Cartilage Tears: Why They Hurt More Than You Think
As medical writers and educators, we often encounter topics that highlight the intricate workings of the human body, and cartilage tearing is one that underscores the importance of joint health. In this comprehensive article, we will explore the fundamentals of cartilage tearing, delving into its causes, symptoms, and available treatments. Cartilage, a flexible connective tissue that cushions our joints and facilitates smooth movement, is vital for everyday activities. However, when it tears, it can lead to significant pain and mobility issues, affecting millions worldwide. Drawing from reliable medical sources, we aim to provide an informational overview that empowers readers to understand this condition better and seek appropriate care. By the end, we hope to equip you with knowledge that could aid in prevention and recovery. Our discussion will span approximately 1,000 words, covering key aspects in detail, including tables, lists, and a relevant quotation.
What Is Cartilage and Why Does It Matter?
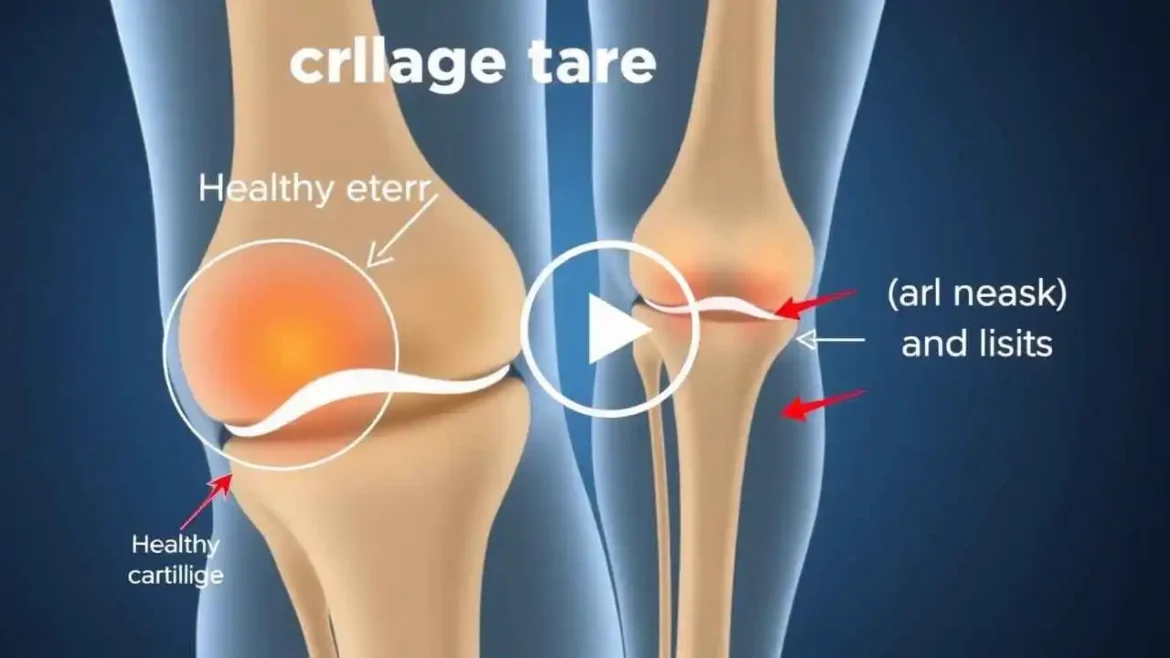
We begin by establishing a foundational understanding of cartilage, as it sets the stage for discussing tearing. Cartilage is a tough, rubbery tissue found in various parts of the body, including the joints, nose, ears, and between vertebrae. It serves as a shock absorber, reducing friction and allowing bones to glide over one another smoothly. There are three main types: hyaline cartilage (found in joints like the knees and elbows), elastic cartilage (in the ears and larynx), and fibrocartilage (in the intervertebral discs and knees). When we talk about cartilage tearing, we’re often referring to injuries in weight-bearing joints, such as the knee or shoulder.
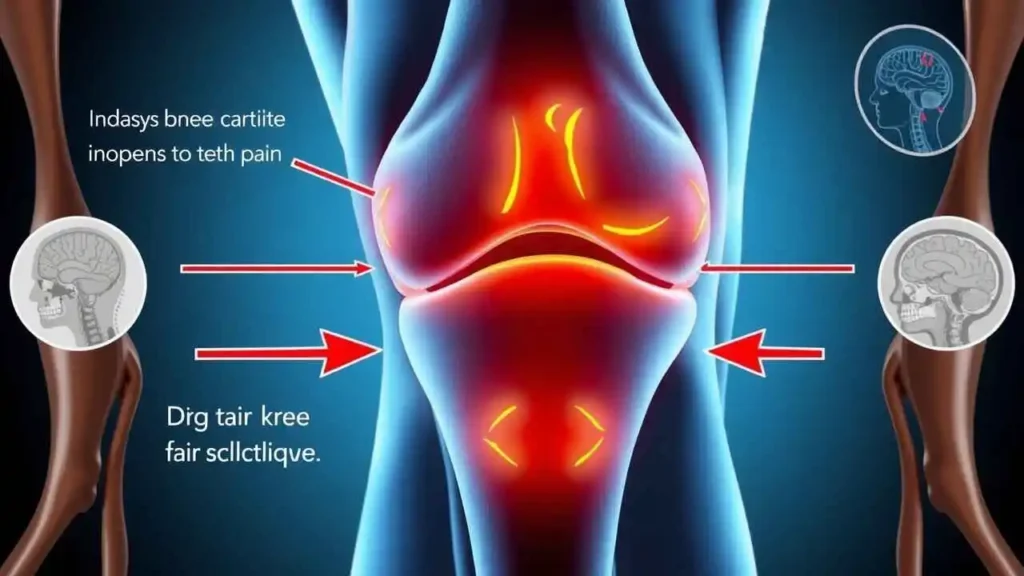
Tearing occurs when this tissue is damaged, either partially or completely, leading to what is medically known as a chondral or meniscal injury. These tears can range from minor fissures to full-thickness defects, and they are particularly common in high-impact sports or due to degenerative conditions. As we age, our cartilage naturally loses elasticity, making it more susceptible to injury. According to the American Academy of Orthopaedic Surgeons, cartilage injuries affect over 10 million people annually in the United States alone, often resulting from trauma or wear and tear. We will now examine the primary causes, which can help us identify risk factors and preventive measures.
Causes of Cartilage Tearing
In our experience, understanding the causes of cartilage tearing is crucial for prevention and early intervention. These injuries don’t happen in isolation; they stem from a combination of acute events and chronic factors. We can categorize the main causes as follows, using an unordered list for clarity:
- Traumatic Injuries: Sudden impacts or twists are among the most common culprits. For instance, during sports like soccer or basketball, a forceful blow to the knee can cause a meniscal tear. We often see this in athletes who pivot quickly or land awkwardly, leading to immediate cartilage damage.
- Overuse and Repetitive Strain: Repetitive motions, such as running on hard surfaces or lifting heavy weights without proper form, can gradually wear down cartilage. This is prevalent in professions like construction or among long-distance runners, where the constant stress exceeds the tissue’s ability to repair itself.
- Age-Related Degeneration: As we advance in age, cartilage naturally thins and becomes less resilient due to reduced blood supply and cellular activity. Conditions like osteoarthritis accelerate this process, making older adults more vulnerable to tears even from minor activities.
- Genetic and Congenital Factors: Some individuals are predisposed to weaker cartilage due to genetic conditions, such as Ehlers-Danlos syndrome, which affects connective tissue integrity. We also note that congenital joint abnormalities can increase the risk.
- Other Contributing Factors: Obesity places extra stress on joints, while poor nutrition—lacking essential nutrients like glucosamine—can impair cartilage health. Additionally, previous injuries that weren’t properly rehabilitated often lead to secondary tears.
These causes highlight how lifestyle, genetics, and environment interplay to create vulnerability. In a table below, we summarize the key causes alongside their typical risk groups and preventive strategies, drawing from clinical data to make this information more digestible.
| Cause | Typical Risk Groups | Preventive Strategies |
| Traumatic Injuries | Athletes, young adults | Use protective gear, warm up properly, and avoid high-risk activities without training |
| Overuse and Strain | Runners, manual laborers | Incorporate rest days, cross-train, and maintain proper ergonomics |
| Age-Related Degeneration | Older adults (over 50) | Engage in low-impact exercises, maintain a healthy weight, and follow a nutrient-rich diet |
| Genetic Factors | Individuals with family history | Regular medical check-ups and genetic counseling |
| Other Factors (e.g., Obesity) | Overweight individuals | Adopt a balanced diet, exercise regularly, and monitor joint health |
This table, based on insights from orthopedic studies, illustrates how targeted prevention can mitigate risks. We encourage readers to consult healthcare professionals for personalized advice.
Recognizing the Symptoms