What Are Airborne Diseases? Navigating the Invisible Threat
We often hear about diseases spreading through the air, particularly in crowded spaces or during outbreaks. These are known as airborne diseases, and understanding how they work is fundamental to protecting ourselves and our communities. Unlike illnesses spread through contaminated food or water, or direct physical contact, airborne diseases utilize the very medium we share – the air we breathe – as their primary mode of transport. This makes them particularly challenging to control and a significant focus of public health efforts worldwide.
In this article, we will delve into the science behind airborne transmission, explore common examples of these diseases, discuss their symptoms, and crucially, outline the strategies we can collectively employ to prevent their spread. By understanding this invisible threat, we empower ourselves to take informed actions that contribute to healthier environments for everyone.
The Science of Airborne Transmission: How Pathogens Take Flight
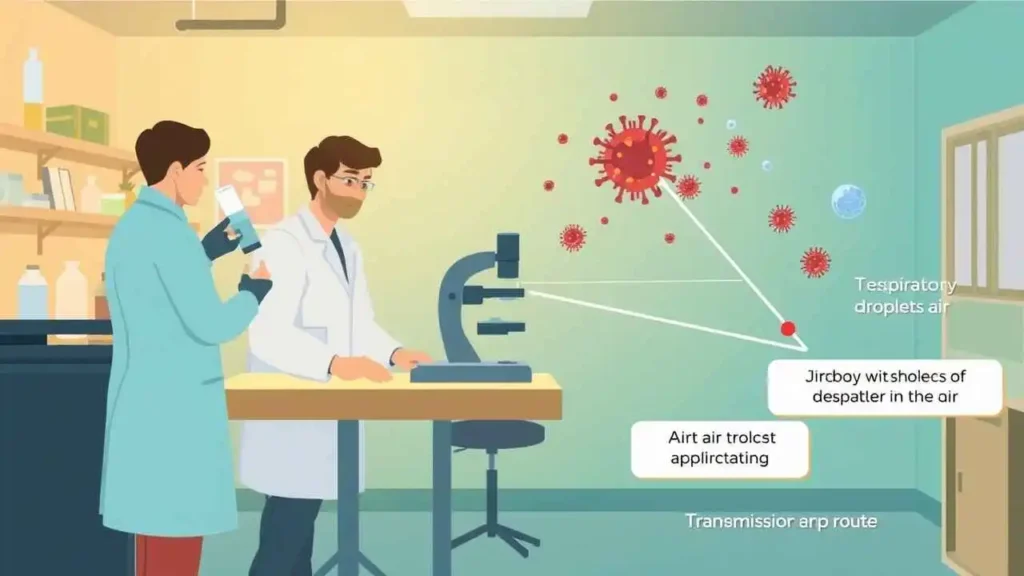
At its core, airborne transmission occurs when tiny particles containing infectious pathogens are expelled into the air and inhaled by a susceptible individual. These particles are typically generated when an infected person breathes, talks, sings, coughs, or sneezes.
We can primarily categorize these infectious particles into two types based on their size and behavior:
- Respiratory Droplets: These are relatively larger particles (generally > 5-10 micrometers in diameter). When expelled, they are heavily influenced by gravity and tend to fall out of the air quickly, usually within a few feet of the source. While they can carry pathogens, their range is limited, often leading to transmission only when people are in close proximity.
- Aerosols (or Droplet Nuclei): These are much smaller particles (generally < 5-10 micrometers in diameter). Due to their small size and lighter weight, they can remain suspended in the air for longer periods – sometimes minutes or even hours – and travel further distances on air currents. This is where the term “airborne” transmission is most accurately applied, describing diseases where these smaller, lingering particles are a significant mode of spread over longer ranges or beyond immediate proximity.
The key mechanism for infection with an airborne disease is inhalation. When we breathe in air containing these infectious aerosols, the pathogens can reach our respiratory tract, where they may establish an infection if conditions are favorable and our immune system doesn’t effectively fight them off.
Several factors influence the likelihood and extent of airborne transmission in a given environment:
- Ventilation: This is perhaps the most critical factor. Well-ventilated spaces, whether through natural airflow (open windows) or mechanical systems (HVAC), help to dilute and remove infectious aerosols from the air, reducing our exposure. Poorly ventilated, crowded indoor spaces are high-risk environments.
- Particle Size: As discussed, smaller particles (aerosols) stay airborne longer and travel further than larger droplets. Diseases spread primarily via aerosols are harder to contain through distance alone.
- Environmental Conditions: Factors like humidity and temperature can affect how long viruses or bacteria remain viable in the air.
- Duration of Exposure: The longer we spend in a shared airspace with an infectious person, the higher the chance we will inhale a sufficient dose of airborne particles to become infected.
- Activity Level: Activities that involve forced exhalation, such as singing, shouting, or heavy exercise, can generate more infectious aerosols and project them further compared to quiet breathing.
Understanding these dynamics helps us appreciate why certain measures are more effective than others in preventing airborne spread.
Common Examples of Airborne Diseases
Many common and serious infectious diseases are primarily or significantly transmitted via airborne routes. Here are some notable examples that we are likely familiar with:
| Disease | Causative Agent | Primary Transmission Type | Select Key Symptoms | Prevention Methods (Partial List) |
| Measles | Measles virus | Aerosols | Rash, fever, cough, runny nose, conjunctivitis | Vaccination (MMR), Isolation |
| Tuberculosis | Mycobacterium tuberculosis | Aerosols | Persistent cough, chest pain, weight loss, fever | Vaccination (BCG – varies), Treatment, Isolation |
| Influenza | Influenza viruses (A, B, C) | Droplets & Aerosols | Fever, cough, sore throat, body aches, fatigue | Vaccination (Annual Flu Shot), Masks, Hygiene, Ventilation |
| Chickenpox | Varicella-zoster virus | Aerosols & Direct Contact | Itchy rash, fever, fatigue | Vaccination (Varicella vaccine), Isolation |
| COVID-19 | SARS-CoV-2 virus | Droplets & Aerosols | Fever, cough, fatigue, loss of taste/smell | Vaccination, Masks, Ventilation, Testing, Isolation, Hygiene |
| Common Cold | Various Rhinovirus strains, etc. | Droplets & Aerosols | Runny nose, sore throat, cough, congestion | Hygiene, Avoiding close contact, Ventilation, Masks (can help) |
| Mumps | Mumps virus | Droplets & Aerosols | Swollen salivary glands, fever, headache | Vaccination (MMR) |
Note: Transmission routes can sometimes involve multiple mechanisms (e.g., indirect contact via contaminated surfaces), but airborne transmission is a significant factor for these diseases.
It’s important to remember that while some diseases listed, like the flu or common cold, are often associated with larger droplets and require closer contact, the aerosol route can still play a role, particularly in poorly ventilated spaces, contributing to wider spread than simple large droplet transmission alone would suggest. Diseases like Measles and Tuberculosis are classic examples of pathogens highly efficient at aerosol transmission, making them incredibly contagious.
Recognizing Symptoms and Seeking Diagnosis