Ophthalmology Essentials: Everything You Need to Know About Eye Health
Introduction
Ophthalmology stands as one of the most intricate and vital specialties in medicine, dedicated to the diagnosis, treatment, and prevention of disorders of the visual system. This remarkable field encompasses the eyes and their surrounding structures, addressing conditions that range from minor irritations to vision-threatening diseases. The significance of ophthalmology extends far beyond medical treatment, touching upon fundamental aspects of human experience, as vision plays an integral role in how we perceive, interact with, and navigate the world around us.
The human eye itself is an extraordinary organ, often described as a window to the body. Its complexity rivals that of any other organ system, with intricate structures working in concert to capture, focus, and convert light into electrochemical impulses that the brain interprets as images. This sophisticated process involves numerous components, each with specialized functions, and requires precise coordination between the eyes and the brain to produce clear vision.
Historically, ophthalmology has evolved from ancient practices of eye care to a highly sophisticated medical and surgical specialty. Ancient civilizations, including the Egyptians, Greeks, and Indians, documented various eye conditions and treatments, though many were based on limited understanding. The development of the ophthalmoscope in the mid-19th century revolutionized the field, allowing physicians to directly visualize the interior of the eye for the first time. Since then, ophthalmology has advanced at an extraordinary pace, incorporating cutting-edge technologies, innovative surgical techniques, and groundbreaking research.
Today’s ophthalmologists are medical doctors who complete extensive education and training, typically including four years of medical school followed by a residency in ophthalmology, and often additional fellowship training in subspecialty areas. This rigorous preparation equips them to address a wide spectrum of eye conditions using medical, laser, and surgical interventions.
The scope of ophthalmology is remarkably broad, encompassing numerous subspecialties that focus on specific aspects of eye care. These include cornea and external disease, glaucoma, vitreoretinal surgery, neuro-ophthalmology, pediatric ophthalmology, ophthalmic plastic surgery, and uveitis, among others. Each subspecialty addresses unique conditions requiring specialized knowledge and skills, reflecting the diversity and complexity of the visual system.
The importance of ophthalmology in healthcare cannot be overstated. Vision impairment and blindness affect millions of people worldwide, with significant personal, social, and economic consequences. According to the World Health Organization, an estimated 2.2 billion people globally have vision impairment, and of these, at least 1 billion have vision impairment that could have been prevented or has yet to be addressed. Ophthalmology plays a crucial role in reducing this burden through prevention, early detection, and effective treatment of eye diseases.
Moreover, the eyes can provide valuable insights into overall health. Many systemic conditions, including diabetes, hypertension, autoimmune diseases, and neurological disorders, can manifest with ocular signs and symptoms. Ophthalmologists often play a key role in identifying these systemic diseases, making eye examinations an important component of comprehensive healthcare.
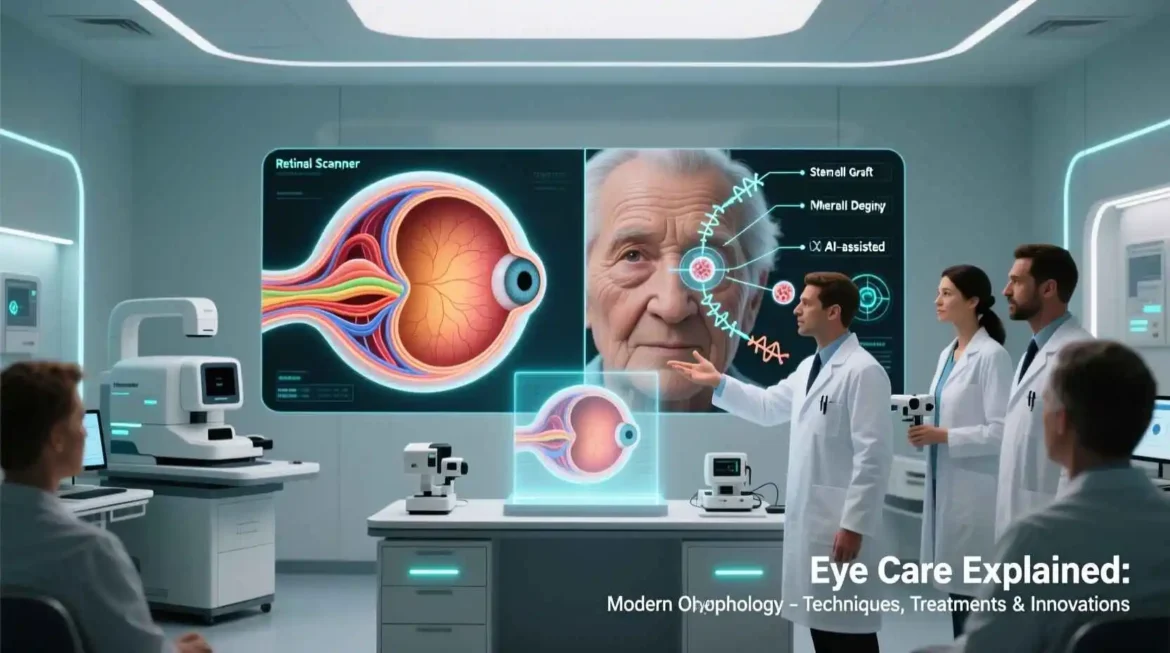
Technological advancements have transformed ophthalmology in recent decades, enhancing diagnostic capabilities, expanding treatment options, and improving surgical outcomes. From advanced imaging techniques that allow visualization of the eye at a microscopic level to laser technologies that enable precise interventions with minimal recovery time, these innovations have revolutionized eye care. The development of new medications, surgical techniques, and devices continues to push the boundaries of what is possible in preserving and restoring vision.
Public health initiatives in ophthalmology have also made significant contributions to vision health worldwide. Screening programs for conditions like diabetic retinopathy, glaucoma, and refractive errors have helped identify eye diseases at earlier, more treatable stages. Vision correction services, including eyeglasses and contact lenses, remain one of the most cost-effective health interventions, improving quality of life and productivity for millions of people.
As we look to the future, ophthalmology continues to evolve at a rapid pace. Emerging technologies such as artificial intelligence for diagnosis and screening, gene therapies for inherited retinal diseases, and regenerative medicine approaches hold promise for further advancing eye care. These developments, combined with ongoing research into the causes and mechanisms of eye diseases, are expanding our understanding of the visual system and opening new frontiers in treatment.
This comprehensive exploration of ophthalmology will delve into the anatomy and physiology of the eye, common eye conditions, diagnostic techniques, treatment approaches, subspecialty areas, and emerging trends in the field. By examining these topics in detail, we aim to provide a thorough understanding of this fascinating medical specialty and its critical role in preserving one of our most precious senses – vision.
Anatomy and Physiology of the Eye
The human eye represents one of nature’s most sophisticated sensory organs, a complex structure designed to capture light and convert it into electrochemical impulses that the brain interprets as visual images. Understanding the intricate anatomy and physiology of the eye is fundamental to comprehending how vision works and how various conditions can affect visual function. The eye consists of three main layers: the fibrous layer, the vascular layer, and the neural layer, each with distinct components and functions.
The fibrous layer forms the outermost coat of the eye and includes the sclera and cornea. The sclera, commonly known as the white of the eye, is a tough, protective covering that maintains the shape of the eye and provides attachment for the extraocular muscles that control eye movement. Composed primarily of collagen fibers, the sclera is relatively avascular but contains numerous nerve endings, making it sensitive to pain when inflamed or irritated.
The cornea, the transparent anterior portion of the fibrous layer, plays a crucial role in vision. As the eye’s primary refractive surface, the cornea is responsible for approximately two-thirds of the eye’s focusing power. Its transparency is essential for clear vision, achieved through several unique features: the absence of blood vessels, the precise arrangement of collagen fibers, and the maintenance of relative dehydration through an active endothelial pump. The cornea is one of the most densely innervated tissues in the body, explaining why even minor corneal abrasions can cause significant pain.
Beneath the fibrous layer lies the vascular layer, or uvea, which consists of the choroid, ciliary body, and iris. The choroid is a highly vascular layer that supplies oxygen and nutrients to the outer layers of the retina. It contains melanocytes that produce melanin, which helps absorb excess light and prevent internal reflection within the eye.
The ciliary body, a ring-shaped structure that extends from the choroid, performs several important functions. It contains the ciliary muscle, which controls the shape of the lens for focusing at different distances (accommodation). The ciliary body also produces aqueous humor, the clear fluid that fills the anterior and posterior chambers of the eye, and contains the ciliary processes, which are part of the blood-aqueous barrier.
The iris, the visible colored portion of the eye, lies between the cornea and the lens. It consists of two layers of smooth muscle fibers that control the size of the pupil, the central opening through which light enters the eye. The sphincter pupillae muscle constricts the pupil in bright light (miosis), while the dilator pupillae muscle enlarges the pupil in dim light (mydriasis). The iris contains pigments that determine eye color, ranging from blue to green to brown, depending on the amount and distribution of melanin.
The innermost layer of the eye is the neural layer, or retina, which contains photoreceptor cells that convert light into electrical signals. The retina is a complex, layered structure approximately 0.5 mm thick, composed of neurons and supporting cells. It can be divided into several regions: the macula, fovea, optic disc, and peripheral retina.
The macula is a small, highly specialized area in the center of the retina responsible for central vision and color perception. Within the macula lies the fovea, a depression containing the highest concentration of cone photoreceptors, which provide the sharpest vision. The fovea is critical for activities requiring detailed vision, such as reading and facial recognition.
The optic disc, also known as the blind spot, is the point where the optic nerve exits the eye. This area lacks photoreceptors and is therefore insensitive to light. The peripheral retina, which surrounds the macula, contains primarily rod photoreceptors that are more sensitive to low light levels and are important for peripheral vision and night vision.
Photoreceptor cells in the retina are of two types: rods and cones. Rods, which number approximately 120 million per eye, are highly sensitive to light and function well in dim lighting conditions. They contain the photopigment rhodopsin and are responsible for peripheral vision and motion detection. Cones, numbering about 6 million per eye, function best in bright light and are responsible for color vision and high visual acuity. Three types of cones contain different photopigments that respond to blue, green, or red wavelengths of light, enabling color discrimination.
Other important structures in the eye include the lens, aqueous humor, and vitreous body. The lens is a transparent, biconvex structure located behind the iris and pupil. It changes shape to focus light onto the retina, a process called accommodation. With age, the lens gradually loses elasticity, leading to presbyopia, a condition that affects near vision.
The aqueous humor is a clear fluid produced by the ciliary body that fills the anterior and posterior chambers of the eye. It maintains intraocular pressure, provides nutrients to the avascular structures of the eye, and removes waste products. The balance between aqueous production and drainage is crucial for maintaining normal eye pressure; disruption of this balance can lead to glaucoma.
The vitreous body, or vitreous humor, is a clear, gel-like substance that fills the space between the lens and the retina. It helps maintain the shape of the eye and provides a pathway for light reaching the retina. With age, the vitreous may liquefy and form floaters, which appear as small moving spots in the visual field.
The eye’s focusing system involves several structures working together to direct light onto the retina. Light first passes through the cornea, which provides most of the refractive power. The light then passes through the pupil, whose size is regulated by the iris. The lens fine-tunes the focus by changing shape, a process controlled by the ciliary muscles. Finally, the light reaches the retina, where it is converted into electrical signals.
The process of vision begins when light enters the eye and stimulates the photoreceptor cells in the retina. When light hits the photopigments in rods and cones, it triggers a chemical reaction that generates electrical signals. These signals are processed by other retinal neurons, including bipolar cells and ganglion cells, which modify and integrate the visual information before transmitting it to the brain.
The optic nerve, composed of axons from ganglion cells, carries visual information from the retina to the brain. At the optic chiasm, fibers from the nasal half of each retina cross to the opposite side, while fibers from the temporal half remain on the same side. This arrangement ensures that the right visual field is processed by the left cerebral hemisphere and vice versa.
Visual information is ultimately processed in the visual cortex of the occipital lobe of the brain. The primary visual cortex receives raw visual data and performs basic processing, while higher visual areas interpret more complex aspects of vision, including form, color, motion, and depth perception. The brain integrates visual information with input from other senses and past experiences to create our perception of the visual world.
The eye also contains several accessory structures that support its function and protection. These include the eyelids, eyelashes, conjunctiva, and lacrimal apparatus. The eyelids protect the eye from foreign objects, distribute tears across the ocular surface, and regulate the amount of light entering the eye. The eyelashes help trap debris and prevent it from entering the eye.
The conjunctiva is a thin, transparent membrane that lines the inner surface of the eyelids and covers the anterior portion of the sclera. It contains numerous goblet cells that produce mucus, which helps lubricate the eye’s surface. The lacrimal apparatus, which includes the lacrimal gland and drainage system, produces and distributes tears that keep the eye moist and protected.
Tear film, which covers the ocular surface, consists of three layers: an outer lipid layer produced by the meibomian glands in the eyelids that prevents evaporation; a middle aqueous layer produced by the lacrimal glands that provides moisture and nutrients; and an inner mucin layer produced by conjunctival goblet cells that helps the tear film adhere to the eye. A stable tear film is essential for clear vision and ocular comfort.
The eye’s blood supply comes primarily from the ophthalmic artery, a branch of the internal carotid artery. The central retinal artery supplies the inner layers of the retina, while the ciliary arteries supply the outer layers, choroid, ciliary body, and iris. Venous drainage occurs through the central retinal vein and vortex veins, which ultimately empty into the cavernous sinus.
The eye is innervated by several cranial nerves, including the optic nerve (cranial nerve II), which carries visual information to the brain; the oculomotor nerve (cranial nerve III), which controls most of the extraocular muscles and the sphincter pupillae muscle; the trochlear nerve (cranial nerve IV), which controls the superior oblique muscle; the trigeminal nerve (cranial nerve V), which provides sensory innervation to the eye and surrounding structures; the abducens nerve (cranial nerve VI), which controls the lateral rectus muscle; and the facial nerve (cranial nerve VII), which controls the muscles of facial expression and the lacrimal gland.
Understanding the complex anatomy and physiology of the eye is essential for comprehending how vision works and how various conditions can affect visual function. This knowledge forms the foundation for the diagnosis and treatment of eye disorders, enabling ophthalmologists to identify abnormalities and develop appropriate interventions to preserve and restore vision.
Common Eye Conditions and Disorders
The field of ophthalmology encompasses a wide array of conditions affecting the eyes and visual system, ranging from minor irritations to vision-threatening diseases. These conditions can affect various structures of the eye and may result from genetic factors, aging, environmental influences, systemic diseases, or infections. Understanding common eye conditions is essential for recognizing symptoms, seeking appropriate care, and implementing preventive measures.
Refractive errors represent the most common vision problems worldwide, affecting individuals of all ages. These conditions occur when the shape of the eye prevents light from focusing directly on the retina, resulting in blurred vision. The primary types of refractive errors include myopia (nearsightedness), hyperopia (farsightedness), astigmatism, and presbyopia.
Myopia, or nearsightedness, affects approximately 30% of the global population and occurs when the eyeball is too long relative to the focusing power of the cornea and lens. This causes light rays to focus in front of the retina rather than directly on it, resulting in clear vision for nearby objects but blurred vision for distant objects. Myopia often develops in childhood and may progress during the teenage years before stabilizing in early adulthood. Factors contributing to myopia include genetics and environmental influences such as prolonged near work and limited time spent outdoors.
Hyperopia, or farsightedness, occurs when the eyeball is too short or the cornea has too little curvature, causing light to focus behind the retina. People with hyperopia can typically see distant objects more clearly than nearby ones, though this depends on the degree of hyperopia and the age of the individual. Mild hyperopia in young children may be compensated for by accommodation (the eye’s ability to focus), but as the eye ages, this compensation becomes less effective, leading to symptoms such as eye strain, headaches, and blurred near vision.
Astigmatism results from an irregular curvature of the cornea or lens, causing light to focus at multiple points rather than a single point on the retina. This irregular focusing leads to blurred or distorted vision at all distances. Astigmatism often occurs in conjunction with myopia or hyperopia and can be corrected with eyeglasses, contact lenses, or refractive surgery.
Presbyopia is an age-related condition that affects the ability to focus on near objects, typically becoming noticeable in the early to mid-40s. It occurs as the lens gradually loses elasticity and the ciliary muscles weaken, reducing the eye’s ability to accommodate for near vision. Presbyopia affects nearly everyone as they age and is typically managed with reading glasses, bifocal or progressive lenses, or multifocal contact lenses.
Cataracts, another extremely common eye condition, involve clouding of the eye’s natural lens, leading to decreased vision. Cataracts can develop in one or both eyes and often progress slowly over time. The primary cause of cataracts is aging, with more than half of Americans aged 80 or older having cataracts or having undergone cataract surgery. Other risk factors include diabetes, smoking, excessive alcohol consumption, prolonged exposure to sunlight, and certain medications such as corticosteroids.
Symptoms of cataracts include blurred or dim vision, increased sensitivity to glare, difficulty with night vision, seeing halos around lights, frequent changes in eyeglass prescription, and fading or yellowing of colors. When cataracts significantly interfere with daily activities, surgical removal of the cloudy lens and replacement with an artificial intraocular lens is the standard treatment. Cataract surgery is one of the most commonly performed surgical procedures worldwide, with high success rates and relatively low risk.
Glaucoma encompasses a group of eye conditions characterized by damage to the optic nerve, often associated with elevated intraocular pressure. This damage leads to progressive, irreversible vision loss that typically begins with peripheral vision and may advance to central vision if left untreated. Glaucoma is a leading cause of irreversible blindness worldwide, affecting an estimated 80 million people globally.
The two main types of glaucoma are open-angle glaucoma and angle-closure glaucoma. Open-angle glaucoma, the more common form, develops slowly and painlessly as the eye’s drainage canals become clogged over time, leading to increased eye pressure. Angle-closure glaucoma occurs when the iris bulges forward to narrow or block the drainage angle formed by the cornea and iris, causing a sudden increase in eye pressure that requires immediate medical attention.
Risk factors for glaucoma include age (being over 60), family history, African or Asian ancestry, certain medical conditions (such as diabetes, heart disease, and high blood pressure), prolonged corticosteroid use, and previous eye injuries. While there is no cure for glaucoma, early detection and treatment can significantly slow or prevent vision loss. Treatment options include prescription eye drops, oral medications, laser treatment, and surgery.
Age-related macular degeneration (AMD) is a leading cause of vision loss among people aged 50 and older. This condition affects the macula, the part of the retina responsible for central vision. AMD can make it difficult to perform daily activities such as reading, recognizing faces, driving, and performing close-up work.
There are two types of AMD: dry (atrophic) and wet (neovascular or exudative). Dry AMD, which accounts for approximately 80-90% of cases, occurs when the macula thins over time as part of the aging process, gradually blurring central vision. Wet AMD, though less common, is more severe and occurs when abnormal blood vessels grow beneath the retina and leak fluid or blood, causing rapid damage to the macula.
Risk factors for AMD include age, family history, smoking, obesity, high blood pressure, and light-colored eyes. While there is no cure for AMD, treatments such as anti-VEGF injections, photodynamic therapy, and laser therapy can help slow its progression and preserve vision. Nutritional supplements containing specific vitamins and minerals (the AREDS2 formula) may also reduce the risk of progression in people with intermediate or advanced dry AMD.
Diabetic retinopathy is a complication of diabetes that affects the blood vessels in the retina. It is a leading cause of blindness in working-age adults and affects approximately one-third of people with diabetes. The condition develops when high blood sugar levels damage the tiny blood vessels that nourish the retina, causing them to leak fluid or blood or to close off completely.
Diabetic retinopathy progresses through stages, from mild nonproliferative diabetic retinopathy (NPDR), with few small areas of balloon-like swelling in retinal vessels, to moderate and severe NPDR, with more blocked blood vessels and potential retinal swelling (macular edema). In advanced stages, proliferative diabetic retinopathy (PDR) occurs, characterized by the growth of new, abnormal blood vessels on the retina’s surface that can bleed easily and lead to scar tissue formation.
Risk factors for diabetic retinopathy include duration of diabetes, poor blood sugar control, high blood pressure, high cholesterol, pregnancy, and tobacco use. Management of diabetic retinopathy focuses on controlling diabetes and other risk factors, along with treatments such as laser photocoagulation, intravitreal injections of anti-VEGF medications or steroids, and vitrectomy surgery in advanced cases.
Dry eye syndrome is a common condition that occurs when the eyes do not produce enough tears or when tears evaporate too quickly. This results in inflammation and discomfort of the eye’s surface. Symptoms include stinging, burning, scratchiness, excessive tearing, sensitivity to light, redness, and blurred vision that may improve with blinking.
Dry eye can be caused by various factors, including aging, hormonal changes (particularly in women during menopause), autoimmune diseases such as Sjögren’s syndrome, certain medications (antihistamines, decongestants, antidepressants, hormone replacement therapy), environmental conditions (wind, dry air, air conditioning), and prolonged screen use. Treatment options include artificial tears, prescription eye drops (such as cyclosporine or lifitegrast), punctal plugs to reduce tear drainage, omega-3 fatty acid supplements, and lifestyle modifications.
Conjunctivitis, commonly known as pink eye, is an inflammation or infection of the conjunctiva, the thin, transparent membrane that lines the inner surface of the eyelid and covers the white part of the eye. Conjunctivitis can be caused by viruses, bacteria, allergens, or irritants. Viral conjunctivitis, often associated with the common cold, typically causes watery discharge and a feeling of grittiness in the eye. Bacterial conjunctivitis produces a thicker, yellow-green discharge and may affect one or both eyes. Allergic conjunctivitis is characterized by itching, redness, and excessive tearing, often accompanied by other allergy symptoms.
Treatment of conjunctivitis depends on the cause. Viral conjunctivitis usually resolves on its own within 1-3 weeks, though supportive care with cold compresses and artificial tears may provide relief. Bacterial conjunctivitis is typically treated with antibiotic eye drops or ointments. Allergic conjunctivitis can be managed with antihistamine eye drops, oral antihistamines, and avoidance of allergens.
Retinal detachment is a serious eye condition that occurs when the retina separates from the underlying supportive tissue. Without prompt treatment, retinal detachment can lead to permanent vision loss. Symptoms include the sudden appearance of floaters (dark, moving specks in the field of vision), flashes of light in one or both eyes, reduced peripheral vision, and the sensation of a curtain or shadow moving across the visual field.
Risk factors for retinal detachment include aging, previous retinal detachment in the other eye, family history, extreme nearsightedness, previous eye surgery or eye injury, and certain eye diseases. Treatment typically involves surgery to reattach the retina, using techniques such as pneumatic retinopexy, scleral buckling, or vitrectomy. The success rate of retinal detachment surgery is high, particularly when performed promptly, but some vision loss may occur even with successful reattachment.
Keratoconus is a progressive eye condition in which the cornea thins and gradually bulges outward into a cone shape. This irregular shape causes light to focus unevenly on the retina, resulting in distorted vision. Keratoconus typically begins in adolescence or early adulthood and may progress for 10-20 years before stabilizing. Symptoms include blurred vision, increased sensitivity to light, glare, and frequent changes in eyeglass prescription.
In early stages, keratoconus can be managed with eyeglasses or soft contact lenses. As the condition progresses, specially designed rigid gas permeable contact lenses, hybrid lenses, or scleral lenses may be necessary. In advanced cases, treatments such as corneal cross-linking (a procedure that strengthens corneal tissue to prevent further bulging), intracorneal ring segments, or corneal transplantation may be required.
Strabismus, commonly known as crossed eyes, is a condition in which the eyes do not properly align with each other. One eye may turn in, out, up, or down while the other eye focuses in one direction. Strabismus can be constant or intermittent and may affect one or both eyes. This condition is particularly common in children, affecting approximately 4% of children in the United States.
Strabismus can lead to amblyopia (lazy eye), a condition in which the brain begins to ignore signals from the misaligned eye, resulting in reduced vision. Treatment of strabismus depends on the underlying cause and may include eyeglasses, prism lenses, vision therapy, eye muscle exercises, or surgery to correct the alignment of the eyes. Early detection and treatment are crucial for preventing permanent vision loss.
Amblyopia, or lazy eye, is a vision development disorder in which an eye fails to achieve normal visual acuity, even with prescription eyeglasses or contact lenses. Amblyopia affects approximately 2-3% of the population and is the most common cause of vision impairment in children. The condition typically occurs when one eye has significantly better focus than the other, due to strabismus, significant refractive error difference between the eyes, or clouding of the ocular media (such as from a cataract).
Treatment of amblyopia is most effective when initiated early in childhood, ideally before age 7. Approaches include correcting the underlying cause (such as prescribing eyeglasses or removing a cataract), patching the stronger eye to force the weaker eye to work harder, using atropine drops to temporarily blur vision in the stronger eye, and vision therapy. With appropriate treatment, vision can often be significantly improved, though some cases may have permanent vision deficits.
Blepharitis is a common eye condition characterized by inflammation of the eyelids, usually affecting both eyes. Symptoms include redness, swelling, itching, burning, a feeling of grittiness in the eyes, crusting of the eyelids (especially upon waking), and flaking of skin around the eyes. Blepharitis can be uncomfortable and unsightly but rarely causes permanent vision damage.
The condition is often associated with bacterial infection, dysfunction of the oil glands in the eyelids (meibomian gland dysfunction), or skin conditions such as seborrheic dermatitis or rosacea. Treatment focuses on good eyelid hygiene, including warm compresses, eyelid massage, and gentle cleansing of the eyelid margins. In more severe cases, antibiotic eye drops or ointments, steroid eye drops, or oral antibiotics may be prescribed.
Uveitis refers to inflammation of the uvea, the middle layer of the eye that includes the iris, ciliary body, and choroid. This condition can affect one or both eyes and may be acute (lasting a short time) or chronic (recurring or lasting a long time). Symptoms include eye redness, pain, light sensitivity, blurred vision, and floaters.
Uveitis can be caused by infections, autoimmune disorders, or eye injuries, though in many cases, the cause remains unknown. Treatment depends on the underlying cause and severity of inflammation but may include corticosteroid eye drops, oral corticosteroids, immunosuppressive medications, or biologic agents. Without proper treatment, uveitis can lead to complications such as cataracts, glaucoma, macular edema, and permanent vision loss.
Eye allergies, also known as allergic conjunctivitis, occur when the eyes react to substances called allergens. Common allergens include pollen, dust mites, mold spores, pet dander, and certain cosmetics or perfumes. When allergens come into contact with the eyes, they trigger the release of histamine and other chemicals that cause symptoms such as itching, redness, tearing, burning, and swelling of the eyelids.
Eye allergies are often associated with other allergic conditions such as hay fever, asthma, or eczema. Management strategies include avoiding known allergens, using cold compresses to reduce swelling, applying lubricating eye drops to wash away allergens, and using over-the-counter or prescription antihistamine eye drops. In severe cases, oral antihistamines or mast cell stabilizer eye drops may be recommended.
Color vision deficiency, commonly known as color blindness, is the inability or decreased ability to see color or perceive color differences under normal lighting conditions. The condition affects approximately 8% of men and 0.5% of women of Northern European descent, though prevalence varies among different populations. Most cases of color vision deficiency are inherited and present from birth, though the condition can also result from eye diseases, medications, or aging.
The most common type of color vision deficiency is red-green color blindness, which affects the ability to distinguish between red and green hues. Blue-yellow color blindness is less common, and complete color blindness (achromatopsia) is rare. While there is no cure for inherited color vision deficiency, most people adapt to the condition with little impact on daily activities. Special tinted lenses or glasses may help some individuals better distinguish colors, and various assistive technologies can aid with color identification tasks.
Understanding these common eye conditions and disorders is essential for recognizing symptoms, seeking appropriate care, and implementing preventive measures. Regular eye examinations play a crucial role in early detection and treatment of eye diseases, helping to preserve vision and maintain quality of life. As research continues to advance our knowledge of eye diseases and their mechanisms, new diagnostic tools and treatment approaches continue to emerge, offering hope for improved outcomes for individuals affected by these conditions.
Diagnostic Techniques in Ophthalmology
The field of ophthalmology relies on a diverse array of diagnostic techniques to evaluate eye health, detect abnormalities, and guide treatment decisions. These techniques range from basic examinations that have been used for centuries to sophisticated imaging technologies that provide unprecedented views of ocular structures. The comprehensive assessment of visual function and ocular health forms the foundation of ophthalmic diagnosis, enabling ophthalmologists to identify conditions at their earliest stages and monitor changes over time.
The diagnostic process typically begins with a thorough patient history, during which the ophthalmologist gathers information about the patient’s symptoms, medical history, family history, medications, and lifestyle factors. This information provides valuable context for interpreting examination findings and helps guide the selection of appropriate diagnostic tests. Common symptoms that prompt ophthalmic evaluation include blurred vision, eye pain, redness, double vision, floaters, flashes of light, and visual field loss.
Visual acuity testing is one of the most fundamental and widely recognized diagnostic techniques in ophthalmology. This test measures the eye’s ability to distinguish details and shapes at a given distance, typically using a Snellen chart or similar visual acuity chart. The patient reads letters or symbols of decreasing size from a standardized distance (usually 20 feet or 6 meters), and the results are expressed as a fraction (e.g., 20/20 vision, which indicates that the patient can see at 20 feet what a person with normal vision can see at 20 feet). Visual acuity testing helps assess the clarity of vision and can detect refractive errors, amblyopia, and various eye diseases.
Refraction is the process of determining the appropriate lens prescription to correct refractive errors. During refraction, the patient looks through a phoropter, an instrument containing various lenses, and indicates which lenses provide the clearest vision. The ophthalmologist may use automated refractors or retinoscopy, a technique that involves shining a light into the eye and observing the reflection from the retina, to obtain an objective measurement of the eye’s refractive error. The results of refraction are used to prescribe eyeglasses or contact lenses.
Slit lamp biomicroscopy is a critical diagnostic technique that allows detailed examination of the anterior segment of the eye, including the eyelids, conjunctiva, cornea, iris, and lens. The slit lamp microscope uses a bright light source that can be adjusted to a narrow slit, combined with a microscope, to provide a magnified, three-dimensional view of ocular structures. Special lenses can be used with the slit lamp to examine deeper structures, including the vitreous and retina. Slit lamp examination is essential for detecting conditions such as cataracts, corneal abnormalities, uveitis, and foreign bodies.
Tonometry is the measurement of intraocular pressure (IOP), which is crucial for diagnosing and monitoring glaucoma. Several methods of tonometry exist, including Goldmann applanation tonometry (considered the gold standard), non-contact tonometry (the “air puff” test), and portable tonometers. During applanation tonometry, the eye is anesthetized with drops, and a small probe gently flattens a portion of the cornea to measure the pressure required. Elevated IOP is a major risk factor for glaucoma, though not all individuals with high IOP develop glaucoma, and some individuals with normal IOP can develop the condition (normal-tension glaucoma).
Ophthalmoscopy is a technique that allows direct visualization of the interior of the eye, including the retina, optic nerve, and blood vessels. Direct ophthalmoscopy provides a magnified but relatively narrow view of the fundus, while indirect ophthalmoscopy, often combined with a condensing lens, provides a wider, stereoscopic view that is particularly useful for examining the peripheral retina. Ophthalmoscopy is essential for detecting conditions such as diabetic retinopathy, macular degeneration, retinal detachment, and optic nerve abnormalities.
Visual field testing, also known as perimetry, measures the entire area that can be seen when the eye is fixed straight ahead. This test is crucial for detecting and monitoring glaucoma, as well as various neurological conditions that affect vision. The most common type of visual field testing is automated static perimetry, in which the patient focuses on a central point and presses a button whenever they see a small light appear in their peripheral vision. The test creates a map of the patient’s visual field, showing areas of reduced sensitivity that may indicate damage to the retina, optic nerve, or visual pathways in the brain.
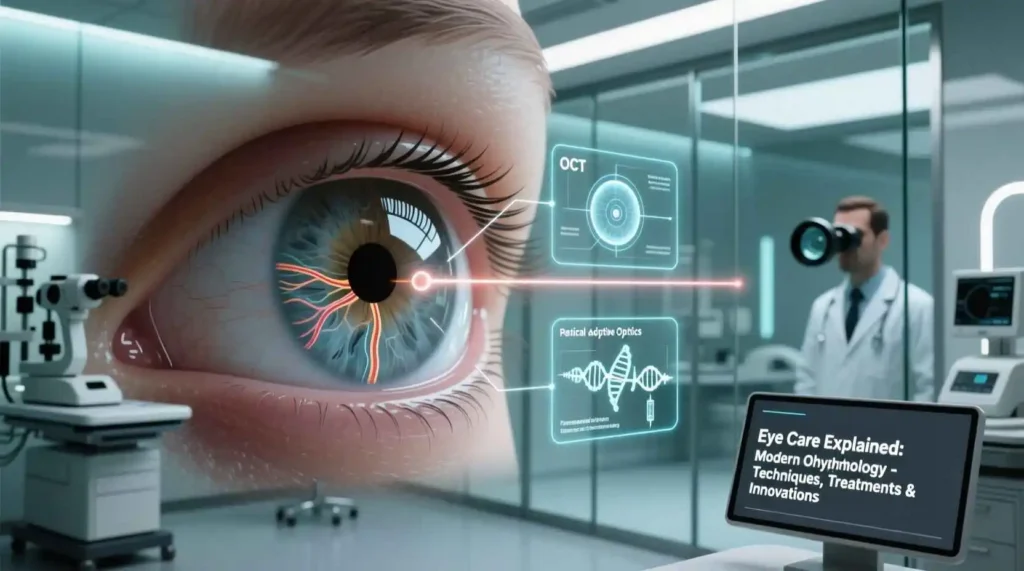
Optical coherence tomography (OCT) has revolutionized ophthalmic imaging since its introduction in the 1990s. This non-invasive imaging technique uses light waves to create cross-sectional images of the retina and optic nerve with micrometer resolution. OCT functions similarly to ultrasound but uses light instead of sound, providing detailed images of retinal layers and enabling precise measurement of retinal thickness. OCT is invaluable for diagnosing and monitoring conditions such as macular degeneration, diabetic retinopathy, glaucoma, and macular holes. The technology continues to advance, with newer devices offering enhanced imaging speed, resolution, and capabilities such as OCT angiography, which visualizes retinal blood vessels without the need for dye injection.
Fluorescein angiography is a diagnostic technique that involves injecting a fluorescent dye (fluorescein) into a vein in the arm and taking rapid-sequence photographs as the dye circulates through the retinal blood vessels. This test helps evaluate blood flow in the retina and choroid and can detect abnormalities such as leaking blood vessels, areas of poor perfusion, and neovascularization (abnormal new blood vessel growth). Fluorescein angiography is particularly useful for managing diabetic retinopathy, macular degeneration, retinal vein occlusions, and inflammatory eye conditions.
Indocyanine green (ICG) angiography is similar to fluorescein angiography but uses a different dye that better penetrates the retinal pigment epithelium. ICG angiography provides enhanced visualization of the choroidal circulation and is particularly useful for evaluating conditions that affect the choroid, such as certain types of macular degeneration, inflammatory conditions, and choroidal tumors.
Ultrasound imaging plays an important role in ophthalmic diagnosis, particularly when media opacities (such as dense cataracts or vitreous hemorrhage) prevent direct visualization of the eye’s interior. B-scan ultrasonography provides a two-dimensional cross-sectional image of the eye and is used to detect conditions such as retinal detachment, intraocular tumors, and intraocular foreign bodies. A-scan ultrasonography measures the length of the eye and is primarily used to calculate intraocular lens power before cataract surgery. Ultrasound biomicroscopy (UBM) uses high-frequency ultrasound to create detailed images of the anterior segment structures, including the iris, ciliary body, and angle.
Corneal topography is a non-invasive imaging technique that maps the surface curvature of the cornea. This test is essential for diagnosing and managing conditions such as keratoconus, planning refractive surgery, and fitting specialty contact lenses. The topography device captures thousands of data points on the corneal surface and creates a color-coded map that highlights areas of steepness or flatness. Advanced corneal topography systems can also provide information about corneal thickness and elevation.
Specular microscopy is a specialized imaging technique that examines the corneal endothelium, the single layer of cells that lines the inner surface of the cornea. These cells are essential for maintaining corneal clarity by regulating fluid within the corneal tissue. Specular microscopy provides detailed images of the endothelial cells, allowing assessment of cell density, size, and shape. This test is particularly valuable for evaluating conditions such as Fuchs’ endothelial dystrophy, assessing corneal health before cataract surgery, and monitoring corneal transplants.
Electrophysiological tests measure the electrical responses of various cells in the visual system to visual stimuli. These tests include electroretinography (ERG), which measures the electrical responses of the retina’s photoreceptor and bipolar cells; electrooculography (EOG), which evaluates the function of the retinal pigment epithelium; and visual evoked potential (VEP), which measures the electrical activity in the visual cortex of the brain in response to visual stimuli. These tests are particularly useful for diagnosing and monitoring inherited retinal disorders, unexplained vision loss, and certain neurological conditions.
Gonioscopy is a specialized examination technique used to evaluate the drainage angle of the eye, the area where the iris meets the cornea. This test is essential for diagnosing and managing glaucoma, as it helps determine whether the angle is open (allowing normal drainage of aqueous humor) or closed (which can lead to angle-closure glaucoma). During gonioscopy, the ophthalmologist places a special contact lens with mirrors on the anesthetized eye, allowing direct visualization of the angle structures.
Pachymetry is the measurement of corneal thickness, typically using ultrasound or optical methods. Corneal thickness is an important factor in glaucoma diagnosis and management, as thin corneas may lead to underestimation of intraocular pressure and are associated with increased risk of glaucoma progression. Pachymetry is also used to evaluate candidates for refractive surgery and to monitor conditions such as corneal edema.
Anterior segment optical coherence tomography (AS-OCT) is an advanced imaging technique that provides high-resolution cross-sectional images of the anterior segment structures, including the cornea, iris, angle, and lens. AS-OCT is particularly useful for evaluating angle anatomy in glaucoma patients, assessing corneal diseases and conditions, and planning and evaluating outcomes of anterior segment surgery.
Confocal microscopy is an advanced imaging technique that provides high-magnification, high-resolution images of living corneal tissue at the cellular level. This non-invasive “optical biopsy” can detect and monitor various corneal conditions, including infections, dystrophies, and post-surgical changes, without the need for tissue sampling.
Adaptive optics is an emerging technology that corrects for optical aberrations in the eye to provide unprecedented resolution of retinal structures. This technique allows visualization of individual photoreceptor cells, retinal pigment epithelium cells, and capillary blood flow in the living retina. Adaptive optics has research applications and potential clinical uses in the early diagnosis and monitoring of retinal diseases.
Artificial intelligence (AI) is increasingly being integrated into ophthalmic diagnostics, particularly in the analysis of retinal images for conditions such as diabetic retinopathy, glaucoma, and macular degeneration. AI algorithms can analyze large datasets of images to detect patterns and abnormalities that might be missed by human observers, potentially improving the efficiency and accuracy of diagnosis, particularly in screening settings.
The diagnostic process in ophthalmology often involves the integration of multiple techniques to provide a comprehensive assessment of visual function and ocular health. The selection of appropriate tests depends on the patient’s symptoms, clinical findings, and suspected conditions. As technology continues to advance, diagnostic capabilities in ophthalmology continue to expand, offering earlier detection, more precise characterization of eye diseases, and improved monitoring of treatment outcomes.
These diagnostic techniques not only aid in the identification of eye diseases but also play a crucial role in monitoring disease progression and evaluating treatment effectiveness. Regular comprehensive eye examinations that incorporate appropriate diagnostic tests are essential for maintaining eye health, detecting conditions at their earliest stages, and implementing timely interventions to preserve vision. The ongoing development and refinement of diagnostic technologies promise to further enhance our ability to understand, diagnose, and treat eye disorders in the years to come.
Treatment Approaches in Ophthalmology
The field of ophthalmology offers a diverse array of treatment approaches for eye conditions, ranging from non-invasive interventions to complex surgical procedures. These treatments are designed to correct refractive errors, manage eye diseases, alleviate symptoms, and preserve or restore vision. The selection of appropriate treatment depends on the specific condition, its severity, the patient’s overall health, and individual preferences. Ophthalmic treatments continue to evolve rapidly, incorporating technological advances and innovative approaches that improve outcomes and enhance patient care.
Refractive error correction represents one of the most common treatment needs in ophthalmology. For centuries, eyeglasses have been the primary method of correcting refractive errors, and they remain a safe, effective, and non-invasive option. Modern eyeglasses offer numerous enhancements, including high-index lenses for thinner, lighter glasses; photochromic lenses that darken in sunlight; anti-reflective coatings to reduce glare; and progressive lenses that provide multiple focal powers without visible lines. Eyeglasses can correct myopia, hyperopia, astigmatism, and presbyopia, making them a versatile solution for refractive correction.
Contact lenses provide an alternative to eyeglasses and offer advantages such as a wider field of vision, freedom from frames, and the ability to participate in sports and other activities without obstruction. Various types of contact lenses are available, including soft lenses, rigid gas permeable (RGP) lenses, hybrid lenses, and specialty lenses for conditions like keratoconus. Soft lenses, made of flexible plastics that allow oxygen to pass through to the cornea, are the most commonly prescribed and can be designed for daily wear, extended wear, or disposable use. RGP lenses, though less comfortable initially, provide sharper vision for some individuals and are more durable than soft lenses. Contact lens care involves proper cleaning, disinfection, and regular replacement to prevent eye infections and complications.
Refractive surgery offers a permanent solution for refractive errors by reshaping the cornea to improve the eye’s focusing ability. The most common refractive surgery is laser-assisted in situ keratomileusis (LASIK), which involves creating a thin flap in the cornea, using a laser to reshape the underlying corneal tissue, and then repositioning the flap. LASIK can effectively correct myopia, hyperopia, and astigmatism, with most patients achieving 20/25 vision or better. Photorefractive keratectomy (PRK) is similar to LASIK but does not involve creating a corneal flap; instead, the laser is applied directly to the corneal surface after removing the outer layer (epithelium). PRK is often recommended for individuals with thin corneas or those at higher risk of flap complications.
Other refractive surgery options include phakic intraocular lenses (IOLs), which are implantable lenses placed in the eye without removing the natural lens; refractive lens exchange, which involves removing the natural lens and replacing it with an artificial lens; and intracorneal ring segments, which are small plastic rings inserted into the cornea to flatten its shape, primarily used for keratoconus. Each refractive surgery option has specific benefits, risks, and candidacy criteria that must be carefully evaluated for each patient.
Cataract surgery is one of the most commonly performed surgical procedures worldwide, with millions of operations conducted annually. Modern cataract surgery typically uses phacoemulsification, a technique that involves making a small incision in the cornea, creating an opening in the lens capsule, inserting a probe that uses ultrasound waves to break up the cloudy lens, and then removing the fragmented lens material. After removing the cataract, an artificial intraocular lens (IOL) is implanted to replace the natural lens and restore focusing power.
Various types of IOLs are available to address different visual needs. Monofocal IOLs provide clear vision at a single distance (usually far) and are the most commonly used lenses. Multifocal IOLs have multiple focal points to provide clear vision at various distances, reducing the need for reading glasses. Accommodating IOLs are designed to move within the eye in response to focusing efforts, providing a range of vision. Toric IOLs correct astigmatism in addition to addressing the cataract. The selection of an appropriate IOL depends on the patient’s visual needs, lifestyle, and ocular characteristics.
Glaucoma treatment aims to lower intraocular pressure to prevent or slow optic nerve damage and vision loss. The first-line treatment for most glaucoma patients is prescription eye drops that either reduce aqueous humor production or improve its outflow. Several classes of glaucoma medications are available, including prostaglandin analogs, beta-blockers, alpha agonists, carbonic anhydrase inhibitors, and rho kinase inhibitors. These medications are typically used once or twice daily and must be taken consistently to be effective.
When medications are insufficient or cause unacceptable side effects, laser treatment may be recommended. Selective laser trabeculoplasty (SLT) uses a low-energy laser to improve the drainage of aqueous humor through the eye’s trabecular meshwork. The procedure is typically performed in an outpatient setting and can lower intraocular pressure for several years. Laser peripheral iridotomy, which involves creating a small hole in the peripheral iris, is used to treat or prevent angle-closure glaucoma by providing an alternative pathway for aqueous humor to flow.
Surgical interventions for glaucoma include trabeculectomy, during which a small drainage fistula is created to allow aqueous humor to bypass the eye’s normal drainage system; glaucoma drainage devices, which are small tubes implanted to shunt aqueous humor from the eye to an external reservoir; and minimally invasive glaucoma surgery (MIGS), which encompasses various procedures that use microscopic equipment and tiny incisions to improve aqueous outflow with reduced risk compared to traditional glaucoma surgery.
Age-related macular degeneration (AMD) treatment depends on the type and severity of the condition. For dry AMD, management focuses on lifestyle modifications and nutritional supplements. The Age-Related Eye Disease Study 2 (AREDS2) formulation, which includes vitamins C and E, lutein, zeaxanthin, zinc, and copper, has been shown to reduce the risk of progression to advanced AMD in individuals with intermediate or advanced dry AMD. Smoking cessation, blood pressure control, and a diet rich in leafy green vegetables and fish may also help slow AMD progression.
For wet AMD, the standard treatment is anti-vascular endothelial growth factor (anti-VEGF) therapy, which involves injecting medications that block the activity of VEGF, a protein that promotes the growth of abnormal blood vessels. Common anti-VEGF medications include ranibizumab, aflibercept, and bevacizumab. These injections are typically administered monthly or at extended intervals and have been shown to stabilize vision in the majority of patients and improve vision in approximately one-third of patients. Other treatments for wet AMD include photodynamic therapy, which uses a light-activated drug to seal leaking blood vessels, and thermal laser photocoagulation, which is less commonly used today but may be appropriate for certain cases.
Diabetic retinopathy management involves both systemic control of diabetes and specific ophthalmic treatments. Good blood sugar control, blood pressure management, and cholesterol control are essential for slowing the progression of diabetic retinopathy. For diabetic macular edema (swelling of the macula), anti-VEGF injections are the first-line treatment, with corticosteroids (injected or implanted) as an alternative. For proliferative diabetic retinopathy, panretinal photocoagulation (PRP) laser treatment is used to create scattered laser burns throughout the peripheral retina, reducing the stimulus for abnormal blood vessel growth. Vitrectomy surgery may be necessary for advanced cases with significant bleeding, retinal detachment, or tractional membranes.
Dry eye syndrome treatment focuses on restoring and maintaining the tear film to reduce symptoms and prevent ocular surface damage. Artificial tears are the first-line treatment and are available in various formulations, including preservative-free options for individuals who use them frequently. For moderate to severe dry eye, prescription medications such as cyclosporine and lifitegrast can reduce inflammation and increase tear production. Punctal plugs, small devices inserted into the tear drainage openings, can help preserve natural tears on the ocular surface. Other treatment approaches include omega-3 fatty acid supplements, warm compresses and eyelid massage for meibomian gland dysfunction, moisture chamber glasses, and autologous serum eye drops for severe cases.
Inflammatory eye conditions, such as uveitis, are typically treated with corticosteroids to reduce inflammation. These can be administered as eye drops, periocular injections, intraocular injections, or oral medications, depending on the severity and location of inflammation. For chronic or recurrent uveitis, immunosuppressive medications such as methotrexate, azathioprine, or mycophenolate may be necessary to control inflammation and reduce steroid dependence. Biologic agents, including tumor necrosis factor-alpha inhibitors, are increasingly used for severe or refractory uveitis.
Infectious eye conditions, such as bacterial, viral, or fungal infections, require targeted antimicrobial therapy. Bacterial conjunctivitis and keratitis are typically treated with antibiotic eye drops or ointments. Viral conjunctivitis, usually caused by adenovirus, is generally self-limiting but may be treated with supportive care and, in severe cases, topical corticosteroids to reduce inflammation. Herpes simplex virus keratitis requires antiviral medications such as acyclovir or ganciclovir in eye drop or oral form. Fungal keratitis, though less common, can be challenging to treat and requires antifungal medications, often for extended periods.
Corneal transplantation, or keratoplasty, may be necessary for conditions that significantly affect corneal clarity, such as advanced keratoconus, corneal scarring, or corneal edema. Penetrating keratoplasty (PK), the traditional approach, involves replacing the full thickness of the cornea with donor tissue. Endothelial keratoplasty, including Descemet’s stripping endothelial keratoplasty (DSEK) and Descemet’s membrane endothelial keratoplasty (DMEK), replaces only the diseased endothelial layer, resulting in faster visual recovery and reduced risk of rejection. Anterior lamellar keratoplasty replaces only the front layers of the cornea while preserving the patient’s healthy endothelium.
Retinal surgery encompasses various procedures to treat conditions affecting the retina and vitreous. Vitrectomy involves removing the vitreous gel and replacing it with a clear solution, allowing the surgeon to repair retinal detachments, remove scar tissue, treat macular holes, or address vitreous hemorrhage. Scleral buckling is a procedure used to repair retinal detachments by placing a silicone band around the outside of the eye to push the wall of the eye against the detached retina. Pneumatic retinopexy is another technique for retinal detachment repair that involves injecting a gas bubble into the eye to push the retina back into place, often combined with laser or cryotherapy to seal the tear.
Oculoplastic surgery involves procedures to correct abnormalities of the eyelids, orbit, and lacrimal system. Blepharoplasty, one of the most common oculoplastic procedures, removes excess skin and fat from the upper and/or lower eyelids, improving both appearance and visual field in cases of significant upper eyelid drooping (ptosis). Ptosis repair specifically addresses drooping of the upper eyelid by tightening the levator muscle. Ectropion and entropion repair correct outward or inward turning of the eyelids, respectively. Orbital surgery may be necessary for conditions such as thyroid eye disease, orbital tumors, or trauma.
Strabismus surgery adjusts the position of the eye muscles to correct misalignment of the eyes. The procedure involves weakening, strengthening, or repositioning the extraocular muscles to improve eye alignment and, in some cases, restore binocular vision. Strabismus surgery is typically performed on an outpatient basis and may be combined with other treatments such as prism glasses or vision therapy for optimal results.
Neuro-ophthalmology addresses visual problems related to the nervous system, including conditions such as optic neuritis, ischemic optic neuropathy, and double vision from cranial nerve palsies. Treatment depends on the underlying cause and may involve medications (such as corticosteroids for optic neuritis), management of systemic conditions (like controlling blood pressure in ischemic optic neuropathy), or prisms to correct double vision.
Pediatric ophthalmology focuses on eye conditions in children, including amblyopia, strabismus, congenital cataracts, and refractive errors. Treatment approaches are often similar to those for adults but require special considerations for the developing visual system. Amblyopia treatment typically involves patching the stronger eye or using atropine drops to blur vision in the stronger eye, forcing the weaker eye to work harder. Pediatric cataract surgery requires prompt intervention to prevent permanent vision loss and often involves additional procedures to manage amblyopia.
Emerging treatments in ophthalmology include gene therapy for inherited retinal diseases, stem cell therapy to replace damaged retinal cells, and sustained-release drug delivery systems to provide long-term treatment with fewer interventions. These innovative approaches hold promise for conditions that previously had limited treatment options and represent the cutting edge of ophthalmic care.
The selection of appropriate treatment in ophthalmology requires careful consideration of the specific condition, its severity, the patient’s overall health, visual needs, and personal preferences. Ophthalmologists work closely with patients to develop individualized treatment plans that balance effectiveness, safety, and quality of life. As research continues to advance our understanding of eye diseases and their mechanisms, new treatment approaches continue to emerge, offering hope for improved outcomes and quality of life for individuals with eye conditions.
Subspecialties in Ophthalmology