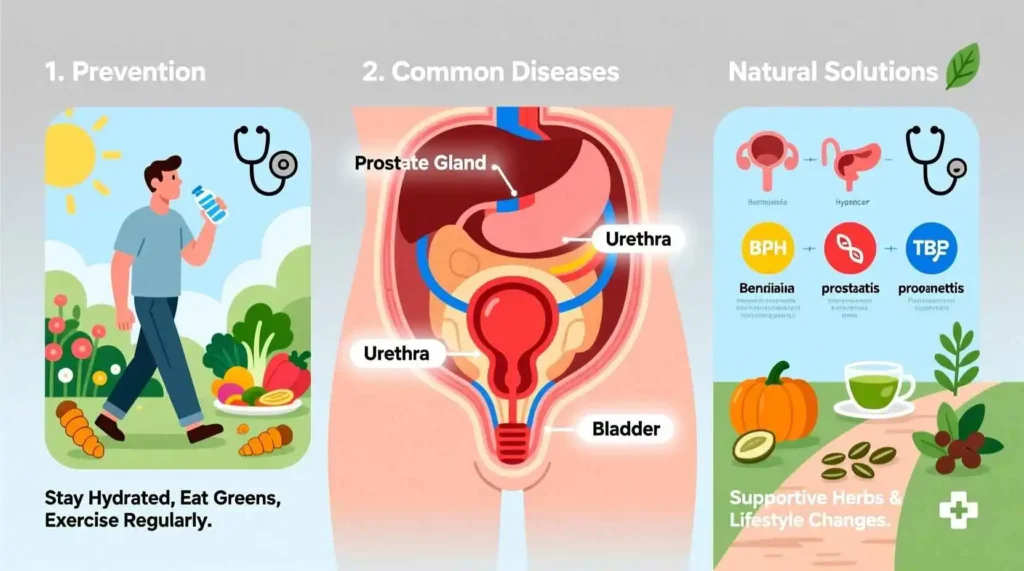
Prostate Health for Men: Prevention, Common Diseases and Natural Solutions
Introduction to Prostate Health
The prostate gland is a small, walnut-sized organ that plays a crucial role in the male reproductive system. Located just below the bladder and in front of the rectum, this gland surrounds the urethra, the tube through which urine and semen exit the body. Despite its small size, the prostate can have a significant impact on a man’s quality of life, particularly as he ages. Understanding prostate health, recognizing potential problems, and taking proactive steps to maintain this gland’s function are essential aspects of men’s healthcare that often go overlooked until issues arise.
Prostate health is a concern that becomes increasingly relevant as men age. By the age of 50, many men begin to experience changes in their prostate function, and by age 80, the majority of men will have some form of prostate issue. These conditions can range from benign enlargement to inflammation and cancer, each with its own set of symptoms, diagnostic approaches, and treatment options.
This comprehensive guide aims to provide men with the knowledge they need to understand their prostate, recognize potential problems, and take proactive steps to maintain their prostate health. We will explore the anatomy and function of the prostate, common conditions that affect it, diagnostic procedures, treatment options (both conventional and natural), and lifestyle modifications that can support prostate health throughout a man’s life.
Anatomy and Function of the Prostate
To understand prostate health, it’s essential first to grasp the basic anatomy and function of this gland. The prostate is part of the male reproductive system and is approximately the size of a walnut in young adult men, though it tends to grow larger with age. The gland is located in the pelvis, nestled between the bladder and the rectum, and it wraps around the urethra, which is the tube that carries urine from the bladder out of the body.
The prostate is composed of several zones, each with distinct functions and characteristics. The peripheral zone makes up about 70% of the prostate gland and is the area where most prostate cancers develop. The central zone accounts for about 25% of the gland and surrounds the ejaculatory ducts. The transition zone, which makes up only about 5% of the prostate in young men, is where benign prostatic hyperplasia (BPH) typically occurs. This zone tends to enlarge with age, potentially causing urinary symptoms.
The primary function of the prostate is to produce and secrete prostate fluid, which is one of the components of semen. This fluid is slightly alkaline, which helps to neutralize the acidity of the vaginal tract, protecting sperm and extending their lifespan. The prostate also contains smooth muscle tissue that helps to expel semen during ejaculation.
The prostate is influenced by male hormones, particularly testosterone and its more potent form, dihydrotestosterone (DHT). These hormones regulate prostate growth and function throughout a man’s life. As men age, hormonal changes can lead to prostate growth and changes in function, which may result in various prostate conditions.
Understanding the anatomy and function of the prostate provides a foundation for recognizing how different conditions can affect urinary and sexual function. It also helps explain why certain symptoms occur and how treatments target specific aspects of prostate health.
Common Prostate Conditions
Several conditions can affect the prostate gland, ranging from benign to malignant. The three most common prostate conditions are benign prostatic hyperplasia (BPH), prostatitis, and prostate cancer. Each of these conditions has distinct characteristics, symptoms, and treatment approaches.
Benign prostatic hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland that commonly occurs as men age. As the prostate grows larger, it can squeeze the urethra, causing urinary symptoms such as frequent urination, difficulty starting urination, weak urine stream, and the feeling of incomplete bladder emptying. BPH is not cancerous and does not increase the risk of developing prostate cancer, but it can significantly impact quality of life.
Prostatitis refers to inflammation of the prostate gland and can affect men of all ages. There are several types of prostatitis, including acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), and asymptomatic inflammatory prostatitis. Symptoms of prostatitis can include pain in the pelvic area, urinary problems, and sometimes flu-like symptoms in the case of bacterial prostatitis.
Prostate cancer is one of the most common cancers among men, particularly those over the age of 50. It occurs when cells in the prostate gland begin to grow uncontrollably. Prostate cancer often develops slowly and may not cause significant symptoms in its early stages. When symptoms do occur, they can include urinary problems, blood in the urine or semen, erectile dysfunction, and pain in the hips, back, or chest if the cancer has spread to other areas of the body.
Each of these conditions requires proper diagnosis and treatment, which may vary depending on the severity of the condition and the individual patient’s needs. Understanding the differences between these conditions is crucial for appropriate management and treatment.
Benign Prostatic Hyperplasia (BPH)
Benign prostatic hyperplasia (BPH), also known as benign prostatic enlargement (BPE), is a common condition that affects aging men. It is characterized by the non-cancerous growth of prostate cells, particularly in the transition zone of the gland. As the prostate enlarges, it can compress the urethra, leading to various urinary symptoms that can significantly impact a man’s quality of life.
The exact cause of BPH is not fully understood, but it is believed to be related to hormonal changes that occur with aging. As men grow older, the balance of hormones in the body changes, with a relative increase in estrogen compared to testosterone. Additionally, the enzyme 5-alpha reductase converts testosterone to dihydrotestosterone (DHT), which has been linked to prostate growth. These hormonal changes, combined with genetic factors and potentially lifestyle influences, contribute to the development of BPH.
The prevalence of BPH increases with age. By age 60, about 50% of men will have some degree of BPH, and by age 85, this number increases to about 90%. However, not all men with BPH will experience symptoms. The severity of symptoms can vary widely, from mild to severe, and may progress over time.
Symptoms of BPH are primarily related to urinary function and are often referred to as lower urinary tract symptoms (LUTS). These can be categorized into two groups: obstructive symptoms and irritative symptoms. Obstructive symptoms include difficulty starting urination, weak urine stream, straining to urinate, dribbling after urination, and the feeling of incomplete bladder emptying. Irritative symptoms include frequent urination (especially at night, a condition called nocturia), urgency (the sudden need to urinate), and urinary incontinence.
Diagnosis of BPH typically involves a combination of medical history assessment, physical examination (including a digital rectal exam), and various tests. These may include a urinalysis to rule out infection or other conditions, a prostate-specific antigen (PSA) blood test to screen for prostate cancer, urine flow studies to measure the strength and volume of urine flow, and imaging studies such as ultrasound to visualize the prostate and bladder. In some cases, a cystoscopy may be performed, which involves inserting a thin tube with a camera into the urethra to directly view the prostate and bladder.
Treatment for BPH depends on the severity of symptoms and the impact on quality of life. For mild symptoms, lifestyle modifications and watchful waiting may be recommended. These can include limiting fluids in the evening, avoiding caffeine and alcohol, double voiding (urinating, then waiting a few moments and trying again), and practicing bladder training exercises.
For more moderate to severe symptoms, medication may be prescribed. There are two main classes of drugs used to treat BPH: alpha blockers and 5-alpha reductase inhibitors. Alpha blockers, such as tamsulosin and alfuzosin, work by relaxing the muscles in the prostate and bladder neck, improving urine flow. 5-alpha reductase inhibitors, such as finasteride and dutasteride, work by blocking the conversion of testosterone to DHT, which can shrink the prostate over time. In some cases, a combination of these medications may be prescribed.
For men who do not respond to medication or have severe symptoms, minimally invasive procedures or surgery may be recommended. These can include transurethral resection of the prostate (TURP), laser surgery, microwave therapy, or prostate artery embolization, among others. These procedures aim to remove or reduce prostate tissue to relieve pressure on the urethra and improve urinary flow.
While BPH is a common and often manageable condition, it’s important for men experiencing urinary symptoms to seek medical evaluation to rule out other conditions, including prostate cancer, and to receive appropriate treatment.
Prostatitis
Prostatitis is a condition characterized by inflammation of the prostate gland and can affect men of all ages, unlike BPH and prostate cancer which are more common in older men. Prostatitis can be a challenging condition to diagnose and treat due to its various forms and overlapping symptoms with other urological conditions.
There are four main types of prostatitis, each with distinct characteristics and treatment approaches:
Acute bacterial prostatitis is the least common but most severe form of prostatitis. It is caused by a bacterial infection and typically presents with sudden and severe symptoms, including fever, chills, lower back pain, pelvic pain, and urinary symptoms such as frequency, urgency, and pain or burning during urination. This condition requires prompt medical attention and is usually treated with antibiotics.
Chronic bacterial prostatitis is a recurring bacterial infection of the prostate gland. It is characterized by persistent or recurrent urinary tract infections and pelvic discomfort. Symptoms may be less severe than acute bacterial prostatitis but can last for months. Treatment typically involves prolonged courses of antibiotics.
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is the most common form of prostatitis, accounting for about 90% of cases. It is not caused by bacteria and its exact cause is often unknown. Symptoms include persistent pain in the pelvic area, urinary problems, and sometimes sexual dysfunction. This condition can be challenging to treat and often requires a multifaceted approach.
Asymptomatic inflammatory prostatitis is characterized by inflammation of the prostate gland without any noticeable symptoms. It is usually discovered incidentally during examination for other conditions, such as infertility or prostate cancer screening. This form of prostatitis does not require treatment unless it is associated with other conditions.
The causes of prostatitis vary depending on the type. Bacterial prostatitis is caused by bacterial infections, often from the same bacteria that cause urinary tract infections. The exact cause of CP/CPPS is not well understood but may involve a combination of factors, including autoimmune responses, nervous system dysfunction, pelvic muscle spasms, and psychological stress.
Diagnosis of prostatitis involves a comprehensive evaluation, including medical history, physical examination (including a digital rectal exam), and various tests. These may include urinalysis and urine culture to check for infection, prostate fluid analysis (expressed prostatic secretions), blood tests, and imaging studies such as ultrasound or MRI. In some cases, urodynamic studies may be performed to evaluate bladder function.
Treatment for prostatitis depends on the type and severity of the condition. Acute bacterial prostatitis is typically treated with antibiotics for 4-6 weeks, along with pain relievers and other supportive measures. Chronic bacterial prostatitis may require longer courses of antibiotics, sometimes for several months.
Treatment for CP/CPPS is more challenging and often involves a combination of approaches. These may include pain management with nonsteroidal anti-inflammatory drugs (NSAIDs) or other pain relievers, alpha blockers to relax the muscles of the prostate and bladder, physical therapy to address pelvic muscle tension, and stress management techniques. Some men may benefit from alternative therapies such as acupuncture, biofeedback, or herbal supplements.
Lifestyle modifications can also play a role in managing prostatitis symptoms. These may include avoiding irritants such as caffeine, alcohol, and spicy foods, staying well-hydrated, practicing good hygiene, and engaging in regular physical activity. Pelvic floor exercises, also known as Kegel exercises, may help strengthen the pelvic muscles and improve symptoms in some cases.
Prostatitis can be a frustrating and painful condition, but with proper diagnosis and treatment, most men can find relief from their symptoms. It’s important for men experiencing pelvic pain, urinary symptoms, or other signs of prostatitis to seek medical evaluation to determine the underlying cause and receive appropriate treatment.
Prostate Cancer
Prostate cancer is one of the most common cancers among men worldwide, second only to skin cancer in many countries. It occurs when cells in the prostate gland begin to grow uncontrollably, forming tumors that can potentially spread to other parts of the body. Prostate cancer typically develops slowly and may not cause significant symptoms in its early stages, which is why regular screening is important for early detection.
The exact cause of prostate cancer is not fully understood, but several risk factors have been identified. Age is the most significant risk factor, with the disease being rare in men under 40 and most common in men over 65. Family history also plays a role, as men with a father or brother who has had prostate cancer are about twice as likely to develop the disease themselves. Race is another factor, with African American men having a higher risk of developing and dying from prostate cancer compared to men of other races.
Other potential risk factors for prostate cancer include diet, particularly a diet high in red meat and high-fat dairy products and low in fruits and vegetables, obesity, and exposure to certain chemicals. Some studies have also suggested a link between inflammation of the prostate (prostatitis) and sexually transmitted infections and an increased risk of prostate cancer, though more research is needed in these areas.
Prostate cancer often develops without causing noticeable symptoms in its early stages. As the cancer progresses, symptoms may include urinary problems similar to those seen with BPH, such as frequent urination (especially at night), difficulty starting or stopping urination, weak urine stream, and the feeling of incomplete bladder emptying. Other symptoms may include blood in the urine or semen, erectile dysfunction, pain in the hips, back, or chest (if the cancer has spread to the bones), and weakness or numbness in the legs or feet (if the cancer has compressed the spinal cord).
Diagnosis of prostate cancer typically involves several steps. The process often begins with a prostate-specific antigen (PSA) blood test and a digital rectal exam (DRE). If these tests suggest the possibility of cancer, a prostate biopsy may be performed, during which small samples of prostate tissue are removed and examined under a microscope for cancer cells. If cancer is found, additional tests may be done to determine the stage (extent) of the cancer, which is crucial for determining the appropriate treatment approach.
Prostate cancer staging takes into account the size of the tumor, whether the cancer has spread to nearby lymph nodes, and whether it has metastasized (spread) to distant parts of the body. The Gleason score is also used to grade prostate cancer based on how abnormal the cancer cells look under a microscope, with higher scores indicating more aggressive cancer.
Treatment for prostate cancer depends on several factors, including the stage and grade of the cancer, the patient’s age and overall health, and the patient’s personal preferences. For early-stage prostate cancer that is slow-growing, active surveillance (also known as watchful waiting) may be recommended, which involves regular monitoring of the cancer without immediate treatment.
For more aggressive or advanced prostate cancer, treatment options may include surgery to remove the prostate gland (radical prostatectomy), radiation therapy (either external beam radiation or brachytherapy, which involves placing radioactive seeds directly into the prostate), hormone therapy to reduce testosterone levels (which can fuel the growth of prostate cancer), chemotherapy, immunotherapy, or targeted therapy. In many cases, a combination of these treatments may be used.
The side effects of prostate cancer treatment can be significant and may include urinary incontinence, erectile dysfunction, bowel problems, and fatigue. These side effects can have a substantial impact on quality of life, so it’s important for men to discuss potential side effects with their healthcare team and consider them when making treatment decisions.
Prostate cancer is a serious condition, but when detected early, it is often treatable. Regular screening with PSA tests and DREs can help detect prostate cancer in its early stages, when treatment is most effective. Men should discuss with their healthcare providers when to begin prostate cancer screening based on their individual risk factors and preferences.
Risk Factors for Prostate Diseases
Understanding the risk factors for prostate diseases can help men take proactive steps to maintain their prostate health and seek appropriate screening and care. While some risk factors cannot be changed, such as age and genetics, others can be modified through lifestyle changes.
Age is the most significant risk factor for prostate diseases, particularly BPH and prostate cancer. As men age, the prostate naturally grows larger, and the risk of developing prostate conditions increases. BPH rarely causes symptoms before age 40, but by age 60, about half of men will have some signs of BPH. By age 85, this number increases to about 90%. Similarly, prostate cancer is rare in men under 40, but the risk increases significantly after age 50, with about 6 in 10 cases diagnosed in men over 65.
Family history and genetics also play a role in prostate health. Men who have a father or brother who has had prostate cancer are about twice as likely to develop the disease themselves. If multiple relatives have been affected, particularly at a young age, the risk is even higher. Certain genetic mutations, such as BRCA1 and BRCA2, which are more commonly associated with breast and ovarian cancer, can also increase the risk of prostate cancer in men.
Race and ethnicity are additional risk factors for prostate diseases. African American men have a higher risk of developing prostate cancer compared to men of other races, and they are more likely to be diagnosed at a younger age and with more aggressive disease. The reasons for these disparities are not fully understood but may involve a combination of genetic, environmental, and socioeconomic factors.
Diet and lifestyle factors can also influence prostate health. A diet high in red meat and high-fat dairy products and low in fruits and vegetables has been associated with an increased risk of prostate cancer. Obesity is another risk factor, as it has been linked to a higher risk of aggressive prostate cancer and poorer outcomes after diagnosis. Conversely, a diet rich in fruits, vegetables, whole grains, and healthy fats (such as those found in fish, nuts, and olive oil) may help protect against prostate diseases.
Physical activity is another important factor in prostate health. Regular exercise has been associated with a lower risk of prostate cancer and may also help manage symptoms of BPH. Exercise can help maintain a healthy weight, reduce inflammation, and improve overall health, all of which can benefit the prostate.
Smoking is a risk factor for many health conditions, including prostate diseases. Studies have suggested that smokers may have an increased risk of developing aggressive prostate cancer and a higher risk of dying from the disease. Quitting smoking can reduce these risks and improve overall health.
Exposure to certain chemicals and environmental toxins may also increase the risk of prostate diseases. Men who work in occupations that involve exposure to pesticides, herbicides, or heavy metals may have a higher risk of prostate cancer. While it may not be possible to avoid all environmental exposures, being aware of potential risks and taking appropriate precautions can help protect prostate health.
Chronic inflammation has been linked to an increased risk of prostate cancer. Conditions such as prostatitis, which cause inflammation of the prostate, may contribute to this risk. Managing inflammation through diet, lifestyle changes, and appropriate medical care may help reduce the risk of prostate diseases.
Sexual activity and history have also been studied in relation to prostate health. Some research has suggested that men with a higher frequency of ejaculation may have a lower risk of prostate cancer, though more studies are needed to confirm this association. Sexually transmitted infections have been linked to an increased risk of prostate cancer, so practicing safe sex and seeking prompt treatment for infections may help protect prostate health.
By understanding these risk factors, men can take proactive steps to maintain their prostate health. While some risk factors cannot be changed, such as age and genetics, others can be modified through lifestyle changes, including maintaining a healthy diet, exercising regularly, avoiding smoking, limiting alcohol consumption, and managing stress. Regular medical check-ups and appropriate screening based on individual risk factors are also important components of prostate health maintenance.
Symptoms of Prostate Problems
Recognizing the symptoms of prostate problems is crucial for early detection and treatment. While different prostate conditions can cause similar symptoms, understanding these signs can prompt men to seek medical evaluation and appropriate care.
Urinary symptoms are among the most common signs of prostate problems. These symptoms, collectively known as lower urinary tract symptoms (LUTS), can include:
Frequent urination, particularly during the night (nocturia), is a common symptom of prostate enlargement. Men may find themselves waking up multiple times to urinate, which can disrupt sleep and affect quality of life. Urgency, the sudden and intense need to urinate, is another common symptom that can make it difficult to delay urination once the need arises.
Difficulty starting urination, known as hesitancy, can occur when the enlarged prostate compresses the urethra, making it harder for urine to flow. Once urination begins, the urine stream may be weak or interrupted, and it may take longer to empty the bladder completely. Some men may also experience straining to urinate or a feeling that the bladder is not completely empty after urination.
Dribbling after urination is another common symptom, where urine continues to leak out after finishing urination. This can be embarrassing and may require men to wear protective pads or take other measures to manage the leakage.
Pain or discomfort during urination, known as dysuria, can occur with various prostate conditions, particularly prostatitis. This pain or burning sensation can make urination uncomfortable and may be accompanied by other symptoms such as fever or chills in cases of bacterial prostatitis.
Blood in the urine (hematuria) or semen (hematospermia) can be alarming symptoms that warrant immediate medical attention. While these symptoms can be caused by various conditions, including prostate cancer, they can also result from less serious issues such as infection or inflammation.
Sexual dysfunction can also be a symptom of prostate problems. Erectile dysfunction, the inability to achieve or maintain an erection sufficient for sexual activity, can be caused by various prostate conditions and their treatments. Painful ejaculation, reduced sexual desire, and difficulty achieving orgasm are other sexual symptoms that can occur with prostate problems.
Pain and discomfort in the pelvic area are common symptoms of prostatitis and can also occur with other prostate conditions. This pain may be felt in the perineum (the area between the scrotum and rectum), lower back, hips, or upper thighs. The pain may be constant or intermittent and can range from mild to severe.
Systemic symptoms such as fever, chills, fatigue, and body aches can occur with acute bacterial prostatitis, which is a serious condition that requires prompt medical treatment. These symptoms are less common with other prostate conditions but can occur in advanced cases of prostate cancer that has spread to other parts of the body.
In advanced cases of prostate cancer, additional symptoms may occur as the cancer spreads to other parts of the body. These can include bone pain (particularly in the spine, hips, or ribs), unexplained weight loss, weakness or numbness in the legs or feet (if the cancer compresses the spinal cord), and swelling in the legs or feet (if lymph nodes are affected).
It’s important to note that many prostate conditions, particularly in their early stages, may not cause any noticeable symptoms. This is particularly true for prostate cancer, which can develop silently for years before symptoms appear. Regular screening with prostate-specific antigen (PSA) tests and digital rectal exams (DREs) can help detect prostate problems before symptoms develop, when treatment is most effective.
Men experiencing any of these symptoms should seek medical evaluation to determine the underlying cause and receive appropriate treatment. While these symptoms can be caused by various prostate conditions, they can also result from other health issues, so a comprehensive medical evaluation is essential for accurate diagnosis and treatment.
Diagnostic Procedures for Prostate Conditions
Diagnosing prostate conditions involves a comprehensive evaluation that includes medical history, physical examination, and various diagnostic tests. The specific approach depends on the suspected condition, the patient’s symptoms, and individual risk factors.
The diagnostic process typically begins with a thorough medical history, during which the healthcare provider will ask about symptoms, their duration and severity, and any factors that worsen or alleviate them. The provider will also inquire about the patient’s personal and family medical history, particularly any history of prostate problems, and lifestyle factors that may influence prostate health.
A physical examination is an essential component of the diagnostic process for prostate conditions. This includes a digital rectal exam (DRE), during which the healthcare provider inserts a gloved, lubricated finger into the rectum to feel the prostate gland. The DRE allows the provider to assess the size, shape, and texture of the prostate, checking for any abnormalities such as lumps, hard areas, or enlargement that may indicate prostate cancer or other conditions.
Blood tests are commonly used in the evaluation of prostate conditions. The prostate-specific antigen (PSA) test measures the level of PSA, a protein produced by the prostate gland, in the blood. Elevated PSA levels can indicate various prostate conditions, including BPH, prostatitis, and prostate cancer. While the PSA test is not specific for prostate cancer, it is an important tool in prostate cancer screening and monitoring. Other blood tests may include a complete blood count (CBC) to check for signs of infection or inflammation, and kidney function tests to assess how well the kidneys are working, particularly if urinary symptoms are severe.
Urinalysis and urine culture are often performed to evaluate urinary symptoms and check for signs of infection or other abnormalities. A urinalysis involves examining a urine sample for the presence of blood, white blood cells, bacteria, or other substances that may indicate infection or inflammation. A urine culture involves growing bacteria from a urine sample in a laboratory to identify the specific type of bacteria causing an infection and determine which antibiotics will be most effective in treating it.
Prostate fluid analysis may be performed in cases of suspected prostatitis. This test, also known as expressed prostatic secretions (EPS), involves collecting a sample of fluid from the prostate gland during a digital rectal exam. The fluid is then examined under a microscope for signs of inflammation or infection.
Imaging studies can provide valuable information about the prostate gland and surrounding structures. Ultrasound, particularly transrectal ultrasound (TRUS), is commonly used to visualize the prostate gland. During a TRUS, a small ultrasound probe is inserted into the rectum, allowing for detailed images of the prostate. This procedure can help determine the size of the prostate gland, identify abnormalities, and guide prostate biopsy.
Magnetic resonance imaging (MRI) may be used to provide more detailed images of the prostate gland, particularly in cases of suspected prostate cancer. Multiparametric MRI (mpMRI) is a specialized type of MRI that can help identify suspicious areas in the prostate that may require biopsy. This imaging technique can also help determine the extent of prostate cancer and whether it has spread beyond the prostate gland.
Urodynamic studies may be performed to evaluate bladder function and urinary symptoms in men with BPH or other prostate conditions. These tests measure various aspects of bladder function, including urine flow rate, bladder pressure, and the amount of urine left in the bladder after urination (post-void residual). Urodynamic studies can help determine the cause of urinary symptoms and guide treatment decisions.
Cystoscopy involves inserting a thin, flexible tube with a camera (cystoscope) into the urethra to directly visualize the urethra, prostate, and bladder. This procedure can help identify abnormalities such as blockages, stones, or tumors that may be causing urinary symptoms. Cystoscopy is typically performed in cases where other diagnostic tests have not provided a clear diagnosis or when treatment planning requires direct visualization of the urinary tract.
Prostate biopsy is often performed when prostate cancer is suspected, particularly if PSA levels are elevated or abnormalities are found during a digital rectal exam or imaging studies. During a prostate biopsy, small samples of prostate tissue are removed using a thin needle, usually guided by transrectal ultrasound. The tissue samples are then examined under a microscope by a pathologist to determine whether cancer cells are present. If cancer is found, the pathologist will also determine the grade of the cancer (how abnormal the cells look) and the Gleason score, which helps predict how quickly the cancer is likely to grow and spread.
In recent years, new diagnostic approaches have been developed to improve the accuracy of prostate cancer diagnosis and reduce unnecessary biopsies. These include liquid biopsies, which analyze blood or urine samples for biomarkers that may indicate prostate cancer, and targeted biopsy techniques, which use MRI or other imaging to guide biopsy needles to suspicious areas of the prostate.
The diagnostic approach for prostate conditions is tailored to each individual patient based on their symptoms, risk factors, and initial test results. A comprehensive evaluation is essential for accurate diagnosis and appropriate treatment planning. Men should discuss with their healthcare providers which diagnostic tests are most appropriate for their specific situation and what to expect during the evaluation process.
Conventional Treatment Options for Prostate Conditions
Treatment for prostate conditions depends on the specific diagnosis, the severity of symptoms, and the patient’s overall health and preferences. Conventional treatment options range from watchful waiting and medication to minimally invasive procedures and surgery.
For benign prostatic hyperplasia (BPH), treatment options vary based on the severity of symptoms. For mild symptoms, watchful waiting or active surveillance may be recommended, which involves regular monitoring without immediate treatment. Lifestyle modifications, such as limiting fluids in the evening, avoiding caffeine and alcohol, double voiding (urinating, then waiting a few moments and trying again), and practicing bladder training exercises, may help manage symptoms.
Medications are commonly used to treat moderate to severe BPH symptoms. Alpha blockers, such as tamsulosin, alfuzosin, silodosin, and terazosin, work by relaxing the muscles in the prostate and bladder neck, improving urine flow and reducing symptoms. These medications typically provide relief within a few days but do not reduce the size of the prostate.
5-alpha reductase inhibitors, such as finasteride and dutasteride, work by blocking the conversion of testosterone to dihydrotestosterone (DHT), which can shrink the prostate over time. These medications may take several months to achieve their full effect and are most effective in men with significantly enlarged prostates. In some cases, a combination of alpha blockers and 5-alpha reductase inhibitors may be prescribed for more effective symptom relief.
Phosphodiesterase-5 inhibitors, such as tadalafil (Cialis), which is primarily used to treat erectile dysfunction, have also been approved for the treatment of BPH. These medications work by relaxing the smooth muscles in the lower urinary tract, improving urine flow and reducing symptoms.
For men with BPH who do not respond to medication or have severe symptoms, minimally invasive procedures or surgery may be recommended. Transurethral resection of the prostate (TURP) has long been the gold standard surgical treatment for BPH. During this procedure, a resectoscope is inserted through the urethra, and excess prostate tissue is removed to relieve pressure on the urethra. TURP is highly effective but can have side effects such as erectile dysfunction, urinary incontinence, and retrograde ejaculation (semen flowing backward into the bladder during ejaculation).
Laser procedures, such as holmium laser enucleation of the prostate (HoLEP) and photoselective vaporization of the prostate (PVP), use laser energy to remove or vaporize excess prostate tissue. These procedures are less invasive than TURP and may have fewer side effects, particularly regarding sexual function.
Other minimally invasive procedures for BPH include transurethral microwave therapy (TUMT), which uses microwave energy to destroy excess prostate tissue; transurethral needle ablation (TUNA), which uses radiofrequency energy to destroy prostate tissue; and prostate artery embolization (PAE), which involves blocking the blood supply to the prostate to reduce its size. These procedures are less invasive than surgery but may not be as effective for very large prostates.
For prostatitis, treatment depends on the type and underlying cause. Acute bacterial prostatitis is typically treated with antibiotics for 4-6 weeks, along with pain relievers and other supportive measures. Hospitalization may be necessary for severe cases with high fever or difficulty urinating.
Chronic bacterial prostatitis may require longer courses of antibiotics, sometimes for several months. In some cases, low-dose antibiotics may be prescribed for an extended period to prevent recurrent infections.
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is more challenging to treat and often requires a multimodal approach. Treatment may include pain management with nonsteroidal anti-inflammatory drugs (NSAIDs) or other pain relievers, alpha blockers to relax the muscles of the prostate and bladder, physical therapy to address pelvic muscle tension, and stress management techniques. Some men may benefit from medications such as amitriptyline or gabapentin for pain management, or finasteride to reduce prostate inflammation.
For prostate cancer, treatment options depend on the stage and grade of the cancer, the patient’s age and overall health, and personal preferences. For early-stage, slow-growing prostate cancer, active surveillance or watchful waiting may be recommended, which involves regular monitoring with PSA tests, DREs, and periodic biopsies, with treatment initiated only if the cancer shows signs of progression.
Radical prostatectomy, the surgical removal of the entire prostate gland and some surrounding tissue, is a common treatment for localized prostate cancer. This can be performed through open surgery or using minimally invasive techniques such as laparoscopic or robot-assisted surgery. Potential side effects include urinary incontinence and erectile dysfunction.
Radiation therapy is another treatment option for localized prostate cancer. External beam radiation therapy (EBRT) involves directing high-energy X-rays at the prostate gland from outside the body, typically over several weeks. Brachytherapy involves placing radioactive seeds directly into the prostate gland, where they deliver radiation over time. Side effects of radiation therapy can include urinary problems, bowel problems, and erectile dysfunction.
Hormone therapy, also known as androgen deprivation therapy (ADT), is used to treat advanced prostate cancer or in combination with other treatments for localized disease. This therapy works by reducing testosterone levels, which can fuel the growth of prostate cancer. Hormone therapy can be achieved through medications that block testosterone production or action, or through surgical removal of the testicles (orchiectomy). Side effects can include hot flashes, loss of libido, erectile dysfunction, osteoporosis, and metabolic changes.
Chemotherapy may be used to treat prostate cancer that has spread to other parts of the body and is no longer responding to hormone therapy. Chemotherapy drugs kill rapidly dividing cells, including cancer cells, but can also affect healthy cells, leading to side effects such as nausea, hair loss, fatigue, and increased risk of infection.
Immunotherapy and targeted therapy are newer approaches to treating advanced prostate cancer. Immunotherapy works by stimulating the body’s immune system to recognize and attack cancer cells. Sipuleucel-T (Provenge) is an immunotherapy approved for the treatment of advanced prostate cancer. Targeted therapy drugs work by targeting specific molecules involved in cancer growth and progression. PARP inhibitors, such as olaparib and rucaparib, are targeted therapies that have shown promise in treating prostate cancer with certain genetic mutations.
The choice of treatment for prostate conditions is a personal decision that should be made in consultation with healthcare providers, taking into account the specific diagnosis, the severity of symptoms, potential side effects, and the patient’s overall health and preferences. Men should discuss all available treatment options, including their benefits and risks, with their healthcare team to make an informed decision.
Natural Remedies and Lifestyle Approaches for Prostate Health
In addition to conventional medical treatments, many men are interested in natural remedies and lifestyle approaches to support prostate health and manage prostate conditions. While these approaches should not replace medical treatment for diagnosed conditions, they can complement conventional therapies and may help reduce the risk of developing prostate problems.
Diet plays a crucial role in prostate health. A diet rich in fruits, vegetables, whole grains, and healthy fats can provide essential nutrients and antioxidants that support prostate health. Tomatoes and tomato products are particularly beneficial due to their high content of lycopene, a powerful antioxidant that has been associated with a reduced risk of prostate cancer. Cooking tomatoes with a small amount of oil can increase the absorption of lycopene.
Cruciferous vegetables such as broccoli, cauliflower, cabbage, and Brussels sprouts contain compounds called sulforaphane and indoles, which have been shown to have anti-cancer properties and may help protect against prostate cancer. These vegetables are most nutritious when lightly steamed or stir-fried, as overcooking can destroy some of their beneficial compounds.
Berries, particularly blueberries, strawberries, and raspberries, are rich in antioxidants and anti-inflammatory compounds that can support prostate health. Green tea is another beverage that has been associated with prostate health benefits due to its high content of polyphenols, particularly epigallocatechin gallate (EGCG), which has been shown to have anti-cancer properties.
Healthy fats, particularly those found in fatty fish such as salmon, mackerel, and sardines, can also support prostate health. These fish are rich in omega-3 fatty acids, which have anti-inflammatory properties and may help reduce the risk of prostate cancer. Nuts and seeds, particularly walnuts, flaxseeds, and pumpkin seeds, are also good sources of healthy fats and other nutrients that support prostate health.
On the other hand, a diet high in red meat, processed meats, and high-fat dairy products has been associated with an increased risk of prostate cancer and other prostate problems. Limiting these foods and replacing them with healthier alternatives can help support prostate health.
Soy products such as tofu, tempeh, and edamame contain compounds called isoflavones, which have been associated with a reduced risk of prostate cancer. These compounds may help regulate hormone levels and inhibit the growth of cancer cells.
Several herbal supplements have been studied for their potential benefits for prostate health. Saw palmetto is one of the most commonly used supplements for BPH, and some studies have suggested that it may help improve urinary symptoms and flow. However, other studies have found no significant benefit compared to placebo, so the evidence is mixed.
Beta-sitosterol, a plant sterol found in many fruits, vegetables, nuts, and seeds, has been shown in some studies to improve urinary symptoms and flow in men with BPH. Pygeum africanum, an extract from the bark of the African plum tree, has also been used to treat BPH symptoms, with some studies showing modest benefits.
Stinging nettle root extract is another herbal remedy that has been used for BPH, often in combination with saw palmetto. Some studies have suggested that it may help improve urinary symptoms and reduce the size of the prostate.
For prostatitis, particularly chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), quercetin, a flavonoid found in many fruits and vegetables, has shown promise in reducing symptoms. Some studies have found that quercetin supplements can improve pain and quality of life in men with CP/CPPS.
Rye grass pollen extract has also been studied for its potential benefits for prostatitis, with some research suggesting that it may help reduce inflammation and improve symptoms.
It’s important to note that while these herbal supplements may offer benefits for some men, they are not regulated by the FDA in the same way as medications, and their quality and effectiveness can vary. Men considering herbal supplements should discuss them with their healthcare provider to ensure they are safe and appropriate for their specific situation.
Regular physical activity is another important lifestyle factor for prostate health. Exercise has been associated with a reduced risk of prostate cancer and may help manage symptoms of BPH and prostatitis. Both aerobic exercise (such as walking, jogging, swimming, or cycling) and strength training can be beneficial.
Exercise can help maintain a healthy weight, reduce inflammation, improve immune function, and regulate hormone levels, all of which can support prostate health. Even moderate exercise, such as brisk walking for 30 minutes most days of the week, can have significant benefits.
Maintaining a healthy weight is particularly important for prostate health. Obesity has been linked to an increased risk of aggressive prostate cancer and poorer outcomes after diagnosis. Losing excess weight through a combination of diet and exercise can help reduce this risk and improve overall health.
Stress management is another important aspect of prostate health. Chronic stress can contribute to inflammation and may exacerbate symptoms of prostatitis and other prostate conditions. Techniques such as meditation, deep breathing exercises, yoga, tai chi, and progressive muscle relaxation can help reduce stress and promote overall well-being.
Adequate sleep is also crucial for prostate health. Poor sleep has been associated with an increased risk of prostate cancer and may worsen symptoms of prostate conditions. Aim for 7-8 hours of quality sleep per night, and practice good sleep hygiene by maintaining a regular sleep schedule, creating a comfortable sleep environment, and avoiding caffeine and electronic devices before bedtime.
Limiting alcohol consumption is another lifestyle change that can support prostate health. Excessive alcohol intake has been associated with an increased risk of prostate cancer and can worsen urinary symptoms in men with BPH. If you choose to drink alcohol, do so in moderation, defined as up to two drinks per day for men.
Smoking is a risk factor for many health conditions, including prostate cancer. Studies have suggested that smokers may have an increased risk of developing aggressive prostate cancer and a higher risk of dying from the disease. Quitting smoking can reduce these risks and improve overall health.
Pelvic floor exercises, also known as Kegel exercises, can help strengthen the muscles that support the bladder and prostate, improving urinary control and reducing symptoms of BPH and prostatitis. These exercises involve contracting and relaxing the pelvic floor muscles, which are the muscles used to stop urination midstream. Regular practice of these exercises can lead to significant improvements in urinary symptoms.
Hydration is important for prostate health, but it’s also important to manage fluid intake, particularly in the evening, to avoid disrupting sleep with frequent nighttime urination. Aim to drink plenty of water throughout the day, but limit fluids for a few hours before bedtime.
Regular sexual activity may also support prostate health. Some studies have suggested that men with a higher frequency of ejaculation may have a lower risk of prostate cancer, though more research is needed to confirm this association. Sexual activity can also help maintain prostate function by promoting regular ejaculation, which may help clear potentially harmful substances from the prostate gland.
While natural remedies and lifestyle approaches can support prostate health and complement conventional treatments, they should not be used as a substitute for medical care. Men with prostate symptoms or diagnosed conditions should work with their healthcare providers to develop a comprehensive treatment plan that includes both conventional and natural approaches as appropriate.
Prevention Strategies for Prostate Diseases





