What are Cardiac Channel Blockers and their Role of in Preventing Heart Attacks
Introduction
The human heart, a remarkable organ that beats approximately 100,000 times each day, relies on a complex electrical system to maintain its rhythm and function. At the core of this system are ion channels, specialized proteins that control the flow of ions in and out of cardiac cells. When these channels malfunction or become overactive, various heart conditions can arise. Cardiac channel blockers, also known as ion channel blockers, represent a critical class of medications designed to modulate these channels, helping to restore normal heart function and prevent life-threatening arrhythmias. This comprehensive guide explores the fascinating world of cardiac channel blockers, their mechanisms, applications, and important considerations for patients and healthcare providers alike.
What Are Cardiac Channel Blockers?
Cardiac channel blockers are medications that selectively inhibit the function of specific ion channels in cardiac tissue. These channels are responsible for generating and propagating electrical impulses that coordinate heart contractions. By blocking these channels, these medications can alter the heart’s electrical activity, slowing down conduction, reducing automaticity, or prolonging repolarization, depending on which channels they target.
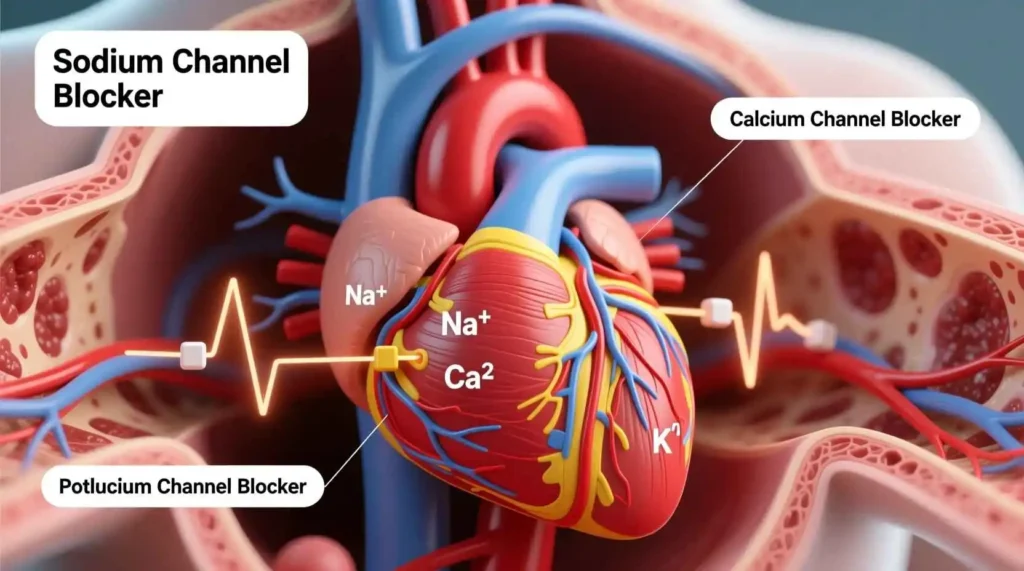
The heart’s electrical system depends on several key ions: sodium, potassium, calcium, and chloride. Each plays a distinct role in the cardiac action potential—the sequence of electrical changes that occur with each heartbeat. Sodium channels primarily drive the rapid depolarization phase, calcium channels sustain the plateau phase, and potassium channels are responsible for repolarization. Cardiac channel blockers are classified based on which ion channels they primarily affect.
These medications have revolutionized the treatment of cardiac arrhythmias, hypertension, angina, and other cardiovascular conditions. They work by fine-tuning the heart’s electrical activity, either by slowing down rapid heart rates, correcting irregular rhythms, or reducing the heart’s workload. Understanding how these medications work at the molecular level provides insight into their therapeutic effects and potential side effects.
Types of Cardiac Channel Blockers
Cardiac channel blockers are categorized into several classes based on their specific targets and mechanisms of action. The primary classifications include sodium channel blockers, calcium channel blockers, potassium channel blockers, and multichannel blockers. Each class has distinct properties and clinical applications.
Sodium Channel Blockers
Sodium channel blockers, also known as Class I antiarrhythmics, inhibit the fast sodium channels responsible for the rapid depolarization phase of the cardiac action potential. By slowing the influx of sodium ions, these medications decrease the conduction velocity through the heart and reduce the excitability of cardiac tissue. Sodium channel blockers are further subdivided into three subclasses:
- Class IA: These medications moderately block sodium channels and also prolong repolarization by blocking potassium channels. Examples include quinidine, procainamide, and disopyramide. They are effective for both atrial and ventricular arrhythmias but carry a risk of QT prolongation and torsades de pointes.
- Class IB: These medications have fast-on, fast-off kinetics, meaning they bind to and unbind from sodium channels quickly. They primarily affect ischemic or depolarized tissue. Examples include lidocaine, mexiletine, and tocainide. They are particularly useful for ventricular arrhythmias, especially those occurring after a heart attack.
- Class IC: These medications potently block sodium channels with slow binding kinetics, significantly slowing conduction throughout the heart. Examples include flecainide, propafenone, and moricizine. They are effective for supraventricular tachycardias and atrial fibrillation but are generally avoided in patients with structural heart disease due to proarrhythmic risks.
Calcium Channel Blockers
Calcium channel blockers inhibit L-type calcium channels, which are crucial for the plateau phase of the cardiac action potential and for excitation-contraction coupling in cardiac and smooth muscle. By reducing calcium influx, these medications decrease heart rate, slow conduction through the AV node, and relax vascular smooth muscle. Calcium channel blockers are divided into two main groups:
- Non-dihydropyridines: These medications have significant effects on the heart, slowing heart rate and AV nodal conduction. Examples include verapamil and diltiazem. They are particularly useful for rate control in atrial fibrillation, hypertension, and angina.
- Dihydropyridines: These medications primarily affect vascular smooth muscle, causing vasodilation with minimal direct cardiac effects. Examples include amlodipine, nifedipine, and felodipine. They are primarily used for hypertension and angina but may cause reflex tachycardia due to their vasodilatory effects.
Potassium Channel Blockers
Potassium channel blockers, also known as Class III antiarrhythmics, inhibit various potassium channels responsible for repolarization. By delaying repolarization, these medications prolong the action potential duration and effective refractory period. This effect helps prevent re-entrant arrhythmias by creating a longer window during which the heart tissue is unexcitable. Examples include:
- Amiodarone: A multichannel blocker that also has sodium, calcium, and beta-blocking effects. It is highly effective for a wide range of atrial and ventricular arrhythmias but has a significant side effect profile.
- Sotalol: A beta-blocker with additional Class III properties. It is used for atrial fibrillation and ventricular tachycardias but carries a risk of QT prolongation and torsades de pointes.
- Dofetilide: A pure potassium channel blocker used specifically for atrial fibrillation and flutter. It requires careful monitoring due to its proarrhythmic potential.
- Ibutilide: Used for acute conversion of atrial fibrillation and flutter. It has a rapid onset but also a significant risk of torsades de pointes.
Multichannel Blockers
Some medications affect multiple ion channels simultaneously, offering broader antiarrhythmic effects. Amiodarone is the most notable example, blocking sodium, potassium, and calcium channels while also exhibiting beta-blocking properties. This multichannel activity makes it effective for a wide range of arrhythmias but also contributes to its complex side effect profile. Other multichannel blockers include dronedarone (a derivative of amiodarone with fewer side effects but less efficacy) and ranolazine (primarily used for chronic angina but also has antiarrhythmic properties).
Mechanism of Action
The therapeutic effects of cardiac channel blockers stem from their ability to modulate ion flow across cardiac cell membranes. To understand their mechanism of action, it’s essential to first grasp the cardiac action potential—the sequence of electrical changes that occur with each heartbeat.
The Cardiac Action Potential
The cardiac action potential consists of several phases:
- Phase 0: Rapid depolarization, primarily driven by the influx of sodium ions through fast sodium channels. This phase represents the rapid upstroke of the action potential.
- Phase 1: Early repolarization, characterized by a brief decrease in membrane potential due to inactivation of sodium channels and activation of transient potassium currents.
- Phase 2: Plateau phase, maintained by the balance between inward calcium currents and outward potassium currents. This phase is unique to cardiac muscle and prolongs the action potential, allowing for coordinated contraction.
- Phase 3: Rapid repolarization, driven by the inactivation of calcium channels and activation of delayed rectifier potassium channels.
- Phase 4: Resting membrane potential, maintained by the sodium-potassium pump and inward rectifier potassium channels. In pacemaker cells, this phase shows spontaneous depolarization due to funny currents.
How Channel Blockers Alter the Action Potential
Cardiac channel blockers exert their effects by interfering with specific phases of the action potential:
- Sodium channel blockers primarily affect Phase 0, reducing the slope and amplitude of depolarization. This slows conduction velocity throughout the heart, particularly in the His-Purkinje system and ventricular muscle. The degree of blockade depends on the heart rate and the resting membrane potential, with greater effects at faster rates and in depolarized tissue (use-dependence).
- Calcium channel blockers mainly influence Phase 2, reducing the plateau duration and amplitude. In nodal tissue (SA and AV nodes), where calcium currents play a dominant role in depolarization, these medications decrease automaticity and slow conduction. In vascular smooth muscle, they reduce calcium influx, leading to vasodilation.
- Potassium channel blockers primarily affect Phase 3, delaying repolarization and prolonging the action potential duration. This increases the effective refractory period, making it harder for re-entrant circuits to sustain themselves. However, excessive prolongation can lead to early afterdepolarizations and torsades de pointes.
Use-Dependence and State-Dependence
Many cardiac channel blockers exhibit use-dependence, meaning their blocking effects are more pronounced at faster heart rates. This property is therapeutically advantageous as it allows these medications to suppress tachyarrhythmias while having minimal effects on normal heart rates. The mechanism involves the drug binding more effectively to channels in the open or inactivated states, which occur more frequently during rapid firing.
State-dependence refers to the preferential binding of a drug to channels in specific conformational states (resting, open, or inactivated). For example, sodium channel blockers like lidocaine bind more strongly to inactivated sodium channels, which are more prevalent in ischemic or depolarized tissue. This makes them particularly effective for treating arrhythmias in damaged myocardium while sparing healthy tissue.
Effects on Cardiac Conduction and Refractoriness
By altering ion channel function, cardiac channel blockers produce several electrophysiological effects:
- Slowed conduction velocity: Sodium channel blockers decrease the speed of electrical impulse propagation through the heart, which can interrupt re-entrant circuits.
- Prolonged refractory period: Potassium channel blockers extend the time during which cardiac cells cannot be re-excited, preventing rapid re-firing.
- Reduced automaticity: Calcium channel blockers decrease the spontaneous firing rate of pacemaker cells, particularly in the SA and AV nodes.
- Altered contractility: Calcium channel blockers reduce the force of cardiac contraction by decreasing calcium influx during the plateau phase.
These effects collectively contribute to the antiarrhythmic, antihypertensive, and antianginal properties of cardiac channel blockers.
Clinical Uses
Cardiac channel blockers have diverse clinical applications, ranging from life-threatening arrhythmias to chronic conditions like hypertension and angina. Their use is guided by the specific ion channels they target and their resulting electrophysiological effects.
Arrhythmia Management
One of the primary uses of cardiac channel blockers is in the treatment of cardiac arrhythmias. Different types of arrhythmias respond to different classes of channel blockers:
- Supraventricular tachycardias (SVTs): Calcium channel blockers (verapamil, diltiazem) are first-line treatments for acute termination of AV nodal re-entrant tachycardia (AVNRT) and AV re-entrant tachycardia (AVRT). They work by slowing conduction through the AV node, interrupting the re-entrant circuit. Sodium channel blockers (flecainide, propafenone) are also effective, particularly for atrial fibrillation and flutter.
- Atrial fibrillation and flutter: For rate control, calcium channel blockers (diltiazem, verapamil) and beta-blockers are preferred. For rhythm control, sodium channel blockers (flecainide, propafenone) and potassium channel blockers (amiodarone, sotalol, dofetilide) may be used. Amiodarone is particularly effective for maintaining sinus rhythm in patients with structural heart disease.
- Ventricular arrhythmias: Sodium channel blockers (lidocaine, mexiletine) are used for acute ventricular tachycardia, especially in the setting of ischemia. Potassium channel blockers (amiodarone, sotalol) are used for both acute and chronic management of ventricular tachycardia and fibrillation. Implantable cardioverter-defibrillators (ICDs) are often used in conjunction with antiarrhythmic drugs for secondary prevention.
- Long QT syndrome: Potassium channel blockers are generally avoided in patients with congenital long QT syndrome as they can exacerbate the condition. Instead, beta-blockers are first-line, with sodium channel blockers (mexiletine) sometimes used for specific subtypes.
Hypertension Management
Calcium channel blockers, particularly dihydropyridines like amlodipine, are widely used for hypertension management. They work by relaxing vascular smooth muscle, reducing peripheral vascular resistance, and lowering blood pressure. Non-dihydropyridine calcium channel blockers (verapamil, diltiazem) are also effective but are typically reserved for patients who also have angina or certain arrhythmias.
Calcium channel blockers are especially useful in specific patient populations:
- Elderly patients: They are well-tolerated and effective in isolated systolic hypertension.
- African American patients: They tend to respond better to calcium channel blockers and diuretics than to ACE inhibitors or ARBs.
- Patients with comorbid conditions: They are beneficial in patients with concomitant angina or Raynaud’s phenomenon.
Angina Pectoris
Calcium channel blockers are effective for both stable and unstable angina. Their antianginal effects stem from several mechanisms:
- Vasodilation of coronary arteries: They improve myocardial oxygen supply by dilating epicardial coronary arteries and preventing coronary vasospasm.
- Reduction of cardiac workload: They decrease myocardial oxygen demand by lowering blood pressure and reducing contractility (non-dihydropyridines).
- Prevention of vasospasm: They are particularly effective for variant (Prinzmetal’s) angina, which is caused by coronary artery spasm.
Sodium channel blockers like ranolazine are also used for chronic angina, particularly in patients who remain symptomatic despite conventional therapy. Ranolazine works by inhibiting the late sodium current, which reduces intracellular calcium overload and improves myocardial efficiency.
Other Cardiovascular Conditions
Cardiac channel blockers have several other important clinical applications:
- Hypertrophic cardiomyopathy: Calcium channel blockers (verapamil) and disopyramide (a Class IA sodium channel blocker) are used to improve symptoms by reducing left ventricular outflow tract obstruction and improving diastolic filling.
- Heart rate control: Calcium channel blockers (diltiazem, verapamil) are used for heart rate control in various tachyarrhythmias, including atrial fibrillation and inappropriate sinus tachycardia.
- Migraine prophylaxis: Verapamil is sometimes used for migraine prevention, particularly in patients who cannot tolerate beta-blockers.
- Raynaud’s phenomenon: Calcium channel blockers (nifedipine, amlodipine) are first-line treatments for reducing the frequency and severity of vasospastic attacks.
Benefits and Efficacy
Cardiac channel blockers offer numerous benefits in the management of cardiovascular diseases, backed by extensive clinical evidence. Their efficacy varies depending on the specific condition, patient population, and individual drug characteristics.
Efficacy in Arrhythmia Management
Cardiac channel blockers have demonstrated significant efficacy in controlling various arrhythmias:
- Atrial fibrillation: Calcium channel blockers (diltiazem, verapamil) effectively control ventricular rate in 70-80% of patients with atrial fibrillation. For rhythm control, flecainide and propafenone maintain sinus rhythm in 50-70% of patients at one year, while amiodarone is effective in up to 70% of patients but with higher discontinuation rates due to side effects.
- Ventricular arrhythmias: Amiodarone is the most effective antiarrhythmic for ventricular tachycardia and fibrillation, reducing arrhythmia recurrence by 60-70% and sudden cardiac death by 40-50% in patients with structural heart disease. Lidocaine terminates acute ventricular tachycardia in 70-80% of cases, particularly in the setting of ischemia.
- Supraventricular tachycardias: Verapamil and adenosine have comparable efficacy in terminating AVNRT and AVRT, with success rates exceeding 90%. Flecainide and propafenone are also highly effective, with success rates of 85-95% for acute termination and long-term prevention.
Blood Pressure Control
Calcium channel blockers are among the most effective antihypertensive agents:
- Monotherapy efficacy: Amlodipine reduces systolic blood pressure by 15-20 mmHg and diastolic blood pressure by 8-12 mmHg as monotherapy, with response rates of 50-60% at standard doses.
- Combination therapy: When combined with ACE inhibitors or ARBs, calcium channel blockers achieve blood pressure control in 70-80% of patients with hypertension.
- Cardiovascular outcomes: Large clinical trials like ALLHAT and ASCOT have demonstrated that calcium channel blockers reduce stroke risk by 30-40% and cardiovascular events by 15-20% compared to placebo, with similar efficacy to other first-line antihypertensives.
Angina Relief





