What Causes Insulin Resistance? Diet, Stress & Hidden Triggers
In the intricate symphony of human physiology, few hormones play as central a role as insulin. Often likened to a key, insulin unlocks the body’s cells, allowing glucose from the bloodstream to enter and serve as vital energy. This process is fundamental to life. However, when this elegant mechanism falters, a condition known as insulin resistance emerges, silently setting the stage for some of the most pervasive and debilitating chronic diseases of our time: type 2 diabetes, heart disease, fatty liver disease, polycystic ovary syndrome (PCOS), and even certain cancers. Insulin resistance is not merely a biochemical anomaly; it is a metabolic state that profoundly impacts energy levels, weight management, cognitive function, and overall vitality. Understanding this condition, recognizing its subtle signs, and harnessing the power of natural remedies and lifestyle changes offer a powerful path towards reclaiming metabolic health and preventing disease progression. This comprehensive guide delves deep into the nature of insulin resistance, explores the science behind natural interventions, and provides actionable strategies to restore insulin sensitivity and foster long-term well-being.
Understanding Insulin Resistance: The Metabolic Crossroads
To grasp insulin resistance, we must first appreciate the normal function of insulin. After you eat, particularly carbohydrates, your digestive system breaks them down into glucose, which enters your bloodstream. The rise in blood glucose signals the beta cells in your pancreas to release insulin. Insulin travels throughout your body and acts primarily in three key ways:
- Facilitates Glucose Uptake: Insulin binds to receptors on the surface of muscle, fat, and liver cells. This binding triggers a cascade of events inside the cell, causing specialized glucose transporters (GLUT4) to move from the cell’s interior to its surface. These transporters act like doors, allowing glucose to move from the blood into the cell where it can be used for energy production or stored for later use (as glycogen in muscles and liver, or as fat in adipose tissue).
- Inhibits Glucose Production: Insulin signals the liver to stop producing and releasing its own glucose (a process called gluconeogenesis) when blood levels are already sufficient.
- Promotes Fat Storage: Insulin encourages the conversion of excess glucose into fatty acids and their storage as triglycerides in fat cells (adipocytes). It also inhibits the breakdown of stored fat (lipolysis).
Insulin resistance occurs when the body’s cells – primarily muscle, fat, and liver cells – become less responsive or “resistant” to the effects of insulin. It’s like the locks on the cell doors (the insulin receptors) become rusty or the keys (insulin) don’t fit as well. To overcome this resistance and maintain normal blood glucose levels, the pancreas compensates by producing and releasing more insulin. This state of elevated insulin levels in the blood is called hyperinsulinemia.
Initially, this compensatory hyperinsulinemia is often effective enough to keep blood glucose levels within the normal range. This phase, where blood sugar is normal but insulin levels are high, is a critical window of opportunity for intervention. However, insulin resistance is often progressive. Over time, the beta cells in the pancreas can become exhausted from the constant demand for excessive insulin production. When they can no longer secrete enough insulin to overcome the resistance, blood glucose levels begin to rise. This marks the transition from insulin resistance with normal blood sugar to prediabetes (elevated blood sugar not yet in the diabetic range) and eventually, if unchecked, to type 2 diabetes (persistently high blood glucose levels).
The development of insulin resistance is complex and multifactorial, involving a interplay of genetic predisposition, lifestyle factors, and environmental influences:
- Excess Body Fat, Particularly Visceral Fat: Fat stored deep within the abdomen, surrounding organs (visceral fat), is highly metabolically active. It releases inflammatory chemicals (cytokines like TNF-alpha and IL-6) and free fatty acids directly into the portal vein leading to the liver. These substances directly interfere with insulin signaling pathways in liver and muscle cells, promoting resistance. Subcutaneous fat (under the skin) is less harmful, but excess overall fat still contributes.
- Physical Inactivity: Muscle is a primary site for glucose disposal. When muscles are inactive, they become less efficient at taking up glucose, even in the presence of insulin. Regular exercise makes muscle cells more sensitive to insulin.
- Dietary Factors: Diets high in refined carbohydrates (white bread, pastries, sugary cereals), added sugars (especially fructose from sugary drinks and processed foods), and unhealthy fats (trans fats, excessive saturated fats) contribute significantly. These foods cause rapid spikes in blood glucose and insulin, promoting inflammation and fat storage, while often lacking the fiber and nutrients that support insulin sensitivity.
- Chronic Stress: The stress hormone cortisol plays a complex role. While essential for acute stress response, chronically elevated cortisol levels (due to persistent work pressure, financial worries, relationship issues, etc.) promote visceral fat deposition, increase blood glucose levels (by stimulating gluconeogenesis), and directly interfere with insulin signaling.
- Inadequate Sleep: Sleep deprivation disrupts the delicate balance of key metabolic hormones. It increases levels of ghrelin (the hunger hormone), decreases levels of leptin (the satiety hormone), raises cortisol, and directly impairs insulin sensitivity the next day. Even one night of poor sleep can induce transient insulin resistance.
- Genetics: Family history plays a role. Some individuals have a genetic predisposition that makes them more susceptible to developing insulin resistance, especially when combined with lifestyle risk factors.
- Aging: Insulin sensitivity tends to naturally decrease with age, partly due to loss of muscle mass (sarcopenia) and changes in body composition (increased fat mass).
- Certain Medications: Corticosteroids, some antipsychotics, and certain medications for high blood pressure can contribute to insulin resistance as a side effect.
- Inflammation: Chronic low-grade systemic inflammation, driven by factors like poor diet, excess visceral fat, stress, and lack of sleep, is both a cause and consequence of insulin resistance. Inflammatory molecules directly disrupt insulin signaling pathways.
The Silent Signs and Far-Reaching Consequences
Insulin resistance often develops silently over years, frequently without obvious symptoms until blood sugar levels rise significantly. However, paying attention to subtle clues can lead to earlier detection and intervention:
- Fatigue and Energy Slumps: Particularly after meals high in carbohydrates, as cells struggle to utilize glucose efficiently for energy.
- Difficulty Concentrating (Brain Fog): The brain relies heavily on glucose. Fluctuations in blood sugar and insulin can impair cognitive function.
- Increased Hunger and Cravings: Especially for sugary or starchy foods, as cells aren’t getting the energy they need, signaling the brain to seek more fuel.
- Weight Gain, Especially Around the Abdomen: Hyperinsulinemia promotes fat storage, particularly visceral fat. Difficulty losing weight despite dieting efforts is common.
- Skin Changes: Dark, velvety patches of skin (acanthosis nigricans), often found on the neck, armpits, or groin, are a visible sign of insulin resistance. Skin tags are also more common.
- Frequent Thirst and Urination: Occur later, as blood sugar levels rise significantly (prediabetes/diabetes).
- High Blood Pressure: Insulin resistance is closely linked to hypertension through mechanisms involving sodium retention, sympathetic nervous system activation, and blood vessel dysfunction.
- High Triglycerides and Low HDL Cholesterol: This specific lipid pattern (high triglycerides, low “good” HDL) is a hallmark of insulin resistance and a major cardiovascular risk factor.
- Polycystic Ovary Syndrome (PCOS): Insulin resistance is a central driver of PCOS in many women, contributing to hormonal imbalances (high androgens), irregular periods, infertility, and ovarian cysts.
The consequences of unmanaged insulin resistance extend far beyond elevated blood sugar:
- Type 2 Diabetes: The most direct consequence. Persistent hyperglycemia damages blood vessels, nerves, eyes, kidneys, and increases infection risk.
- Cardiovascular Disease: Insulin resistance is a major independent risk factor for heart attack and stroke. It contributes to atherosclerosis (plaque buildup in arteries), hypertension, dyslipidemia (unhealthy cholesterol/triglycerides), and inflammation.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Excess fat builds up in the liver due to insulin-driven fat synthesis and impaired fat breakdown. This can progress to inflammation (NASH), fibrosis, cirrhosis, and liver failure.
- Neurodegenerative Diseases: Insulin resistance in the brain (sometimes termed “Type 3 Diabetes”) is increasingly linked to an increased risk of Alzheimer’s disease and other forms of dementia. Inflammation and impaired glucose metabolism harm brain cells.
- Certain Cancers: Hyperinsulinemia and chronic inflammation create an environment conducive to cancer development and progression. Strong links exist to cancers of the colon, breast (postmenopausal), endometrium, pancreas, and liver.
- Kidney Disease: Diabetes and hypertension, both driven by insulin resistance, are the leading causes of chronic kidney disease.
- Infertility and Reproductive Issues: As seen in PCOS, and potentially impacting male fertility through effects on testosterone and sperm quality.
- Accelerated Aging: Metabolic dysfunction, inflammation, and oxidative stress associated with insulin resistance contribute to cellular aging processes.
Recognizing insulin resistance early and taking decisive action through natural, lifestyle-centered approaches is paramount to halting this progression and preventing these devastating outcomes.
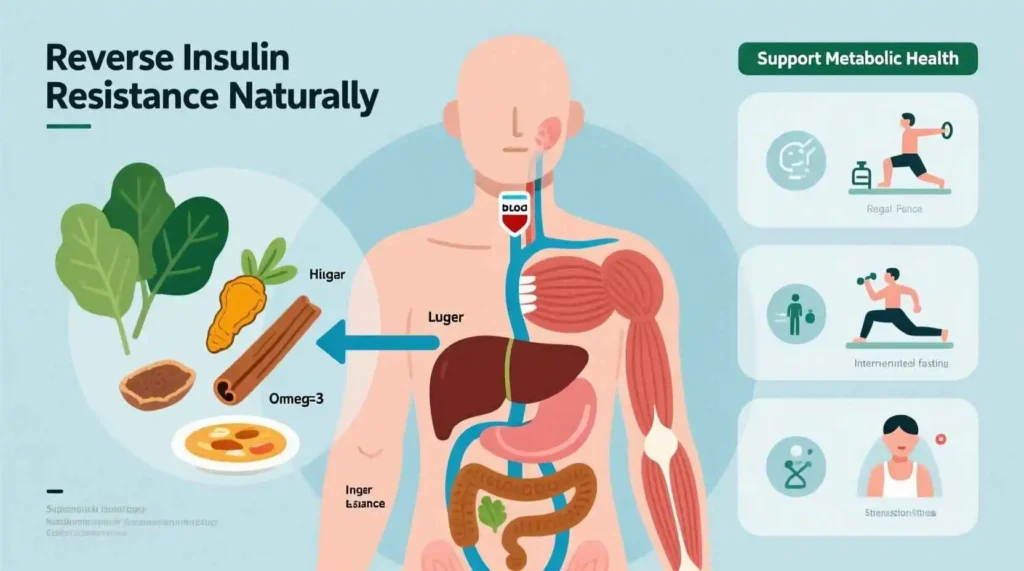
Harnessing Nature’s Pharmacy: Evidence-Based Natural Remedies
While lifestyle changes form the bedrock of managing insulin resistance, certain natural compounds and remedies have demonstrated promising effects in supporting insulin sensitivity and metabolic health. It’s crucial to understand that “natural” does not automatically mean “safe for everyone” or “a substitute for medical care.” Always consult with a healthcare professional before starting any new supplement, especially if you have underlying health conditions or take medications.
- Berberine:
- What it is: A bioactive compound extracted from several plants, including goldenseal, barberry, Oregon grape, and tree turmeric. It has a long history in traditional Chinese and Ayurvedic medicine.
- Mechanism: Berberine has been extensively studied for its effects on metabolism. It activates an enzyme inside cells called AMP-activated protein kinase (AMPK). Often called a “metabolic master switch,” AMPK plays a crucial role in regulating energy metabolism. Activating AMPK:
- Increases glucose uptake in muscle cells (similar to exercise).
- Improves insulin sensitivity.
- Decreases glucose production by the liver.
- Enhances fat burning (lipolysis) and reduces fat storage (lipogenesis).
- Modulates gut microbiota composition.
- Evidence: Numerous clinical trials show berberine can significantly lower fasting blood glucose, HbA1c (a marker of long-term blood sugar control), insulin levels, LDL cholesterol, and triglycerides in individuals with type 2 diabetes and metabolic syndrome. Some studies suggest its efficacy for blood sugar control is comparable to the common diabetes drug metformin, though often with milder gastrointestinal side effects.
- Considerations: Can cause gastrointestinal upset (cramping, diarrhea, gas), especially when starting. Taking it with meals may help. Can interact with many medications (e.g., blood thinners, antidepressants, certain antibiotics, statins). Dosing typically ranges from 900mg to 1500mg per day, divided into 2-3 doses. Professional guidance is essential.
- Cinnamon:
- What it is: A common spice derived from the bark of Cinnamomum trees. Cassia cinnamon is the most common type found in supermarkets; Ceylon cinnamon (“true” cinnamon) is often preferred for supplements due to lower levels of coumarin (a compound that can be harmful to the liver in large doses).
- Mechanism: Cinnamon contains bioactive compounds, particularly cinnamaldehyde and procyanidins, which are thought to:
- Mimic insulin effects and enhance insulin signaling pathways.
- Increase glucose uptake by cells.
- Slow the emptying of the stomach after meals, reducing post-meal blood sugar spikes.
- Possess antioxidant and anti-inflammatory properties.
- Evidence: Research on cinnamon’s effects is somewhat mixed, but several meta-analyses of clinical trials indicate modest but significant benefits. It may help lower fasting blood glucose, HbA1c, and improve insulin sensitivity, particularly in individuals with prediabetes or poorly controlled type 2 diabetes. Effects are generally more pronounced at higher doses (1-6 grams per day) than typical culinary use.
- Considerations: Generally safe when used as a spice. High-dose supplements (especially Cassia cinnamon) carry a risk of liver toxicity due to coumarin; Ceylon cinnamon is safer for supplementation. Can interact with blood thinners and diabetes medications (risk of hypoglycemia). Adding 1-2 teaspoons to food daily is a safe culinary approach.
- Alpha-Lipoic Acid (ALA):
- What it is: A powerful antioxidant compound naturally produced in the body and found in small amounts in foods like spinach, broccoli, and organ meats. It exists in R-ALA (natural form) and S-ALA (synthetic form); R-ALA is considered more bioactive.
- Mechanism: ALA’s primary benefits for insulin resistance stem from its potent antioxidant properties and its unique ability to function in both water-soluble and fat-soluble environments. It:
- Reduces oxidative stress, a key contributor to insulin resistance.
- Enhances glucose uptake into muscle cells by stimulating GLUT4 translocation (similar to insulin and exercise).
- May improve insulin signaling.
- Has shown benefits for diabetic neuropathy (nerve damage).
- Evidence: Clinical studies, particularly using intravenous ALA, show significant improvements in insulin sensitivity in individuals with type 2 diabetes. Oral supplementation (600-1200 mg/day) has also demonstrated benefits for reducing insulin resistance and symptoms of diabetic neuropathy.
- Considerations: Generally well-tolerated. High doses may cause nausea or stomach upset. Can potentially lower blood sugar too much if combined with diabetes medication. May interact with thyroid medications or chemotherapy drugs. R-ALA is often preferred for supplements.
- Magnesium:
- What it is: An essential mineral involved in over 300 enzymatic reactions in the body, including glucose metabolism and insulin signaling. It is abundant in leafy greens, nuts, seeds, legumes, and whole grains.
- Mechanism: Magnesium is crucial for insulin action. It:
- Acts as a cofactor for enzymes involved in glucose utilization.
- Influences insulin receptor activity and tyrosine kinase activity (key steps in insulin signaling).
- Helps regulate intracellular calcium levels; imbalances can impair insulin secretion and action.
- Deficiency is strongly linked to insulin resistance and increased risk of type 2 diabetes.
- Evidence: Numerous observational studies show an inverse relationship between magnesium intake/status and insulin resistance/diabetes risk. Intervention studies supplementing magnesium (often magnesium glycinate, citrate, or chloride, 200-400 mg elemental magnesium/day) in individuals with deficiency or prediabetes/diabetes show improvements in insulin sensitivity, fasting glucose, and HbA1c.
- Considerations: Dietary sources are best first. Supplements can cause diarrhea (especially magnesium oxide); glycinate or citrate are better absorbed and less likely to cause GI issues. Individuals with kidney disease should not supplement without medical supervision.
- Omega-3 Fatty Acids (EPA & DHA):
- What it is: Essential polyunsaturated fats primarily found in fatty fish (salmon, mackerel, sardines, herring), fish oil, and algae oil. Eicosapentaenoic acid (EPA) and Docosahexaenoic acid (DHA) are the most biologically active forms.
- Mechanism: Omega-3s exert multiple beneficial effects:
- Potent Anti-inflammatory Action: They reduce the production of pro-inflammatory cytokines (like TNF-alpha, IL-6) that drive insulin resistance.
- Improved Cell Membrane Fluidity: Incorporating omega-3s into cell membranes enhances the function of insulin receptors and glucose transporters.
- Reduced Liver Fat: Help decrease fat accumulation in the liver (NAFLD), improving hepatic insulin sensitivity.
- Improved Lipid Profile: Lower triglycerides, raise HDL cholesterol.
- Evidence: Studies show omega-3 supplementation (typically 1-4 grams of combined EPA+DHA per day) can improve insulin sensitivity, particularly in individuals with existing insulin resistance, type 2 diabetes, or NAFLD. Effects on blood sugar control can be modest but significant, especially for reducing triglycerides and inflammation.
- Considerations: Generally safe. High doses (>3g/day) may increase bleeding risk (caution with blood thinners). Choose reputable brands tested for purity (heavy metals, PCBs). Dietary intake of fatty fish is highly recommended.
- Chromium:
- What it is: An essential trace mineral found in small amounts in foods like broccoli, potatoes, whole grains, meat, and nuts. Chromium picolinate is a common supplemental form.
- Mechanism: Chromium is thought to enhance insulin action by:
- Potentiating the signaling pathway of insulin, potentially increasing the number of insulin receptors or their sensitivity.
- Aiding in the movement of glucose transporters (GLUT4) to the cell membrane.
- Evidence: Research on chromium is mixed. Some studies, particularly in individuals with chromium deficiency or poorly controlled diabetes, show modest improvements in fasting glucose, HbA1c, and insulin sensitivity. Other studies show no significant benefit. Effects appear more pronounced in those with deficiency or significant insulin resistance.
- Considerations: Generally safe at recommended doses (200-1000 mcg/day). High doses can cause kidney damage or other issues. Picolinate form may have better absorption but theoretical concerns about DNA damage at very high doses; other forms (like nicotinate or histidinate) are alternatives. Not universally effective; benefits may be limited to deficient individuals.
- Fenugreek:
- What it is: An herb commonly used as a spice (seeds) in Indian cuisine and in traditional medicine. Its seeds are rich in soluble fiber (galactomannan) and steroid saponins.
- Mechanism: Fenugreek’s benefits likely stem from:
- High Soluble Fiber Content: Slows gastric emptying and carbohydrate digestion/absorption, blunting post-meal blood sugar spikes.
- Saponins: May stimulate insulin secretion and improve insulin sensitivity.
- 4-Hydroxyisoleucine (an amino acid): Shown to stimulate insulin secretion.
- Evidence: Clinical trials consistently show fenugreek supplementation (typically 5-100 grams of defatted seed powder or 1-2 grams of extract per day) significantly lowers fasting and post-meal blood glucose levels and improves glucose tolerance in individuals with type 2 diabetes and prediabetes. Effects on insulin sensitivity are also observed.
- Considerations: Generally safe. Can cause gastrointestinal upset (gas, diarrhea), especially at higher doses. Maple syrup odor in urine/sweat is harmless. May interact with blood thinners and diabetes medications. Culinary use is safe; start supplements cautiously.
- Probiotics and Prebiotics:
- What they are: Probiotics are beneficial live bacteria (e.g., Lactobacillus, Bifidobacterium strains) found in fermented foods (yogurt, kefir, sauerkraut, kimchi) and supplements. Prebiotics are types of fiber (e.g., inulin, FOS, GOS) that feed these beneficial bacteria, found in foods like onions, garlic, leeks, asparagus, bananas, and whole grains.
- Mechanism: The gut microbiome plays a crucial role in metabolism:
- Short-Chain Fatty Acid (SCFA) Production: Gut bacteria ferment prebiotic fibers to produce SCFAs (like butyrate, propionate, acetate). SCFAs enhance insulin sensitivity in muscle and liver, stimulate gut hormones (GLP-1, PYY) that improve insulin secretion and satiety, and reduce inflammation.
- Reduced Endotoxemia: A healthy gut barrier prevents bacterial endotoxins (like LPS) from entering the bloodstream. Dysbiosis (imbalanced gut flora) increases gut permeability (“leaky gut”), allowing LPS into circulation, triggering inflammation and insulin resistance. Probiotics/prebiotics support gut barrier integrity.
- Modulation of Bile Acid Metabolism: Gut bacteria influence bile acid signaling, which impacts glucose and lipid metabolism.
- Evidence: Growing research shows that specific probiotic strains (e.g., Lactobacillus acidophilus, Lactobacillus casei, Bifidobacterium bifidum) and prebiotic fibers can improve insulin sensitivity, reduce inflammation, lower HbA1c, and improve lipid profiles in individuals with metabolic syndrome, prediabetes, and type 2 diabetes. Multi-strain probiotics and synbiotics (combinations of pro- and prebiotics) often show the most promise.
- Considerations: Generally safe. Effects are strain-specific and dose-dependent. Start with fermented foods. Supplements vary widely in quality and viability. May cause temporary gas/bloating initially. Individuals with severe immune compromise should consult a doctor.
- Resveratrol:
- What it is: A polyphenol antioxidant found in red grapes, red wine, berries, peanuts, and Japanese knotweed. It gained fame for its potential role in the “French Paradox.”
- Mechanism: Resveratrol activates sirtuins, particularly SIRT1, a protein involved in regulating cellular metabolism, stress resistance, and aging. It:
- Enhances insulin signaling pathways.
- Improves mitochondrial function (cellular energy production).
- Reduces inflammation and oxidative stress.
- May protect pancreatic beta cells.
- Evidence: Animal studies are very promising. Human clinical trials show more mixed but often positive results, particularly in individuals with type 2 diabetes. Studies indicate improvements in insulin sensitivity, HbA1c, post-meal glucose, and blood pressure. Effects can be modest.
- Considerations: Generally safe. Bioavailability from food/supplements can be low. High doses may interact with blood thinners. Focus on dietary sources (berries, grapes, moderate red wine) or consider standardized extracts if supplementing.
- Vitamin D:
- What it is: A fat-soluble vitamin/hormone synthesized in the skin upon sun exposure and found in fatty fish, fortified milk, and supplements.
- Mechanism: Vitamin D receptors are present in insulin-producing beta cells and insulin-responsive tissues (muscle, fat, liver). Vitamin D:
- Influences insulin secretion from beta cells.
- Modulates insulin sensitivity in peripheral tissues.
- Regulates calcium flux, which is important for insulin-mediated intracellular processes.
- Has anti-inflammatory effects.
- Evidence: Strong observational data links low vitamin D status to increased risk of insulin resistance, prediabetes, and type 2 diabetes. Intervention studies supplementing vitamin D in deficient individuals show improvements in insulin sensitivity, beta-cell function, and sometimes HbA1c, particularly in those with significant deficiency or poor glycemic control. Effects in sufficient individuals are less clear.
- Considerations: Get levels tested if deficiency is suspected. Supplementation is crucial for deficient individuals (dosage depends on level and individual factors). Excessive intake can be toxic. Safe sun exposure and dietary sources are important.
The Cornerstone of Reversal: Transformative Lifestyle Changes
While natural remedies can provide valuable support, the most powerful and sustainable approach to reversing insulin resistance lies in comprehensive lifestyle modifications. These changes address the root causes of the condition – excess visceral fat, inactivity, poor diet, stress, and poor sleep. Implementing these strategies consistently can dramatically improve insulin sensitivity, often leading to weight loss, normalized blood sugar, and reduced risk of complications.
1. Dietary Revolution: Eating for Insulin Sensitivity
Diet is arguably the most impactful lever for improving insulin sensitivity. The goal is to stabilize blood sugar levels, reduce inflammation, promote weight loss (especially visceral fat), and provide essential nutrients.
- Prioritize Whole, Unprocessed Foods: Base your diet on foods as close to their natural state as possible. This means vegetables, fruits, whole grains, legumes, nuts, seeds, lean proteins, and healthy fats. Minimize or eliminate ultra-processed foods, which are often high in refined carbs, added sugars, unhealthy fats, sodium, and low in fiber and nutrients.
- Embrace Low Glycemic Load Carbohydrates: Focus on carbohydrates that are digested and absorbed slowly, causing gradual rises in blood sugar and insulin.
- Non-Starchy Vegetables: Abundantly! Leafy greens (spinach, kale, arugula), broccoli, cauliflower, peppers, mushrooms, asparagus, zucchini, tomatoes, cucumbers. They are low in carbs/calories but high in fiber, vitamins, minerals, and antioxidants. Aim to fill half your plate with non-starchy veggies.
- Legumes: Beans, lentils, chickpeas. Excellent sources of plant-based protein, soluble fiber, and complex carbs. They have a very low glycemic impact.
- Whole Grains (Intact): Oats (steel-cut or rolled, not instant), quinoa, brown rice, wild rice, barley, farro, buckwheat. Choose intact grains over flours whenever possible. They provide sustained energy and fiber.
- Low-Sugar Fruits: Berries (strawberries, blueberries, raspberries), cherries, apples, pears, citrus fruits. Consume in moderation (1-2 servings per day), paired with protein or fat to blunt blood sugar spikes.
- Drastically Reduce Added Sugars and Refined Carbohydrates: This is critical.
- Eliminate Sugary Drinks: Soda, fruit juice (even 100%), sweetened teas/coffees, sports drinks, energy drinks. These are liquid sugar bombs causing rapid insulin spikes.
- Avoid Refined Grains: White bread, white rice, regular pasta, pastries, cookies, cakes, sugary cereals. These are stripped of fiber and nutrients, acting like sugar in the body.
- Read Labels: Added sugars hide everywhere – sauces, dressings, bread, yogurt, granola bars. Look for terms like sucrose, high-fructose corn syrup, dextrose, maltose, cane sugar, etc. Aim for products with minimal or no added sugar.
- Include Adequate Lean Protein at Every Meal: Protein promotes satiety, helps preserve muscle mass during weight loss (muscle is crucial for glucose disposal), and has a minimal impact on blood sugar. Excellent sources include:
- Poultry (chicken, turkey breast)
- Fish (especially fatty fish like salmon, mackerel, sardines)
- Eggs
- Lean cuts of meat (in moderation)
- Tofu, tempeh, edamame
- Legumes (also provide carbs/fiber)
- Low-fat dairy or dairy alternatives (unsweetened)
- Incorporate Healthy Fats: Fat is essential and does not inherently cause insulin resistance. Focus on anti-inflammatory, heart-healthy fats.
- Monounsaturated Fats: Avocados, olive oil, avocado oil, nuts (almonds, walnuts, pistachios, pecans), seeds (pumpkin, sesame).
- Polyunsaturated Fats (Omega-3s): Fatty fish, flaxseeds, chia seeds, walnuts.
- Limit Saturated Fats: Found in fatty red meats, processed meats, full-fat dairy, butter, coconut oil, palm oil. Use in moderation.
- Avoid Trans Fats: Found in partially hydrogenated oils (check labels – banned in many places, but may still be present in some processed foods). Extremely harmful.
- Maximize Fiber Intake: Fiber, especially soluble fiber, is a superstar for insulin resistance.
- Slows Digestion: Blunts post-meal blood sugar and insulin spikes.
- Promotes Satiety: Helps control appetite and calorie intake.
- Feeds Gut Bacteria: Fermented to beneficial SCFAs.
- Binds Bile Acids/Cholesterol: Helps lower LDL cholesterol.
- Aim for 25-40 grams per day: Focus on vegetables, fruits (with skin), legumes, whole grains, nuts, and seeds.
- Consider Meal Timing and Patterns:
- Avoid Constant Snacking: Give your pancreas and insulin levels a break between meals. Aim for 3 main meals and potentially 1-2 small, protein/fiber-rich snacks if needed, rather than grazing all day.
- Time-Restricted Eating (TRE)/Intermittent Fasting (IF): This involves limiting your daily eating window (e.g., eating within an 8-hour window, fasting for 16 hours – 16:8 method). Benefits include:
- Lowered overall insulin levels over the day.
- Improved insulin sensitivity.
- Enhanced cellular repair processes (autophagy).
- Potential for weight loss.
- Note: Not suitable for everyone (e.g., pregnant/breastfeeding women, individuals with a history of eating disorders, those on certain medications). Start gradually (e.g., 12:12) and consult a doctor if unsure. Focus on nutrient density during eating windows.
- Stay Hydrated: Drink plenty of water throughout the day. Sometimes thirst is mistaken for hunger. Herbal teas are also good options. Limit sugary drinks and excessive caffeine.
2. Movement as Medicine: Exercise for Insulin Sensitivity
Physical activity is a potent, non-negotiable tool for combating insulin resistance. It works through multiple mechanisms:
- Immediate Glucose Uptake: Muscle contraction stimulates glucose uptake into muscle cells independently of insulin. This effect lasts for hours after exercise.
- Improved Insulin Sensitivity: Regular exercise makes muscle cells more responsive to insulin, meaning less insulin is needed to move glucose into the cells. It also enhances liver insulin sensitivity.
- Reduced Visceral Fat: Exercise, particularly aerobic exercise, is highly effective at burning visceral fat, reducing the source of inflammatory cytokines.
- Increased Muscle Mass: Strength training builds skeletal muscle. Muscle is the primary site for glucose disposal. More muscle mass means a larger “sink” for glucose, improving overall metabolic health and resting metabolic rate.
- Reduced Inflammation: Exercise has potent anti-inflammatory effects.
Key Exercise Strategies:
- Aerobic Exercise (Cardio):
- Frequency & Duration: Aim for at least 150 minutes of moderate-intensity aerobic activity OR 75 minutes of vigorous-intensity activity per week. Spread throughout the week (e.g., 30 minutes, 5 days/week moderate).
- Moderate Intensity: Brisk walking, cycling on level ground, water aerobics, doubles tennis, hiking (you can talk, but not sing).
- Vigorous Intensity: Running, swimming laps, fast cycling, uphill hiking, singles tennis, high-intensity cardio classes (you can only say a few words without pausing).
- High-Intensity Interval Training (HIIT): Involves short bursts (e.g., 30-60 seconds) of near-maximum effort followed by periods (e.g., 1-2 minutes) of lower-intensity recovery or rest. HIIT is extremely time-efficient and highly effective for improving insulin sensitivity and burning visceral fat. Examples: sprint intervals, cycling intervals, burpees, jump squats. Start with 1 session per week, gradually increasing.
- Strength Training (Resistance Training):
- Frequency: Aim for 2-3 sessions per week, targeting all major muscle groups (legs, back, chest, shoulders, arms, core). Allow at least 48 hours between sessions targeting the same muscle group.
- Methods: Use free weights (dumbbells, barbells), weight machines, resistance bands, or bodyweight exercises (squats, lunges, push-ups, pull-ups, planks).
- Focus: Prioritize compound exercises that work multiple muscle groups simultaneously (e.g., squats, deadlifts, bench press, rows, overhead press) for maximum efficiency and metabolic benefit.
- Progression: Gradually increase the weight, number of repetitions (reps), number of sets, or reduce rest time to keep challenging your muscles and stimulating growth.
- Increase Non-Exercise Activity Thermogenesis (NEAT): This refers to the calories burned during daily activities that are not formal exercise. Boosting NEAT makes a significant difference:
- Take the stairs instead of the elevator.
- Park farther away from entrances.
- Walk or cycle for short errands instead of driving.
- Stand or walk around while talking on the phone.
- Do household chores actively.
- Use a standing desk or take regular standing/walking breaks if you have a desk job.
- Consistency is Paramount: Find activities you genuinely enjoy. This makes it far more likely you’ll stick with exercise long-term. Mix different types to prevent boredom and overuse injuries. Start slowly if you’re new to exercise and gradually increase duration and intensity.
3. Stress Mastery: Calming the Metabolic Storm
Chronic stress is a major driver of insulin resistance through its effects on cortisol. Actively managing stress is essential for metabolic health.
- Mindfulness and Meditation: These practices train the mind to focus on the present moment without judgment. They directly activate the body’s relaxation response (parasympathetic nervous system), counteracting the stress response (sympathetic nervous system) and lowering cortisol levels.
- How to Start: Begin with just 5-10 minutes daily. Use guided meditations (apps like Calm, Headspace, Insight Timer are helpful), focus on your breath, or simply sit quietly and observe your thoughts without getting caught up in them. Consistency is more important than duration.
- Deep Breathing Exercises: Simple techniques can quickly induce relaxation.
- Diaphragmatic (Belly) Breathing: Place one hand on your chest, one on your belly. Inhale slowly and deeply through your nose, allowing your belly to rise (chest should move minimally). Exhale slowly through your mouth, letting your belly fall. Repeat for several minutes.
- Box Breathing: Inhale for 4 counts, hold for 4 counts, exhale for 4 counts, hold for 4 counts. Repeat.
- Regular Physical Activity: As mentioned, exercise is a powerful stress reliever.
- Spending Time in Nature: “Forest bathing” (Shinrin-yoku) or simply spending time in green spaces has proven calming and restorative effects, lowering cortisol and blood pressure.
- Engaging in Hobbies and Relaxation: Make time for activities you find truly relaxing and enjoyable – reading, listening to music, gardening, crafting, spending time with loved ones, playing with pets. This provides a mental break from stressors.
- Yoga and Tai Chi: These mind-body practices combine physical postures, breathing exercises, and meditation, making them excellent tools for stress reduction and improving insulin sensitivity.
- Adequate Downtime and Boundaries: Schedule time for rest and relaxation. Learn to say no to additional commitments when you’re feeling overwhelmed. Protect your personal time.
- Seek Support: Talk to friends, family, or a therapist. Don’t bottle up stress. Professional counseling (e.g., Cognitive Behavioral Therapy – CBT) can be highly effective for managing chronic stress and anxiety.
4. The Power of Sleep: Restoring Metabolic Balance
Sleep is not a luxury; it is a fundamental pillar of metabolic health. Chronic sleep deprivation wreaks havoc on hormones critical for insulin sensitivity.
- Prioritize Duration: Aim for 7-9 hours of quality sleep per night consistently. This is non-negotiable for metabolic health.
- Establish a Consistent Schedule: Go to bed and wake up at roughly the same time every day, even on weekends. This helps regulate your body’s internal clock (circadian rhythm), which influences hormone release, including insulin and cortisol.
- Optimize Your Sleep Environment:
- Dark: Use blackout curtains or an eye mask. Even small amounts of light can suppress melatonin production.
- Quiet: Use earplugs or a white noise machine if needed.
- Cool: A slightly cool room temperature (around 60-67°F or 15-19°C) is generally optimal for sleep.
- Comfortable: Invest in a supportive mattress and pillows.
- Create a Relaxing Wind-Down Routine: Dedicate 30-60 minutes before bed to calm your mind and body. Avoid stimulating activities.
- Avoid Screens: The blue light emitted by phones, tablets, computers, and TVs suppresses melatonin. Stop using screens at least an hour before bed. Read a physical book instead.
- Relaxing Activities: Take a warm bath, listen to calming music, practice gentle stretching or restorative yoga, do some light reading, practice meditation or deep breathing.
- Limit Stimulants:
- Caffeine: Avoid caffeine (coffee, tea, soda, chocolate) in the afternoon and evening. Its effects can last many hours.
- Nicotine: Nicotine is a stimulant that disrupts sleep.
- Alcohol: While alcohol might make you feel drowsy initially, it disrupts sleep architecture later in the night, leading to fragmented, poor-quality sleep. Avoid alcohol close to bedtime.
- Get Morning Sunlight: Exposure to natural light in the morning helps regulate your circadian rhythm, promoting better sleep at night.
- Address Sleep Disorders: If you suspect you have sleep apnea (loud snoring, gasping for air, daytime sleepiness) or another sleep disorder, seek diagnosis and treatment. Untreated sleep apnea is strongly linked to insulin resistance.
5. Weight Management: Focusing on Visceral Fat
While the lifestyle changes above will naturally promote healthy weight loss, focusing specifically on reducing visceral fat is key for reversing insulin resistance.
- Sustainable Calorie Deficit: Weight loss requires consuming fewer calories than you expend. However, extreme restriction is counterproductive and unsustainable. Focus on the nutrient-dense, whole-foods diet described above. The high fiber and protein content naturally promote satiety, making it easier to maintain a modest calorie deficit without constant hunger.
- Prioritize Visceral Fat Loss: The good news is that visceral fat is often the first fat lost when you adopt a healthier lifestyle, particularly with exercise. The dietary and exercise strategies outlined above are specifically targeted at reducing this dangerous fat depot.
- Focus on Health, Not Just the Scale: While weight loss is beneficial, improvements in insulin sensitivity can occur even before significant weight loss is seen, especially with exercise. Pay attention to other markers: waist circumference reduction, increased energy, improved mood, better sleep, and improvements in blood work (fasting glucose, HbA1c, triglycerides, HDL).
- Be Patient and Consistent: Healthy, sustainable weight loss is typically gradual (0.5-2 pounds per week). Focus on building lasting habits rather than quick fixes.
Integrating the Approach: A Synergistic Path to Reversal