How to Prevent Fever: Tips for Staying Healthy and Avoiding Common Causes
Fever is one of the most common medical symptoms experienced by people of all ages. It is not a disease itself but rather a sign that the body is fighting off an infection or illness. Understanding fever, its various types, causes, symptoms, diagnosis, treatment options, and prevention methods is essential for proper management and knowing when to seek medical attention. This comprehensive guide explores fever in detail, providing valuable insights into this physiological response and offering practical advice for dealing with it effectively.
The Physiology of Fever
Fever is a complex physiological response that involves the body’s temperature regulation system. Under normal circumstances, the human body maintains a core temperature of approximately 98.6°F (37°C), with slight variations throughout the day. This temperature regulation is controlled by the hypothalamus, a small region in the brain that acts as the body’s thermostat.
When the body detects the presence of pathogens such as bacteria, viruses, or fungi, immune cells release substances called pyrogens. These pyrogens travel through the bloodstream to the hypothalamus, causing it to reset the body’s thermostat to a higher temperature. This elevated temperature set point triggers various responses in the body to generate and conserve heat, resulting in fever.
The physiological changes during fever include vasoconstriction of blood vessels near the skin surface to reduce heat loss, increased muscle tone and shivering to generate heat, and increased metabolic rate. These changes work together to raise the body’s temperature to the new set point established by the hypothalamus.
Fever serves as a defense mechanism against infections. Elevated body temperature can inhibit the growth of many pathogens, enhance the function of immune cells, and increase the production of antibodies. While fever can be uncomfortable, it is generally beneficial and indicates that the immune system is functioning properly.
Types of Fever
Fever can be classified in several ways based on its pattern, duration, and severity. Understanding these different types can help healthcare providers determine the underlying cause and appropriate treatment approach.
Classification by Temperature
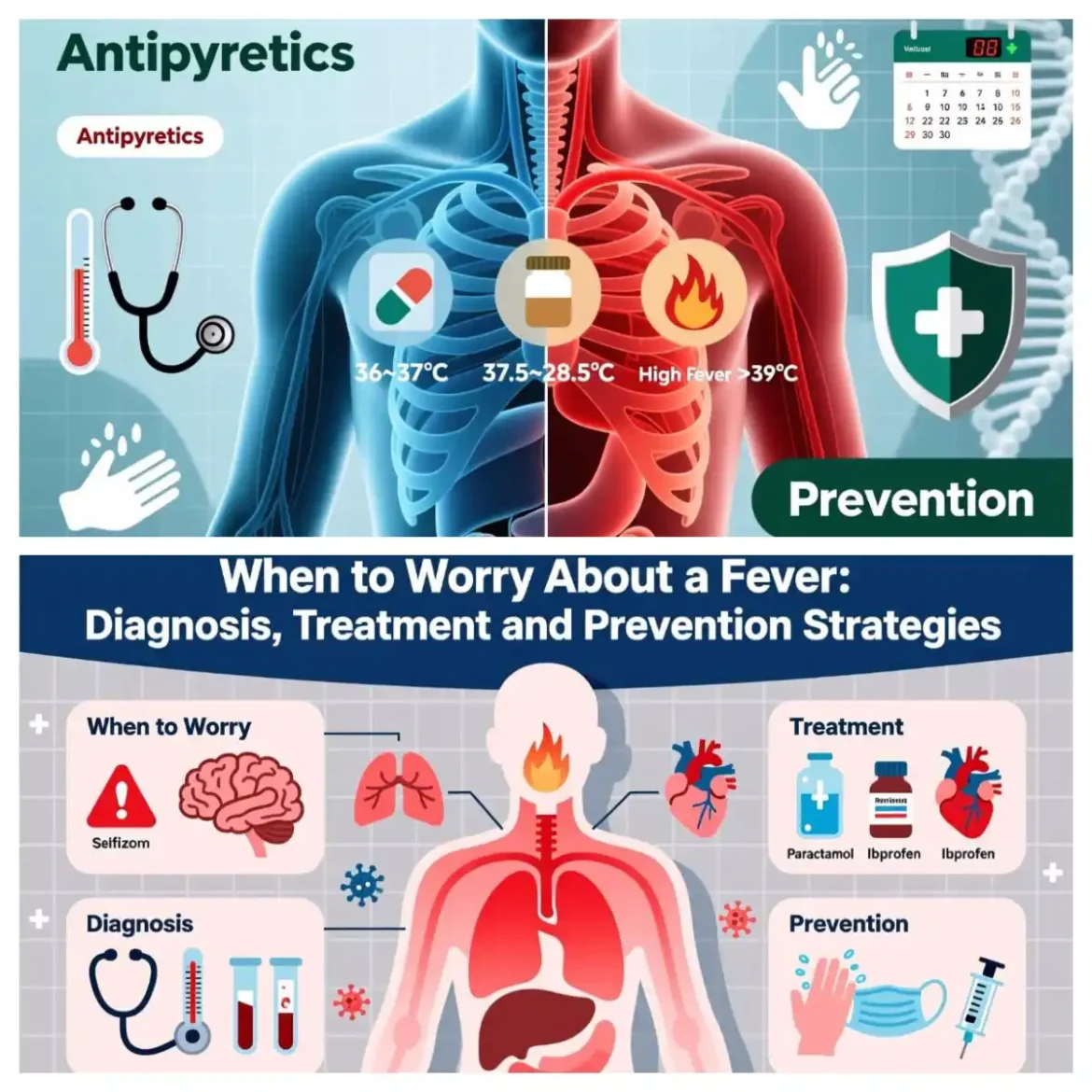
- Low-Grade Fever A low-grade fever is typically defined as a body temperature between 100.4°F (38°C) and 102.2°F (39°C). This type of fever is common with mild infections and inflammatory conditions. Low-grade fevers often do not require treatment unless they cause significant discomfort or are associated with other concerning symptoms.
- Moderate Fever Moderate fever refers to body temperatures ranging from 102.2°F (39°C) to 104.0°F (40°C). This level of fever indicates a more significant immune response and is often seen with more severe infections or inflammatory conditions. Moderate fevers may cause more pronounced symptoms such as headache, muscle aches, and fatigue.
- High-Grade Fever High-grade fever is characterized by temperatures above 104.0°F (40°C). This type of fever requires medical attention, especially in children, older adults, and individuals with compromised immune systems. High-grade fevers can lead to complications such as dehydration, seizures (particularly in young children), and altered mental status.
- Hyperpyrexia Hyperpyrexia is an extremely high fever with temperatures exceeding 106.7°F (41.5°C). This is a medical emergency that requires immediate intervention. Hyperpyrexia can cause serious complications, including organ damage and neurological effects.
Classification by Pattern
- Continuous Fever Continuous fever is characterized by a persistently elevated temperature that does not fluctuate by more than 1°C (1.8°F) during a 24-hour period. The temperature remains above normal throughout the day and night. This pattern is often seen in conditions such as typhoid fever, urinary tract infections, and lobar pneumonia.
- Intermittent Fever Intermittent fever is defined by temperature elevations that occur only at certain times of the day, with the temperature returning to normal between episodes. The febrile and afebrile periods alternate in a regular pattern. Malaria is a classic example of a disease that causes intermittent fever, with fever spikes occurring every 48 or 72 hours depending on the species of Plasmodium parasite.
- Remittent Fever Remittent fever is characterized by fluctuations in body temperature, but the temperature never returns to normal within a 24-hour period. The temperature may vary by more than 1°C (1.8°F) but remains elevated above normal. This pattern is commonly associated with infections such as infective endocarditis and certain viral illnesses.
- Relapsing Fever Relapsing fever consists of periods of fever alternating with afebrile periods, with each febrile episode lasting for several days followed by several days of normal temperature. This pattern is seen in conditions such as relapsing fever caused by Borrelia species and some cases of brucellosis.
- Pel-Ebstein Fever Pel-Ebstein fever is a specific pattern of fever associated with Hodgkin’s lymphoma. It is characterized by afebrile periods of about one week followed by febrile periods of similar duration, creating a cyclical pattern.
Classification by Duration
- Acute Fever Acute fever lasts for less than one week. It is typically caused by common infections such as viral upper respiratory tract infections, influenza, or urinary tract infections. Acute fevers usually resolve with treatment of the underlying cause.
- Subacute Fever Subacute fever persists for one to two weeks. This duration may indicate infections that take longer to resolve, such as certain viral infections, early stages of bacterial infections, or non-infectious inflammatory conditions.
- Chronic Fever Chronic fever is defined as fever lasting more than two weeks. This prolonged duration often requires more extensive investigation to determine the underlying cause. Chronic fever can be caused by persistent infections, inflammatory conditions, malignancies, or other systemic diseases.
Causes of Fever
Fever can result from a wide range of conditions, including infections, inflammatory disorders, medications, and other medical conditions. Identifying the underlying cause is essential for appropriate treatment and management.
Infectious Causes
- Viral Infections Viral infections are among the most common causes of fever. Examples include:
- Common cold and influenza
- COVID-19
- Gastroenteritis (stomach flu)
- Respiratory syncytial virus (RSV)
- Varicella (chickenpox)
- Measles, mumps, and rubella
- Viral hepatitis
- Dengue fever
- Viral meningitis and encephalitis
- HIV (during acute infection and later stages)
- Bacterial Infections Bacterial infections often cause more significant fevers than viral infections. Common bacterial causes of fever include:
- Strep throat
- Urinary tract infections
- Pneumonia
- Tuberculosis
- Meningitis
- Sepsis
- Lyme disease
- Typhoid fever
- Bacterial gastroenteritis (e.g., Salmonella, E. coli)
- Skin and soft tissue infections (cellulitis, abscesses)
- Fungal Infections Fungal infections are less common causes of fever but can be serious, especially in immunocompromised individuals. Examples include:
- Candidiasis
- Aspergillosis
- Histoplasmosis
- Coccidioidomycosis
- Cryptococcosis
- Parasitic Infections Parasitic infections can cause fever, particularly in tropical and subtropical regions. Common parasitic causes include:
- Malaria
- Toxoplasmosis
- Schistosomiasis
- Trypanosomiasis (sleeping sickness, Chagas disease)
- Leishmaniasis
Non-Infectious Causes
- Inflammatory and Autoimmune Disorders Many inflammatory and autoimmune conditions can cause fever, often as part of a systemic inflammatory response. Examples include:
- Rheumatoid arthritis
- Systemic lupus erythematosus (SLE)
- Inflammatory bowel disease (Crohn’s disease, ulcerative colitis)
- Giant cell arteritis and polymyalgia rheumatica
- Still’s disease
- Sarcoidosis
- Inflammatory myopathies
- Vasculitis
- Malignancies Cancer can cause fever through various mechanisms, including the production of pyrogens by tumor cells, tumor necrosis, or secondary infections. Malignancies associated with fever include:
- Lymphomas (Hodgkin’s and non-Hodgkin’s)
- Leukemias
- Renal cell carcinoma
- Hepatocellular carcinoma
- Metastatic cancer to various organs
- Solid tumors with central necrosis
- Medications and Vaccines Many medications and vaccines can cause fever as a side effect. Common examples include:
- Antibiotics (especially beta-lactams, sulfonamides)
- Anticonvulsants
- Antihypertensives
- Antiarrhythmics
- Certain antidepressants and antipsychotics
- Vaccines (fever is a common and expected response to many vaccines)
- Drug fever (an idiosyncratic reaction to medications)
- Endocrine Disorders Certain endocrine conditions can disrupt the body’s temperature regulation and cause fever:
- Hyperthyroidism (thyrotoxicosis)
- Adrenal insufficiency (Addisonian crisis)
- Pheochromocytoma
- Neurological Conditions Some neurological disorders can affect temperature regulation and cause fever:
- Stroke or hemorrhage affecting the hypothalamus
- Traumatic brain injury
- Spinal cord injuries (especially above T6)
- Autonomic dysfunction
- Neuroleptic malignant syndrome
- Malignant hyperthermia (a genetic condition triggered by certain anesthetics)
- Other Causes Various other conditions can cause fever:
- Deep vein thrombosis and pulmonary embolism
- Gout and pseudogout
- Familial Mediterranean fever
- Periodic fever syndromes
- Heat stroke and heat exhaustion
- Blood transfusions
- Granulomatous diseases
Symptoms Associated with Fever
Fever rarely occurs in isolation and is often accompanied by various symptoms that can help identify the underlying cause. Recognizing these associated symptoms is crucial for accurate diagnosis and appropriate treatment.
General Symptoms
- Chills and Rigors Chills are sensations of coldness accompanied by shivering, which occurs as the body tries to generate heat to reach the new temperature set point. Rigors are more intense episodes of shivering and teeth chattering that often accompany high fevers. Chills and rigors are commonly seen in bacterial infections, malaria, and other serious infections.
- Sweating Sweating typically occurs when the fever “breaks” or begins to resolve. As the hypothalamus resets the temperature set point back to normal, the body dissipates excess heat through sweating. This can result in drenching sweats that may soak clothing and bedding.
- Fatigue and Malaise Fever increases the body’s metabolic rate and energy expenditure, leading to fatigue and a general feeling of illness (malaise). These symptoms are common with many infectious and inflammatory conditions.
- Headache Headache frequently accompanies fever and can range from mild to severe. The mechanisms include the effects of inflammatory mediators on blood vessels, dehydration, and direct effects of infections or inflammatory conditions on the central nervous system.
- Muscle and Joint Aches Myalgia (muscle aches) and arthralgia (joint pains) are common with fever, particularly in viral infections like influenza and COVID-19. These symptoms result from the effects of inflammatory mediators on muscles and joints.
Respiratory Symptoms
- Cough Cough often accompanies fever in respiratory infections such as the common cold, influenza, pneumonia, and bronchitis. The characteristics of the cough (dry or productive) can provide clues about the underlying cause.
- Sore Throat Throat pain or irritation is common with fever in conditions like strep throat, infectious mononucleosis, and viral upper respiratory infections.
- Nasal Congestion and Discharge Nasal symptoms often accompany fever in upper respiratory infections, allergic rhinitis, and sinusitis.
- Shortness of Breath Difficulty breathing or shortness of breath with fever can indicate more serious conditions such as pneumonia, pulmonary embolism, or heart failure.
Gastrointestinal Symptoms
- Nausea and Vomiting Nausea and vomiting often accompany fever in gastrointestinal infections, systemic infections, and conditions that increase intracranial pressure.
- Abdominal Pain Abdominal pain with fever can indicate infections of the gastrointestinal tract, urinary tract, or abdominal organs, as well as inflammatory conditions like appendicitis, pancreatitis, or inflammatory bowel disease.
- Diarrhea Diarrhea commonly accompanies fever in gastrointestinal infections caused by viruses, bacteria, or parasites.
- Loss of Appetite Decreased appetite is a common symptom with fever, resulting from the effects of inflammatory mediators on the digestive system and the body’s prioritization of energy for immune function.
Neurological Symptoms
- Altered Mental Status Changes in mental status, including confusion, lethargy, or irritability, can occur with high fevers, especially in very young children, older adults, and individuals with compromised immune systems. These symptoms may indicate central nervous system involvement or systemic illness.
- Neck Stiffness Neck stiffness (nuchal rigidity) with fever can indicate meningitis, a serious infection of the membranes surrounding the brain and spinal cord. This symptom requires immediate medical attention.
- Photophobia Sensitivity to light (photophobia) often accompanies fever in conditions like meningitis, encephalitis, and migraines.
- Seizures Febrile seizures can occur in young children with high fevers, typically between the ages of 6 months and 5 years. While usually benign, febrile seizures can be frightening for parents and require medical evaluation.
Skin Symptoms
- Rash Various types of rashes can accompany fever, providing important diagnostic clues:
- Maculopapular rash (flat, red spots with small bumps) seen in viral infections like measles and rubella
- Petechial rash (small, red or purple spots caused by bleeding under the skin) seen in meningococcemia and other serious infections
- Vesicular rash (fluid-filled blisters) seen in chickenpox and shingles
- Erythema migrans (bull’s-eye rash) seen in Lyme disease
- Palmar or plantar rash seen in coxsackievirus infection (hand-foot-mouth disease)
- Skin Warmth and Flushing During fever, the skin may feel warm and appear flushed due to increased blood flow to the skin surface as the body attempts to dissipate heat.
- Dry Skin Fever can lead to dehydration, which may cause dry skin and mucous membranes.
Cardiovascular Symptoms
- Increased Heart Rate Fever typically causes an increase in heart rate (tachycardia), with the heart rate increasing by approximately 10 beats per minute for each 1°C (1.8°F) rise in temperature.
- Low Blood Pressure In severe infections or sepsis, fever may be accompanied by low blood pressure (hypotension), which can indicate a serious condition requiring immediate medical attention.
Urinary Symptoms
- Painful Urination Pain or burning during urination (dysuria) with fever can indicate a urinary tract infection or sexually transmitted infection.
- Increased Urinary Frequency Needing to urinate more frequently than usual (frequency) along with fever can suggest a urinary tract infection or conditions like diabetes insipidus.
- Changes in Urine Appearance Cloudy, bloody, or foul-smelling urine with fever can indicate a urinary tract infection or kidney involvement.
Diagnosis of Fever
Diagnosing the cause of fever requires a systematic approach that includes a thorough medical history, physical examination, and potentially various diagnostic tests. The diagnostic process aims to identify the underlying cause to guide appropriate treatment.
Medical History
A detailed medical history is the cornerstone of fever diagnosis. Healthcare providers will typically ask about:
- Fever Characteristics
- Temperature measurements and how they were taken (oral, rectal, axillary, tympanic)
- Duration of fever
- Pattern of fever (continuous, intermittent, remittent, relapsing)
- Response to fever-reducing medications
- Associated symptoms (chills, sweats, headache, etc.)
- Recent Exposures
- Travel history (including specific regions and activities)
- Contact with sick individuals
- Exposure to animals or insects
- Occupational or environmental exposures
- Recent hospitalizations or medical procedures
- Food history (potential sources of foodborne illness)
- Medical History
- Pre-existing medical conditions
- Recent illnesses or surgeries
- Immunization history
- Allergies
- Medication history (prescription, over-the-counter, supplements)
- Social History
- Tobacco, alcohol, and substance use
- Sexual history
- Living situation
- Travel history
Physical Examination
A comprehensive physical examination provides valuable information to help diagnose the cause of fever:
- Vital Signs
- Temperature measurement using appropriate method
- Heart rate and rhythm
- Respiratory rate and effort
- Blood pressure
- Oxygen saturation
- General Appearance
- Level of alertness and orientation
- Signs of distress or discomfort
- Nutritional status
- Hydration status
- Skin Examination
- Temperature and color of the skin
- Presence of rash, lesions, or petechiae
- Signs of jaundice or cyanosis
- Turgor to assess hydration
- Head and Neck Examination
- Examination of the eyes for conjunctivitis, photophobia, or other abnormalities
- Examination of the ears for otitis media or other infections
- Examination of the nose and sinuses for congestion, discharge, or tenderness
- Examination of the throat for erythema, exudate, or other abnormalities
- Assessment of cervical lymph nodes for enlargement or tenderness
- Evaluation for neck stiffness
- Chest Examination
- Inspection of chest shape and movement
- Palpation for tenderness or crepitus
- Percussion to assess for dullness or hyperresonance
- Auscultation to listen for abnormal breath sounds (wheezes, crackles, diminished breath sounds)
- Cardiovascular Examination
- Assessment of heart sounds, murmurs, rubs, or gallops
- Evaluation of peripheral pulses
- Examination for peripheral edema
- Abdominal Examination
- Inspection for distension or abnormal contours
- Auscultation of bowel sounds
- Palpation for tenderness, masses, or organomegaly
- Percussion for tenderness or abnormal dullness
- Neurological Examination
- Assessment of mental status
- Cranial nerve examination
- Motor and sensory examination
- Reflex testing
- Evaluation for signs of meningeal irritation
- Musculoskeletal Examination
- Assessment of joint swelling, warmth, or tenderness
- Evaluation of range of motion
- Examination for muscle tenderness or weakness
Diagnostic Tests
Depending on the findings from the history and physical examination, various diagnostic tests may be ordered:
- Laboratory Tests
- Complete blood count (CBC): Can show signs of infection (elevated white blood cell count), anemia, or other abnormalities
- Blood cultures: To identify bacteria or fungi in the bloodstream
- Inflammatory markers: C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) to assess inflammation
- Comprehensive metabolic panel: To evaluate electrolyte balance, kidney and liver function, and glucose levels
- Urinalysis and urine culture: To identify urinary tract infections
- Sputum culture: For respiratory infections with productive cough
- Stool studies: For gastrointestinal infections
- Serologic tests: To detect antibodies against specific pathogens
- Arterial blood gas: To assess oxygenation and acid-base status in severe illness
- Imaging Studies
- Chest X-ray: To evaluate for pneumonia, lung abscess, or other pulmonary conditions
- Computed tomography (CT): Provides more detailed images of the chest, abdomen, or other areas as needed
- Ultrasound: Useful for evaluating abdominal organs, soft tissues, or detecting fluid collections
- Magnetic resonance imaging (MRI): Provides detailed images of soft tissues, particularly useful for neurological conditions
- Echocardiogram: To evaluate for heart valve abnormalities or vegetations in suspected infective endocarditis
- Specialized Tests
- Lumbar puncture: To obtain cerebrospinal fluid for analysis in suspected meningitis or encephalitis
- Biopsy: To obtain tissue samples for histological examination in suspected malignancies or granulomatous diseases
- Electrocardiogram (ECG): To assess for cardiac involvement or arrhythmias
- Tuberculin skin test or interferon-gamma release assay: To screen for tuberculosis
- Polymerase chain reaction (PCR) tests: To detect specific genetic material of pathogens
- Antigen tests: To detect specific proteins from pathogens
Diagnostic Algorithms
Healthcare providers often follow diagnostic algorithms based on the duration of fever and associated symptoms:
- Acute Fever Algorithm For acute fevers (less than one week), the focus is on identifying common causes such as respiratory infections, urinary tract infections, or gastroenteritis. Diagnostic testing is targeted based on symptoms and physical examination findings.
- Subacute Fever Algorithm For subacute fevers (1-2 weeks), a broader range of conditions is considered, including evolving infections, early stages of inflammatory conditions, or medication reactions. More extensive testing may be warranted.
- Fever of Unknown Origin (FUO) Algorithm Fever of unknown origin is defined as fever lasting more than three weeks with no apparent cause despite initial investigation. A systematic approach is used, including:
- Repeated history and physical examination
- Standard laboratory tests
- Imaging studies (CT, MRI)
- Specialized tests as indicated
- Consideration of less common causes
- Sometimes, empiric treatment or observation may be necessary
Differential Diagnosis