How MRI Scans Work: Understanding the Technology Behind Different MRI Types
Introduction
Magnetic Resonance Imaging, commonly known as MRI, represents one of the most significant advancements in medical imaging technology over the past century. Since its clinical introduction in the 1980s, MRI has revolutionized diagnostic medicine, providing unparalleled visualization of soft tissues within the human body without exposing patients to ionizing radiation. This non-invasive imaging technique utilizes powerful magnetic fields and radio waves to generate detailed images of organs, tissues, and other internal body structures, offering critical insights for diagnosis, treatment planning, and monitoring of various medical conditions.
The versatility of MRI technology has led to the development of numerous specialized imaging sequences and techniques, each designed to optimize visualization of specific tissues or physiological processes. From basic anatomical imaging to advanced functional assessments, MRI has become an indispensable tool across nearly all medical specialties, including neurology, orthopedics, cardiology, oncology, and many others.
This comprehensive guide aims to explore the various types of MRI scans available in modern medical practice, examining their underlying principles, clinical applications, procedural aspects, and the unique information each technique provides. Whether you’re a patient scheduled for an MRI examination, a healthcare professional seeking to expand your knowledge, or simply someone interested in medical imaging technology, this guide will provide valuable insights into the remarkable world of MRI.
The Science Behind MRI Technology
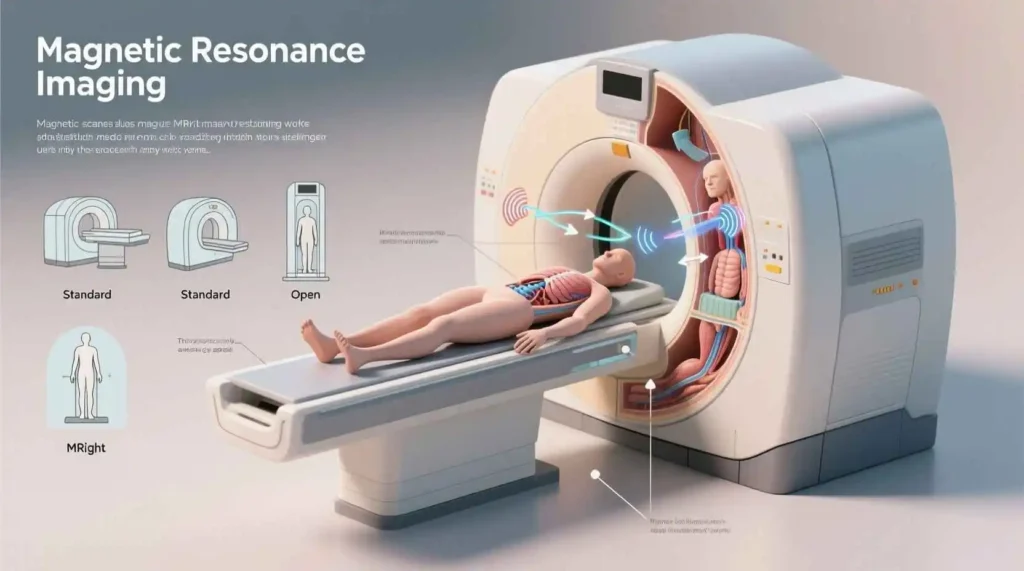
Before delving into the specific types of MRI scans, it’s essential to understand the fundamental principles that make this imaging modality possible. Unlike X-rays or computed tomography (CT) scans, which rely on ionizing radiation, MRI harnesses the properties of atomic nuclei within a magnetic field to create images.
At the core of MRI technology lies the behavior of hydrogen atoms, which are abundant in the human body, primarily in water and fat molecules. These hydrogen atoms possess a property called spin, causing them to behave like tiny magnets. When placed in a strong external magnetic field (typically 0.5 to 3.0 Tesla in clinical scanners, with research scanners going up to 7.0 Tesla or higher), these hydrogen nuclei align with the magnetic field.
The MRI scanner then emits radiofrequency pulses that temporarily knock these nuclei out of alignment. When the radiofrequency pulse is turned off, the nuclei return to their aligned state, releasing energy in the process. This emitted energy is detected by coils within the MRI scanner and processed by sophisticated computer algorithms to create detailed images.
The rate at which the nuclei return to their aligned state is characterized by two relaxation times: T1 (longitudinal relaxation) and T2 (transverse relaxation). Different tissues have different T1 and T2 relaxation times, which forms the basis for tissue contrast in MRI images. By manipulating the timing and parameters of the radiofrequency pulses and signal detection, radiologists can emphasize these differences to highlight specific tissues or pathologies.
Basic MRI Sequences
All MRI examinations are built upon a foundation of basic pulse sequences that provide fundamental anatomical information. Understanding these sequences is crucial for appreciating the more specialized MRI techniques discussed later in this guide.
T1-Weighted Imaging
T1-weighted sequences are designed to highlight differences in T1 relaxation times between tissues. In these images, fat appears bright (hyperintense), while water or fluid appears dark (hypointense). This contrast makes T1-weighted imaging particularly useful for evaluating anatomical structures, fatty tissues, and subacute hemorrhage. T1-weighted images are often considered the “anatomical” images in an MRI examination, providing excellent detail of normal anatomy and structural relationships.
T2-Weighted Imaging
T2-weighted sequences emphasize differences in T2 relaxation times between tissues. Unlike T1-weighted images, water and fluid appear bright on T2-weighted images, while fat appears less bright. This contrast makes T2-weighted imaging extremely sensitive to edema, inflammation, tumors, and other pathological processes that increase water content in tissues. T2-weighted images are often considered the “pathological” images in an MRI examination, as they readily reveal most abnormalities.
Proton Density (PD) Weighted Imaging
Proton density weighted sequences provide images that primarily reflect the concentration of hydrogen nuclei (protons) in tissues, with less influence from T1 or T2 relaxation times. These sequences offer a balance between T1 and T2 contrast and are particularly useful for evaluating structures with varying proton density, such as cartilage, ligaments, and tendons.
Fluid-Attenuated Inversion Recovery (FLAIR)
FLAIR is a specialized T2-weighted sequence that suppresses the signal from cerebrospinal fluid (CSF) while maintaining the sensitivity to pathology of a T2-weighted image. This makes FLAIR particularly valuable in neuroimaging, where it allows for better visualization of periventricular and subcortical lesions that might otherwise be obscured by the bright CSF signal on standard T2-weighted images.
Advanced MRI Techniques
While the basic sequences provide essential anatomical information, advanced MRI techniques offer insights into tissue composition, physiological processes, and functional aspects of organs. These specialized techniques have expanded the clinical utility of MRI beyond simple anatomical imaging.
Diffusion-Weighted Imaging (DWI)
Diffusion-weighted imaging measures the random motion of water molecules within tissues. In healthy tissues, water molecules move freely, but in areas of cellular injury or restricted diffusion (such as acute stroke or certain tumors), this movement is impeded. DWI is particularly sensitive in detecting acute ischemic stroke within minutes of symptom onset, making it a critical tool in emergency neuroimaging. The apparent diffusion coefficient (ADC) map, often calculated from DWI, helps differentiate true restricted diffusion from T2 “shine-through” effects.
Diffusion Tensor Imaging (DTI)
Diffusion tensor imaging is an extension of DWI that measures the directionality of water molecule movement in tissues. This technique is particularly valuable for mapping white matter tracts in the brain, as water molecules tend to move along the direction of nerve fibers. DTI can generate tractography images that visualize the connectivity between different brain regions, making it useful for planning neurosurgical procedures and studying various neurological disorders.
Magnetic Resonance Angiography (MRA)
Magnetic resonance angiography encompasses various techniques designed to visualize blood vessels without the need for catheterization or contrast agents in some cases. MRA can evaluate arteries and veins throughout the body, helping detect aneurysms, stenosis, occlusions, and vascular malformations. Common MRA techniques include time-of-flight (TOF) MRA, phase-contrast (PC) MRA, and contrast-enhanced MRA (CE-MRA), each with specific advantages for different vascular territories and clinical questions.
Magnetic Resonance Venography (MRV)
Similar to MRA, magnetic resonance venography focuses specifically on visualizing the venous system. MRV is particularly useful for evaluating venous sinus thrombosis, venous malformations, and other venous pathologies. Techniques include 2D time-of-flight, phase-contrast, and contrast-enhanced methods.
Perfusion-Weighted Imaging (PWI)
Perfusion-weighted imaging assesses blood flow at the capillary level in tissues. This technique is particularly valuable in stroke imaging, where it can identify the ischemic penumbra (tissue at risk but not yet infarcted) by comparing perfusion with diffusion findings (the perfusion-diffusion mismatch). PWI is also used in tumor imaging to assess tumor vascularity and grade, and in cardiac imaging to evaluate myocardial blood flow.
Magnetic Resonance Spectroscopy (MRS)
Magnetic resonance spectroscopy provides biochemical information about tissues by measuring the concentration of specific metabolites rather than creating anatomical images. MRS can help differentiate between tumor types, evaluate metabolic disorders, assess treatment response, and identify areas of ischemia or infection. Common metabolites evaluated in brain MRS include N-acetylaspartate (NAA), creatine, choline, lactate, and myo-inositol, each providing information about different aspects of tissue health and pathology.
Specialized MRI Applications by Body System
The versatility of MRI technology has led to the development of specialized applications for nearly every body system. These applications leverage specific sequences and techniques to address unique diagnostic challenges in different anatomical areas.
Neurological MRI
Neurological imaging represents one of the most common applications of MRI, with numerous specialized techniques developed to evaluate the brain and spinal cord.
Brain MRI
Brain MRI is the imaging modality of choice for evaluating a wide range of neurological conditions, including stroke, tumors, inflammatory diseases, neurodegenerative disorders, and traumatic injuries. A comprehensive brain MRI typically includes T1-weighted, T2-weighted, FLAIR, DWI, and often contrast-enhanced T1-weighted sequences. Specialized applications include:
- Functional MRI (fMRI): This technique detects changes in blood oxygenation related to neural activity, allowing for mapping of brain function. fMRI is valuable for presurgical planning, particularly in patients with brain tumors or epilepsy, to identify eloquent areas of the brain that should be preserved during surgery.
- Susceptibility-Weighted Imaging (SWI): SWI is highly sensitive to magnetic susceptibility differences between tissues, making it excellent for detecting blood products, calcium, and iron deposition. It is particularly useful in evaluating traumatic brain injury, vascular malformations, and neurodegenerative disorders.
- Arterial Spin Labeling (ASL): ASL is a non-contrast perfusion technique that uses magnetically labeled arterial blood water as an endogenous tracer to quantify cerebral blood flow. It is useful in evaluating cerebrovascular disease, dementia, and brain tumors.
Spinal MRI
Spinal MRI is the gold standard for evaluating spinal cord compression, disc herniation, spinal tumors, infections, and inflammatory conditions affecting the spine. High-resolution imaging of the spinal cord, nerve roots, discs, and surrounding structures is typically achieved using a combination of T1-weighted, T2-weighted, STIR (Short Tau Inversion Recovery), and contrast-enhanced sequences. Specialized techniques include:
- Myelography: MRI myelography techniques, such as CISS (Constructive Interference in Steady State) or FIESTA (Fast Imaging Employing Steady-state Acquisition), provide high-resolution images of the spinal cord and nerve roots, particularly useful for evaluating syrinx, nerve root compression, and CSF leaks.
- Diffusion Tensor Imaging (DTI) of the Spinal Cord: Similar to brain DTI, this technique maps white matter tracts in the spinal cord and can be useful in assessing spinal cord injury and compression.
Musculoskeletal MRI
Musculoskeletal MRI has revolutionized the evaluation of joints, soft tissues, and bones, providing detailed information that is often not available through other imaging modalities.
Joint MRI
MRI is the preferred imaging modality for evaluating internal derangements of joints, including ligament tears, meniscal injuries, cartilage abnormalities, and bone marrow lesions. Specific applications include:
- Knee MRI: Typically includes high-resolution T1-weighted, T2-weighted, PD-weighted, and often fat-suppressed sequences to evaluate menisci, ligaments, cartilage, and bone marrow. Specialized techniques include cartilage-specific sequences such as dGEMRIC (delayed Gadolinium-Enhanced MRI of Cartilage) and T2 mapping, which provide quantitative assessment of cartilage health.
- Shoulder MRI: Evaluates rotator cuff tears, labral injuries, and shoulder instability. MR arthrography, which involves the injection of contrast material into the joint space, provides improved visualization of intra-articular structures such as the labrum and articular cartilage.
- Hip MRI: Assesses femoroacetabular impingement, labral tears, cartilage abnormalities, and avascular necrosis. Specialized sequences include radial imaging, which provides detailed evaluation of the acetabular labrum and cartilage.
Soft Tissue MRI
MRI is excellent for evaluating soft tissue masses, muscle injuries, tendon and ligament pathology, and peripheral nerve disorders. Specific applications include:
- Muscle MRI: Can detect muscle inflammation, edema, fatty infiltration, and atrophy in various neuromuscular disorders. Specific sequences such as fat-suppressed T2-weighted imaging are particularly sensitive to muscle pathology.
- Nerve MRI: Techniques such as MR neurography provide detailed visualization of peripheral nerves, helping evaluate nerve compression, tumors, and trauma.
Cardiovascular MRI
Cardiovascular MRI (CMR) has emerged as a comprehensive tool for evaluating cardiac structure, function, perfusion, and viability without exposure to ionizing radiation.
Cardiac MRI
Cardiac MRI provides a complete assessment of cardiac anatomy and function, with applications including:
- Cine MRI: Uses electrocardiogram (ECG) gating to create dynamic images of the beating heart, allowing for accurate assessment of ventricular function, wall motion, and valve function.
- Late Gadolinium Enhancement (LGE): This technique, performed 10-20 minutes after contrast administration, detects areas of myocardial scarring or fibrosis. LGE is valuable in assessing myocardial viability after infarction, identifying fibrosis in cardiomyopathies, and detecting myocarditis.
- Stress Perfusion MRI: Evaluates myocardial blood flow during pharmacological stress (typically with adenosine or regadenoson) to detect perfusion defects indicative of coronary artery disease.
- T1 and T2 Mapping: These quantitative techniques measure the intrinsic T1 and T2 relaxation times of myocardial tissue, providing early detection of diffuse fibrosis, edema, and other tissue changes before they become apparent on conventional imaging.
Vascular MRI





