Understanding Burns: Types, First Aid, Treatments, and Precautions
Burns are among the most common household injuries, affecting millions of people each year. They can range from minor, superficial wounds to life-threatening emergencies that require immediate medical attention. Understanding burns, the0ir types, appropriate first aid measures, available treatments, and necessary precautions is essential knowledge for everyone, as proper initial response can significantly affect the outcome and healing process. This comprehensive guide explores the various aspects of burns, providing detailed information to help you recognize, respond to, and prevent these painful injuries.
Introduction to Burns
A burn is a type of injury to skin or other tissues caused by heat, cold, electricity, chemicals, friction, or radiation. Most burns are due to heat from hot liquids, solids, or fire. While burns are typically associated with the skin, they can also affect deeper tissues, muscles, bones, and internal organs in severe cases.
The skin is the body’s largest organ and serves as a protective barrier against the environment. When a burn occurs, this barrier is compromised, potentially leading to infection, fluid loss, and other complications. The severity of a burn depends on its depth, size, location, and the age and overall health of the affected individual.
Burn injuries are a significant global health problem, with an estimated 180,000 deaths annually, according to the World Health Organization. The majority of these deaths occur in low- and middle-income countries, where prevention programs and access to care may be limited. In high-income countries, while mortality rates are lower, burns remain a leading cause of disability and disfigurement.
The impact of burns extends beyond physical injury. Survivors often face long-term psychological, social, and economic challenges, including post-traumatic stress disorder, depression, social stigma, and loss of productivity. Understanding burns and their management is crucial not only for healthcare professionals but for the general public, as immediate and appropriate first aid can significantly improve outcomes.
Types of Burns
Burns are classified based on their depth, the cause of the injury, and the extent of tissue damage. Understanding these classifications helps determine the appropriate treatment and predict the potential for complications and scarring.
Classification by Depth
The depth of a burn refers to how deeply it penetrates the skin’s layers. The skin has three main layers: the epidermis (outer layer), the dermis (middle layer), and the subcutaneous tissue (deepest layer). Burns are traditionally classified into four degrees based on depth:
First-Degree Burns: These are superficial burns that affect only the epidermis, the outermost layer of the skin. They cause redness, pain, and minor swelling but do not blister. Common examples include mild sunburn and brief contact with hot objects. First-degree burns typically heal within 3-6 days without scarring.
Second-Degree Burns: These burns extend into the dermis, the second layer of skin. They are characterized by redness, blistering, severe pain, and swelling. Second-degree burns are divided into two categories:
Superficial partial-thickness burns affect the upper part of the dermis. They are painful, blister immediately, and typically heal within 2-3 weeks with minimal scarring.
Deep partial-thickness burns extend deeper into the dermis. They may appear white or yellowish, are less painful due to nerve damage, and take longer to heal (3-8 weeks). These burns often result in scarring and may require skin grafting.
Third-Degree Burns: Also known as full-thickness burns, these extend through the dermis and affect the subcutaneous tissue. The burned area may appear white, blackened, or charred, and the skin may feel leathery or waxy. Surprisingly, these burns may not be painful due to complete destruction of nerve endings. Third-degree burns always require medical attention and typically heal with significant scarring. Skin grafting is usually necessary.
Fourth-Degree Burns: These are the most severe burns, extending through all layers of the skin and into underlying tissues, including muscle, bone, and tendons. The area may appear charred or blackened, and there is typically no sensation in the burned area due to complete nerve destruction. Fourth-degree burns are life-threatening and require immediate, specialized medical care, often including extensive surgery and rehabilitation.
Classification by Cause
Burns can also be classified based on the cause of the injury. Understanding the cause is important as it influences the immediate treatment approach and potential complications:
Thermal Burns: These are the most common type of burn, caused by exposure to heat sources such as fire, hot liquids (scalds), steam, hot objects, and explosions. Thermal burns can range from superficial to deep, depending on the temperature of the heat source and the duration of contact.
Chemical Burns: These result from exposure to strong acids, alkalis, or other corrosive substances. Chemical burns can continue to damage tissue until the chemical is completely removed or neutralized. They can be deceptive, as the initial injury may appear mild but can penetrate deeply over time.
Electrical Burns: These occur when electrical current passes through the body. Electrical burns can cause both external and internal damage, with the internal injury often being more severe than the external appearance suggests. They can affect the heart and other organs and may cause additional complications such as cardiac arrhythmias or neurological damage.
Radiation Burns: These are caused by exposure to various forms of radiation, including ultraviolet (UV) radiation from the sun or tanning beds, X-rays, and radiation therapy for cancer treatment. Radiation burns can range from mild sunburn to severe tissue damage, depending on the type and duration of exposure.
Friction Burns: These occur when the skin rubs against a hard surface, generating heat that causes a burn. Friction burns are a combination of a thermal burn and an abrasion. Common examples include rope burns, carpet burns, and injuries from motorcycle or bicycle accidents.
Cold Burns: Also known as frostbite, these are caused by exposure to extreme cold. Cold burns damage skin and underlying tissues by freezing them. They typically affect exposed areas such as the nose, ears, cheeks, fingers, and toes.
Classification by Extent
The extent of a burn refers to the percentage of the body surface area (BSA) affected. This classification is important for determining fluid resuscitation needs, treatment approach, and prognosis. The “Rule of Nines” is commonly used to estimate BSA in adults:
The head and neck account for 9% of BSA. Each arm accounts for 9% of BSA. The front of the torso accounts for 18% of BSA. The back of the torso accounts for 18% of BSA. Each leg accounts for 18% of BSA. The genital area accounts for 1% of BSA.
For children, the Lund-Browder chart is more accurate as it accounts for the proportional differences in body surface area with age.
Burns are often categorized by extent as:
Minor burns: Less than 10% of BSA in adults or less than 5% in children, with only first- or second-degree burns. Moderate burns: 10-20% of BSA in adults or 5-10% in children, or any third-degree burn less than 2% of BSA. Major burns: More than 20% of BSA in adults or more than 10% in children, or any third-degree burn more than 2% of BSA, or burns involving critical areas such as the face, hands, feet, genitalia, or major joints.
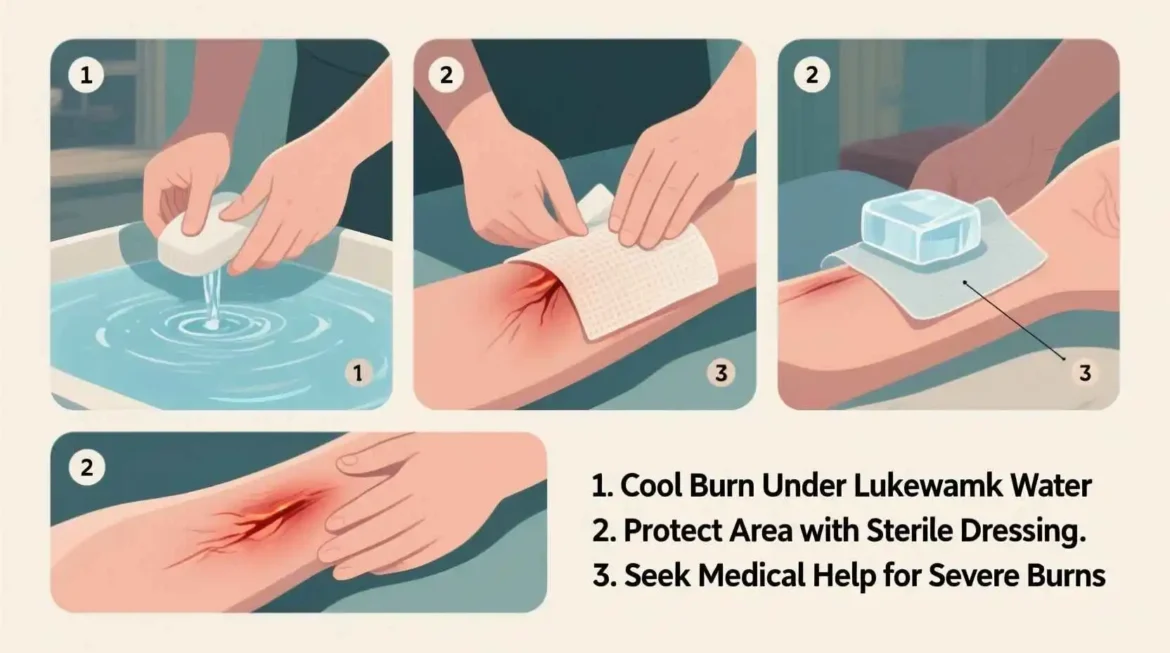
First Aid for Burns
Proper first aid for burns is crucial as it can reduce pain, prevent infection, minimize tissue damage, and improve healing outcomes. The appropriate first aid measures depend on the type and severity of the burn, but some general principles apply to most burn injuries.
Immediate Actions
The first step in managing a burn is to ensure safety for both the victim and the first aider. Remove the person from the source of the burn to prevent further injury. For chemical burns, remove any contaminated clothing, being careful not to spread the chemical to unaffected areas. For electrical burns, ensure the power source is turned off before approaching the victim to avoid electrocution.
Once safety is ensured, assess the burn’s severity. Minor burns can often be treated at home with appropriate first aid, while moderate to severe burns require immediate medical attention. When in doubt, it’s always best to seek professional medical care.
First Aid for Thermal Burns
For thermal burns caused by heat, follow these steps:
Cool the burn: Hold the burned area under cool (not cold) running water for at least 10-20 minutes. This helps dissipate heat, reduce pain, and minimize tissue damage. Avoid using ice or ice water, as extreme cold can cause further tissue injury.
Remove jewelry and tight clothing: Remove any jewelry, watches, or tight clothing from the burned area before swelling begins. Do not attempt to remove anything that is stuck to the burn.
Cover the burn: After cooling, cover the burn with a sterile, non-stick dressing or clean cloth. Avoid using cotton balls or fluffy materials that may leave fibers in the wound.
Manage pain: Over-the-counter pain relievers such as acetaminophen or ibuprofen can help manage pain. Follow the dosage instructions on the package.
Do not break blisters: If blisters form, do not break them, as this increases the risk of infection. If blisters break on their own, clean the area with mild soap and water, apply an antibiotic ointment, and cover with a sterile dressing.
First Aid for Chemical Burns
Chemical burns require special attention as the chemical can continue to damage tissue until it is completely removed. Follow these steps:
Remove contaminated clothing: Carefully remove any clothing or jewelry that has come into contact with the chemical. Wear protective gloves if available to avoid getting the chemical on your own skin.
Brush off dry chemicals: If the chemical is a powder, brush it off the skin before flushing with water.
Flush with water: Rinse the affected area with copious amounts of cool running water for at least 20 minutes. For chemical burns to the eyes, flush continuously for at least 30 minutes, holding the eyelids open to ensure thorough rinsing.
Do not neutralize: Do not attempt to neutralize the chemical with another substance, as this can cause a chemical reaction that generates heat and worsens the burn.
Cover the burn: After thorough flushing, cover the burn with a sterile dressing.
Seek immediate medical attention: All chemical burns should be evaluated by a healthcare professional, as they can be more severe than they initially appear.
First Aid for Electrical Burns
Electrical burns can be particularly dangerous as they can cause both external and internal damage. Follow these steps:
Ensure safety: Before approaching the victim, make sure the power source is turned off or the victim is no longer in contact with the electrical source. Do not touch the victim with your bare hands if they are still in contact with electricity.
Call for emergency help: Electrical burns always require immediate medical attention, even if they appear minor externally.
Check for other injuries: Electrical burns can cause cardiac arrhythmias, respiratory arrest, fractures, and spinal injuries. Be prepared to perform CPR if necessary.
Treat visible burns: Cool any visible burns with cool running water and cover with a sterile dressing.
Monitor the victim: Keep the victim warm and comfortable while waiting for emergency medical services. Monitor their breathing and consciousness.
First Aid for Radiation Burns
Radiation burns, such as sunburn or radiation therapy burns, can be managed with the following steps:
Cool the burn: Apply cool compresses or take a cool bath to soothe the burn and reduce heat.
Moisturize: After cooling, apply a moisturizing lotion or aloe vera gel to soothe the skin and prevent dryness.
Protect from further exposure: Keep the burned area covered and protected from further radiation exposure.
Manage pain: Over-the-counter pain relievers can help manage discomfort.
Avoid popping blisters: If blisters form, leave them intact to prevent infection.
First Aid for Friction Burns
Friction burns combine a thermal burn with an abrasion. First aid includes:
Clean the wound: Gently clean the area with mild soap and water to remove dirt and debris.
Apply antibiotic ointment: After cleaning, apply a thin layer of antibiotic ointment to prevent infection.
Cover the wound: Cover with a sterile non-stick dressing.
Change dressings regularly: Change the dressing daily or whenever it becomes wet or dirty.
Monitor for infection: Watch for signs of infection, such as increased redness, swelling, pain, or pus.
First Aid for Cold Burns (Frostbite)
Cold burns, or frostbite, require careful warming to prevent further tissue damage:
Move to a warm area: Get the person to a warm place as soon as possible.
Remove wet clothing: Replace wet clothing with dry, warm clothing.
Warm the affected area: Soak the affected area in warm (not hot) water (37-40°C or 98.6-104°F) for 15-30 minutes. Do not use direct heat such as a heating pad or fire, as this can cause further damage.
Protect the area: After warming, keep the affected area dry and protected. Gently bandage the area with sterile dressings, separating fingers and toes with sterile gauze if needed.
Avoid rubbing: Do not rub or massage the affected area, as this can cause further tissue damage.
Seek medical attention: All but the mildest cases of frostbite should be evaluated by a healthcare professional.
Medical Treatments for Burns
While minor burns can often be treated at home with proper first aid, moderate to severe burns require medical intervention. The treatment approach depends on the depth, extent, location, and cause of the burn, as well as the patient’s age and overall health.
Assessment and Initial Care
Upon arrival at a medical facility, burn patients undergo a thorough assessment to determine the severity of the burn and the appropriate treatment plan. This assessment includes:
Burn depth and extent: Healthcare providers determine the depth of the burn and the percentage of body surface area affected.
Airway assessment: For burns involving the face, neck, or chest, or for burns that occurred in an enclosed space, healthcare providers assess the airway for potential inhalation injury.
Circulation assessment: The patient’s circulation is evaluated, particularly for circumferential burns (burns that encircle a body part), which can restrict blood flow.
Fluid resuscitation: For moderate to severe burns, intravenous fluids are administered to prevent dehydration and shock. The amount of fluid is calculated based on the patient’s weight and the extent of the burn, often using formulas such as the Parkland formula.
Pain management: Burn pain can be severe, so adequate pain control is a priority. This may include oral or intravenous pain medications, and in some cases, regional or general anesthesia for procedures.
Tetanus prophylaxis: Tetanus vaccination may be administered if the patient’s immunization status is not up to date.
Wound Care and Dressings
Proper wound care is essential for preventing infection and promoting healing. The approach depends on the depth and extent of the burn:
Cleaning: The burn wound is gently cleaned to remove debris, dead tissue, and bacteria. This may be done in a hydrotherapy tub or with showering.
Debridement: For deeper burns, debridement (removal of dead tissue) may be necessary to promote healing and prevent infection. This can be done surgically, enzymatically, or through mechanical methods.
Dressings: Various types of dressings may be used, depending on the burn’s characteristics. These include:
Non-adherent dressings for superficial burns. Antimicrobial dressings for burns at risk of infection. Absorbent dressings for weeping wounds. Biological dressings such as collagen or biosynthetic dressings for deeper burns.
The frequency of dressing changes depends on the type of dressing and the burn’s characteristics, ranging from daily to weekly changes.
Topical Treatments
Topical medications are often used to prevent infection and promote healing:
Antibiotic ointments: Silver sulfadiazine is commonly used for burn wounds due to its broad-spectrum antimicrobial activity. Other options include mupirocin, bacitracin, and neomycin.
Silver-based products: Various silver-impregnated dressings and creams are available, providing sustained antimicrobial activity.
Other antimicrobials: In some cases, other antimicrobial agents such as mafenide acetate or silver nitrate may be used, particularly for resistant infections.
Pain-relieving gels: Topical anesthetics such as lidocaine may be used to provide temporary pain relief during dressing changes.
Surgical Interventions