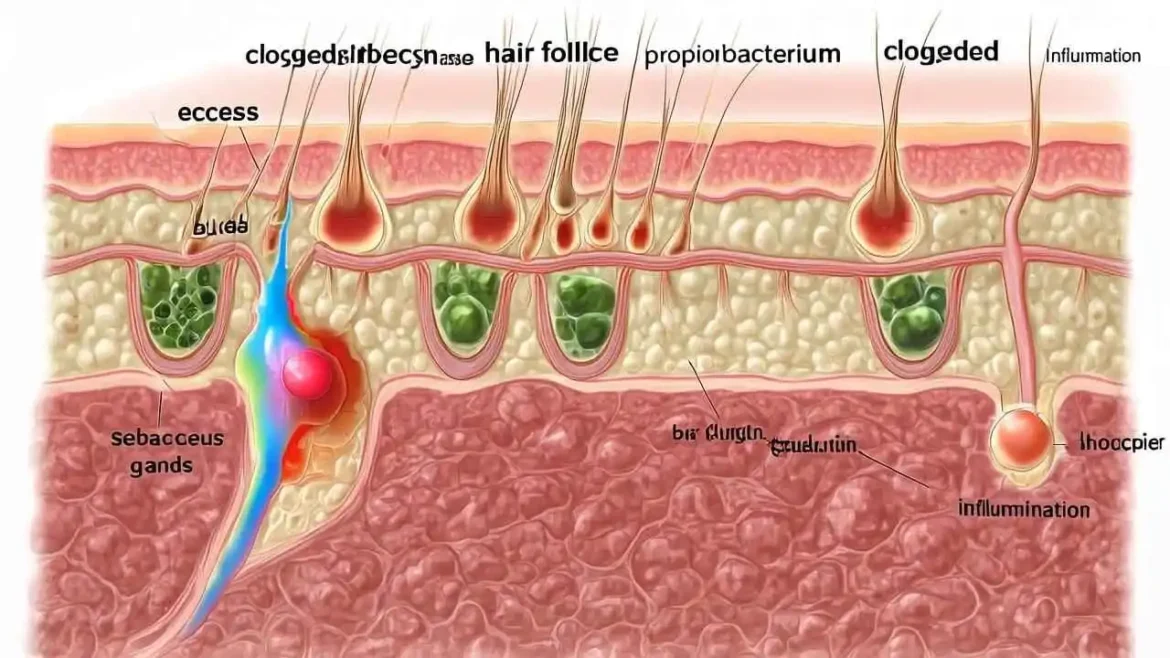
While the four core mechanisms – excessive sebum production, follicular hyperkeratinization, Cutibacterium acnes (formerly Propionibacterium acnes) proliferation, and inflammation – are universally at play in the development of acne vulgaris, a diverse array of external and internal factors can significantly influence, exacerbate, or even trigger its onset. It’s crucial to understand that these are primarily contributing factors, not direct, sole causes, and their individual impact varies profoundly from person to person, highlighting the highly individualized nature of acne.
Let’s delve deeper into these influences:
- Hormonal Fluctuations: Hormones, particularly androgens, are pivotal in regulating sebaceous gland activity. During puberty, a surge in androgens like testosterone and dehydroepiandrosterone sulfate (DHEA-S) directly stimulates the sebaceous glands to enlarge and produce more sebum. This increased oil production creates an ideal environment for acne development. In women, hormonal acne commonly manifests during specific life stages or in response to cyclical changes:
- Menstrual Cycle: Many women experience pre-menstrual flares due as hormonal shifts, particularly a relative increase in androgenic activity or sensitivity, can lead to increased oil production and inflammation in the days leading up to menstruation.
- Pregnancy: The fluctuating and elevated hormone levels during pregnancy can either improve or worsen acne, depending on the individual’s hormonal response.
- Polycystic Ovary Syndrome (PCOS): This common endocrine disorder is characterized by elevated androgen levels, often driven by insulin resistance, which leads to exaggerated sebum production, increased facial and body hair (hirsutism), and persistent acne.
- Perimenopause and Menopause: Hormonal shifts during these periods can also lead to acne flare-ups, often termed “adult-onset acne.”
- Genetics: A significant genetic predisposition exists for acne. If one or both of your parents experienced acne, particularly severe forms, you have a substantially higher likelihood of developing it yourself. Genetics can influence a multitude of factors related to acne pathogenesis, including:
- Sebum Production Levels: Inherited differences in the size and activity of sebaceous glands.
- Follicular Hyperkeratinization: The propensity for skin cells to shed abnormally and clump together, blocking pores.
- Immune Response: The intensity of the inflammatory response to Cutibacterium acnes and other triggers.
- Hormone Receptor Sensitivity: How readily sebaceous glands respond to circulating hormone levels.
- Skin Barrier Function: Inherited differences in the skin’s protective barrier, impacting its susceptibility to irritation and inflammation.
- Diet: Mounting evidence increasingly suggests a link between certain dietary patterns and the exacerbation of acne, primarily by influencing systemic inflammation and hormone levels.
- High-Glycemic-Index (HGI) Foods: Diets rich in refined carbohydrates and sugary foods (e.g., white bread, sugary snacks, sweetened beverages) cause rapid spikes in blood sugar. This leads to increased insulin and Insulin-like Growth Factor 1 (IGF-1) levels. Both insulin and IGF-1 can stimulate sebaceous gland activity and keratinocyte proliferation, thereby promoting comedone formation and inflammation.
- Dairy Products: For some individuals, consumption of dairy, particularly skim milk, has been associated with worsened acne. This link is thought to be due to hormones naturally present in milk (e.g., certain growth factors) and whey protein, which can also influence insulin/IGF-1 pathways. The evidence is less consistent than for HGI foods, and individual sensitivity varies greatly.
- Other Potential Triggers: While less definitively proven, some individuals report sensitivities to specific foods like certain types of chocolate (though the scientific evidence is weak) or excessive saturated fats. The focus is generally shifting towards a more holistic, anti-inflammatory dietary approach rich in whole foods, fruits, vegetables, and lean proteins, which may help improve overall skin health.
- Stress: While stress does not directly cause acne, it can significantly worsen existing conditions. When we are stressed, our bodies release a cascade of hormones, fundamentally cortisol and other stress-related neuropeptides. These hormones have a direct impact on sebaceous glands, increasing sebum output. Furthermore, stress can compromise the skin barrier function, making it more susceptible to inflammation and bacterial colonization. The relationship can become a vicious cycle: stress triggers acne flares, and the presence of acne can, in turn, cause emotional distress, leading to more stress and potentially more breakouts. Effective stress management techniques, such as mindfulness, regular exercise, and adequate sleep, can therefore play a supportive role in acne management.
- Medications: Certain systemic medications can have acne as a side effect or can exacerbate pre-existing acne. These include:
- Corticosteroids: Both oral and topical corticosteroids can trigger steroid-induced acne, which often presents as uniform small bumps.
- Androgens and Anabolic Steroids: Used in hormone replacement therapy or by athletes, these can significantly increase sebum production.
- Lithium: Used to treat bipolar disorder.
- Certain Anticonvulsants: Such as phenytoin or phenobarbital.
- Some Anti-Tuberculosis Drugs.
- High Doses of B Vitamins: Particularly B6 and B12, though this is less common.
- Immunosuppressants: Like cyclosporine. It is crucial for individuals on these medications to discuss any acne concerns with their prescribing doctor, as stopping medication without medical advice can be dangerous.
- Occlusive Products and Environmental Factors: External factors that block pores or create friction can contribute to acne:
- Comedogenic Cosmetics and Skincare: Heavy, pore-clogging ingredients commonly found in some makeup, moisturizers, sunscreens, and even hair products can trap dead skin cells and sebum, leading to the formation of comedones. Look for labels like “non-comedogenic” or “oil-free.”
- Hair Products: Greasy or heavy hair products (e.g., gels, pomades, waxes) can migrate onto the face, neck, and back, contributing to breakouts in those areas.
- Friction and Pressure (Acne Mechanica): Prolonged pressure or friction on the skin from tight clothing, helmets, headbands, backpacks, or even cell phones and face masks (“maskne”) can irritate follicles, cause micro-trauma, and lead to inflammation and breakouts.
Understanding these contributing factors is essential for developing a personalized and effective acne management strategy. Often, a multi-pronged approach that addresses both the underlying biological mechanisms and these influencing factors yields the best long-term results. Consulting with a dermatologist can help identify specific triggers and tailor treatment plans accordingly.
Navigating the landscape of acne treatment can often feel like a daunting and confusing journey. The most effective and sustainable path to clearer skin is frequently a tiered and systematic approach, starting with the most accessible and least intensive options, and gradually escalating to professional medical interventions only as necessary. This methodical strategy ensures that you’re giving your skin the best chance to respond to treatment without immediately resorting to more potent solutions.
A fundamental cornerstone of any acne regimen is consistency and patience. Unlike immediate remedies, skin cell turnover and the resolution of inflammation take time. It’s crucial to commit to a chosen treatment plan for a minimum of 6-8 weeks before expecting to see noticeable improvement. Giving products and prescribed medications adequate time to work is key to evaluating their efficacy.
As the text wisely states, “There is no single ‘cure’ for acne, but there is a vast and effective toolbox of treatments. The key is finding the right combination for the individual’s specific acne type and skin, which often requires professional guidance. What works for one person may not work for another.” This highlights the highly personal nature of acne treatment. Understanding your specific type of acne (whiteheads, blackheads, cysts, nodules) and your skin’s unique sensitivities is paramount, underscoring the value of consulting with a skincare professional.
Let’s delve deeper into each level of this tiered approach:
Level 1: Over-the-Counter (OTC) Solutions – The First Line of Defense
These readily available products are the initial step for individuals experiencing mild to moderate acne, offering effective solutions that target common acne causes.
- Benzoyl Peroxide (BP): This powerful ingredient works by introducing oxygen into the pore, which is toxic to the C. acnes (formerly P. acnes) bacteria, a primary contributor to inflammatory acne. Beyond its antibacterial properties, BP also acts as a peeling agent, helping to shed dead skin cells and clear out clogged pores. Available in various concentrations (from 2.5% to 10%), it’s effective but can cause dryness, redness, and even bleach fabrics.
- Salicylic Acid (BHA – Beta Hydroxy Acid): Unlike water-soluble exfoliants, salicylic acid is oil-soluble, allowing it to penetrate deep into pores filled with sebum and dead skin cells. It effectively dissolves this debris, making it incredibly effective for treating and preventing blackheads and whiteheads (comedones). It also has mild anti-inflammatory properties, making it suitable for congested, breakout-prone skin.
- Adapalene (e.g., Differin Gel): This is a third-generation topical retinoid that acts by normalizing skin cell turnover. This process helps prevent the formation of microcomedones (the earliest stage of an acne lesion) and ensures that pores remain clear. As a retinoid, it encourages healthy skin cell exfoliation from within the follicle, reducing clogging. Although available OTC, it’s a potent ingredient, and users should start slowly to minimize potential irritation like dryness and redness.
Level 2: Prescription Topical Treatments – Stepping Up for Persistent Acne
When OTC products fail to sufficiently clear acne, a dermatologist’s expertise becomes invaluable. They can prescribe stronger topical medications that target more persistent or moderate lesions.
- Topical Retinoids (e.g., Tretinoin, Tazarotene): These are more potent derivatives of Vitamin A than adapalene. Tretinoin (Retin-A, Renova) and Tazarotene (Tazorac) are highly effective at preventing comedones, reducing inflammation, and promoting healthy cell turnover. They can significantly improve skin texture and reduce hyperpigmentation over time. Due to their potency, they often cause initial dryness, redness, and sun sensitivity, necessitating careful introduction and diligent sunscreen use.
- Topical Antibiotics (e.g., Clindamycin, Erythromycin): These medications work by reducing the population of C. acnes bacteria on the skin and diminishing inflammation. They are particularly useful for inflammatory lesions like papules and pustules. To prevent bacterial resistance, which can render the antibiotic ineffective over time, dermatologists often prescribe them in combination with benzoyl peroxide. This synergistic approach ensures comprehensive bacterial control.
- Azelaic Acid: A versatile ingredient, azelaic acid boasts antibacterial, anti-inflammatory, and mild exfoliating properties. It’s particularly well-suited for individuals with sensitive skin who may not tolerate other strong actives. Furthermore, azelaic acid is known for its ability to reduce post-inflammatory hyperpigmentation (PIH) and post-inflammatory erythema (PIE), the red or dark marks left behind after acne lesions heal, making it a valuable addition for improving overall skin tone and texture.
Level 3: Oral Medications and Professional Procedures – Comprehensive Solutions for Severe or Recalcitrant Acne
For moderate to severe, widespread, or persistent acne that hasn’t responded to topical treatments, a dermatologist may recommend systemic medications or in-office procedures to tackle the root causes more aggressively.
- Oral Antibiotics (e.g., Doxycycline, Minocycline): These systemic medications reduce acne-causing bacteria throughout the body and, more importantly for acne, possess powerful anti-inflammatory effects. They are typically prescribed for a limited duration to bring widespread inflammation under control, often as a bridge to other long-term treatments, due to concerns about antibiotic resistance with prolonged use.
- Hormonal Therapies (e.g., Oral Contraceptives, Spironolactone): These treatments are particularly effective for women whose acne is primarily linked to hormonal fluctuations, often presenting as deeper, cystic lesions around the jawline, chin, and neck. Oral contraceptives work by regulating androgen (male hormone) activity, which can stimulate excess sebum production. Spironolactone, an anti-androgen medication, also helps to reduce oil production and improve hormonal acne.
- Isotretinoin (formerly Accutane): This is a highly potent oral retinoid considered the most effective treatment for severe, recalcitrant, or scarring nodulocystic acne that has not responded to other therapies. Isotretinoin uniquely addresses all four primary causes of acne: it significantly reduces sebum production, normalizes follicular keratinization (preventing clogged pores), reduces C. acnes bacteria, and possesses strong anti-inflammatory properties. Due to its efficacy and potential for significant side effects (such as severe dryness, muscle aches, and most critically, severe birth defects if taken during pregnancy), it requires strict medical supervision, including monthly blood tests and enrollment in a risk management program (like iPLEDGE in the U.S.) for female patients. Its transformative results often make it a life-changing treatment for those with severe acne.
Managing acne is a journey that often requires a dynamic and personalized approach. By understanding these tiered treatment options and working closely with a qualified dermatologist, individuals can effectively navigate their path to clearer, healthier skin, finding the right “toolbox” of solutions tailored to their unique needs.
Beyond the Bottle: Building a Supportive, Consistent Daily Skincare Routine for Healthy Skin
While targeted treatment products are undoubtedly powerful allies in the fight against acne, they represent only one crucial piece of a larger, more intricate puzzle. True, lasting success in managing breakouts and achieving overall skin health hinges on the unwavering commitment to a consistent, supportive daily skincare routine. This holistic approach not only maximizes the efficacy of your treatments but also nurtures your skin’s natural resilience, leading to long-term clarity and comfort.
Here are the fundamental pillars of such a routine:
- Cleanse Gently & Wisely: The foundation of any healthy skin routine begins with proper cleansing. Aim to wash your face no more than twice a day – once in the morning and once in the evening, and perhaps after a very sweaty workout – with a mild, non-stripping cleanser. The goal is to remove dirt, excess oil, makeup, and impurities without stripping away your skin’s natural protective oils, which are vital for maintaining a healthy barrier. Aggressive scrubbing, using harsh physical exfoliants, or over-washing can severely irritate the skin, disrupt its delicate microbiome, compromise its natural protective barrier, and paradoxically trigger more oil production and inflammation, potentially worsening acne breakouts and sensitivity. Always use lukewarm water and your fingertips, then gently pat your skin dry with a clean towel.
- Targeted Treatment Application: Once your skin is freshly cleansed and gently patted dry, it’s time for your active treatment. Whether you’re using an over-the-counter (OTC) spot treatment, a full-face topical medication, or a prescription-strength formula, always apply it precisely as directed by the product instructions or your dermatologist. Using too much, too little, or applying it incorrectly can diminish its effectiveness, increase the likelihood of unwanted side effects like redness or peeling, or simply waste product. Allow the treatment to fully absorb for a few minutes before proceeding to the next step, ensuring maximum penetration and efficacy.
- Embrace Essential Hydration (Moisturize): This step is absolutely non-negotiable, especially for acne-prone skin that is often subjected to drying treatments. Many acne medications, from retinoids and benzoyl peroxide to salicylic acid, can significantly dehydrate the skin, leading to flakiness, tightness, increased sensitivity, and even a compromised skin barrier. A non-comedogenic (meaning it won’t clog pores), lightweight moisturizer is your skin’s best friend. It acts as a protective shield, helping to repair and maintain the skin’s crucial moisture barrier, reduce redness and irritation, and significantly improve your skin’s tolerance to active treatments, allowing you to stay consistent. Apply it generously over your entire face and neck, ideally while your skin is still slightly damp from cleansing or after your treatment has absorbed, to lock in hydration effectively.
- Crucial Daily Sun Protection: Every single morning, without fail, conclude your routine with a generous application of a broad-spectrum sunscreen with an SPF of 30 or higher. This step is critically important for several reasons: Firstly, many common acne treatments (like retinoids, AHAs, and BHAs) increase your skin’s photosensitivity, making it much more vulnerable to sun damage, sunburn, and irritation. Secondly, sun exposure can significantly exacerbate and darken post-inflammatory hyperpigmentation (PIH) – the stubborn red, brown, or purple marks that blemishes often leave behind long after the breakout has healed. By consistently using sunscreen, you not only protect against harmful UVA/UVB rays and premature aging but also powerfully minimize the appearance and longevity of these unsightly dark spots, ensuring your skin heals more evenly and quickly. Reapply throughout the day if exposed to direct sunlight for extended periods.
The Power of Consistency and Patience:
Implementing these steps daily creates a synergistic effect, where each product supports the others, leading to healthier, clearer skin over time. Remember that results don’t happen overnight; consistency is paramount. Be patient with your skin, observe how it responds, and don’t hesitate to consult with a dermatologist for personalized advice and to ensure your routine is perfectly tailored to your unique skin needs. A well-constructed, supportive routine isn’t just about clearer skin; it’s about building confidence and fostering a healthier relationship with your skin every single day.
Acne vulgaris is a complex medical condition, not a reflection of personal failing. By understanding the underlying biology and the diverse range of available treatments, we empower ourselves to manage it effectively. The journey often requires trial, error, and immense patience. But with a consistent routine, the right combination of treatments, and, when necessary, the guidance of a dermatologist, we can move beyond the surface-level frustration and achieve clearer, healthier skin.
Sure! Here are 30 frequently asked questions (FAQs) on preventing Acne Vulgaris through natural remedies and lifestyle changes, along with their answers:
FAQs on Preventing Acne Vulgaris
- What is Acne Vulgaris?
- Acne Vulgaris is a common skin condition characterized by the presence of pimples, blackheads, and cysts. It occurs when hair follicles become clogged with oil and dead skin cells.
- Can diet affect Acne Vulgaris?
- Yes, certain foods can trigger acne. Diets high in processed sugars and dairy may exacerbate the condition, while a balanced diet rich in fruits, vegetables, and whole grains can help promote clear skin.
- What natural remedies are effective for preventing acne?
- Natural remedies include tea tree oil, aloe vera, green tea, and honey. These have antibacterial and anti-inflammatory properties that may help reduce acne.
- Is it important to keep the skin clean to prevent acne?
- Yes, maintaining proper skin hygiene by cleansing your face twice a day with a mild cleanser can help remove excess oil, dirt, and bacteria.
- How does hydration affect acne?
- Drinking enough water keeps the skin hydrated and may help regulate oil production, reducing the likelihood of clogged pores.
- What lifestyle changes can help prevent Acne Vulgaris?
- Regular exercise, sufficient sleep, stress management, and avoiding touching your face can be beneficial in preventing acne.
- Can stress cause acne flare-ups?
- Yes, stress can lead to hormonal changes that may increase oil production and trigger breakouts.
- Should I avoid makeup if I have acne-prone skin?
- While it may not be necessary to avoid makeup completely, opting for non-comedogenic and oil-free products can help prevent clogged pores.
- Does over-exwashing contribute to acne?
- Yes, overwashing can strip the skin of its natural oils, leading to irritation and increased oil production, which may worsen acne.
- How can I utilize essential oils to combat acne?
- Certain essential oils, like lavender and tea tree oil, can be diluted with a carrier oil and applied topically for their antibacterial and calming properties.
- Is sun exposure beneficial for acne-prone skin?
- Moderate sun exposure can dry out some acne, but excessive sun can cause skin damage and lead to post-inflammatory hyperpigmentation. Always use sunscreen.
- Can consuming probiotics help with acne?
- Yes, probiotics can promote gut health, which may influence skin health and reduce inflammation related to acne.
- Is there a link between dairy consumption and acne?
- Some studies suggest that dairy products, particularly skim milk, may be associated with acne development in some individuals.
- Can chocolate contribute to acne?
- While chocolate itself doesn’t directly cause acne, it may exacerbate existing conditions in some people, especially those sensitive to sugar or dairy in chocolate products.
- How important is sleep for preventing acne?
- Quality sleep is crucial as it helps regulate hormones, supports skin repair, and mitigates stress, all of which can impact acne.
- Is it true that certain vitamins can help improve acne?
- Vitamins A, C, D, and E, as well as zinc, may contribute to skin health and help manage acne. A balanced diet can help you get these vitamins.
- Can apple cider vinegar be used for acne prevention?
- Yes, diluted apple cider vinegar may have antibacterial properties and can be used as a toner; however, it should be patch-tested first to avoid irritation.
- What role does regular physical activity play in acne prevention?
- Exercise helps reduce stress, improves circulation, and can help regulate hormones, all of which may help in preventing acne.
- How can I manage hormonal acne?
- Hormonal acne can be managed through lifestyle changes, stress reduction, and possibly dietary adjustments. Consult a healthcare provider for personalized advice.
- Can I use natural exfoliants for acne prevention?
- Yes, natural exfoliants like sugar, coffee grounds, or oatmeal can help remove dead skin cells, promoting clearer skin when used gently and not excessively.
- Are there any herbs recommended for acne treatment?
- Herbs like spearmint, turmeric, and neem have anti-inflammatory and antibacterial properties that may aid in preventing acne.
- Is it safe to pop pimples?
- Popping pimples can lead to scarring and further infection. It is generally not recommended; instead, let them heal naturally.
- How does smoking affect acne?
- Smoking can impair circulation and oxygen delivery to the skin, leading to a variety of skin issues, including acne.
- Should I change my pillowcase frequently to prevent acne?
- Yes, changing your pillowcase regularly can reduce the transfer of oil, bacteria, and dead skin cells that can clog pores.
- What are some signs that I might have acne-prone skin?
- Oily skin, frequent breakouts, and enlarged pores are common signs of acne-prone skin.
- Does drinking green tea help with acne?
- Green tea contains antioxidants and anti-inflammatory properties that may help reduce acne and improve overall skin health.
- Should I consult a dermatologist for persistent acne?
- Yes, if you experience persistent or severe acne, it’s important to consult a dermatologist for proper diagnosis and treatment options tailored to your needs.
- Can quitting birth control pills lead to acne?
- Yes, stopping hormonal contraceptives can lead to hormonal fluctuations that may trigger acne flare-ups in some individuals.
- How does sugar intake impact acne?
- High sugar intake can spike insulin levels, leading to increased oil production and inflammation—both of which can worsen acne.
- Is it helpful to keep a skincare diary for acne management?
- Yes, tracking your skincare routine, diet, and lifestyle factors can help identify triggers and effective treatments for preventing acne.
Conclusion
These FAQs provide a comprehensive overview of natural remedies and lifestyle changes that can help in preventing Acne Vulgaris. It’s important to remember that individual results may vary, and consulting with a healthcare professional is advisable for personalized advice.
Medical Disclaimer:
The information provided on this website is for general educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.