospinal fluid and meninges (a meningocele), the outcome is generally more favorable. However, if substantial brain tissue has herniated (a meningoencephalocele), there is a higher risk of neurological deficits, including developmental delays, intellectual disability, hydrocephalus (fluid buildup in the brain), and vision problems, as the occipital lobes are the brain’s primary visual processing centers.
2. Frontoethmoidal (or Sincipital) Encephalocele
- Location on the Skull: At the front of the head, involving a defect at the junction of the frontal and ethmoid bones, near the forehead and the root of the nose.
- Prevalence & Notes: While less common in the West, this type is significantly more prevalent in Southeast Asia. Frontoethmoidal encephaloceles are often visible as a mass on the face, which can cause significant craniofacial deformities. They are sub-classified based on their exact point of exit:
- Nasofrontal: Exits between the frontal and nasal bones, appearing as a mass at the bridge of the nose.
- Nasoethmoidal: Exits through the front of the ethmoid bone, presenting as a mass on the side of the nose.
- Naso-orbital: Exits into the orbit (eye socket), potentially displacing the eyeball. This type can be entirely external or have an internal component, known as a nasal encephalocele. In these cases, the protruding tissue extends into the nasal cavity, where it can be mistaken for a nasal polyp. This can lead to persistent nasal obstruction, causing significant breathing difficulties, especially in infants.
3. Parietal Encephalocele
- Location on the Skull: On the top (superior) or upper side (lateral) of the head, arising from a defect in one of the parietal bones.
- Prevalence & Notes: Parietal encephaloceles are a much less common location. They are often associated with a higher incidence of other severe craniofacial and neurological abnormalities. These can include hydrocephalus, agenesis of the corpus callosum (the absence of the brain structure that connects the two cerebral hemispheres), and other syndromes like Dandy-Walker malformation. The prognosis for a parietal encephalocele is often more dependent on the severity of these co-occurring conditions than on the encephalocele itself. Surgical repair can also be complex due to the location and the vital brain structures that may be involved.
4. Basal (or Sphenoidal) Encephalocele
- Location on the Skull: At the base of the skull, with the defect occurring in the sphenoid or ethmoid bones deep within the head. The brain tissue protrudes downwards into the cavities of the head.
- Prevalence & Notes: These are among the rarest and most difficult encephaloceles to diagnose because they are not visible externally. The protrusion extends into the nasopharynx (the area behind the nose), the pharynx (throat), or the sphenoid sinus. Because of their hidden nature, they may not be discovered until a child presents with otherwise unexplained symptoms, such as:
- Persistent respiratory issues or sleep apnea from the mass obstructing the airway.
- Recurrent episodes of meningitis, as the defect creates a direct pathway for bacteria from the nasal passages to the brain.
- Cerebrospinal fluid (CSF) rhinorrhea (leaking of clear, watery fluid from the nose).
- Endocrine or vision problems if the encephalocele affects the pituitary gland or optic nerves. Diagnosis requires a high degree of clinical suspicion and is confirmed with advanced imaging like CT or MRI scans. Surgical correction is essential to prevent life-threatening meningitis and is typically performed via a transnasal or craniofacial approach.
Delving Deeper: The Complex Origins and Risk Factors of Encephalocele
The development of an encephalocele, a type of neural tube defect (NTD), is a complex event that medical science is still working to fully understand. The prevailing understanding is that its origin is multifactorial, meaning it doesn’t arise from a single, isolated cause. Instead, it is believed to result from a sophisticated and delicate interplay between a person’s genetic makeup and various environmental exposures or maternal health conditions. Rather than pointing to one specific trigger, we look at a combination of influences that can collectively increase the risk of the neural tube failing to close completely during the crucial first few weeks of embryonic development.
A more detailed breakdown of the key risk factors that have been identified through extensive research.
1. Folic Acid Deficiency