Arthroscopy and Trauma: A Comprehensive Guide to Diagnosis, Treatment and Recovery
Introduction
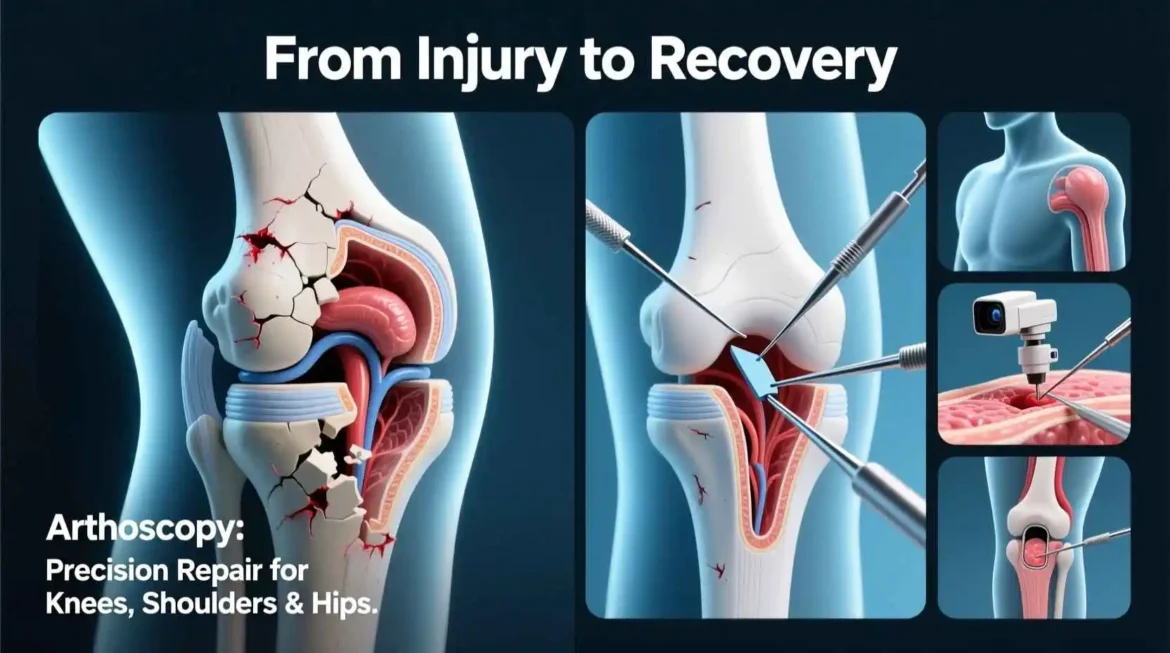
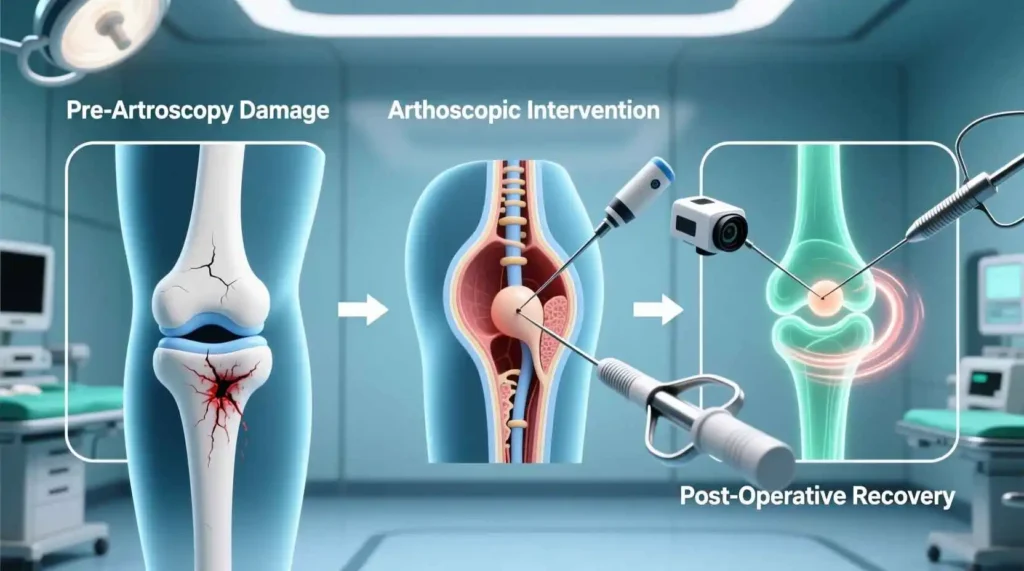
Arthroscopy has revolutionized the field of orthopedic medicine, providing minimally invasive solutions for diagnosing and treating a wide range of joint injuries and conditions. When combined with trauma care, this advanced surgical technique has transformed outcomes for patients with joint injuries resulting from accidents, sports activities, and other traumatic events. This comprehensive guide explores the intricate relationship between arthroscopy and trauma, examining how these specialized procedures are used to diagnose, treat, and rehabilitate joint injuries with precision and efficiency.
The evolution of arthroscopic techniques represents one of the most significant advances in orthopedic surgery over the past century. What once required large incisions and extensive recovery periods can now often be accomplished through small portals, minimizing tissue damage and accelerating rehabilitation. This progress has been particularly beneficial in trauma cases, where timely intervention and minimal additional trauma to already injured tissues can significantly impact patient outcomes.
Understanding arthroscopy in the context of trauma requires knowledge of both the technological aspects of the procedure and the complex biomechanics of joint injuries. This guide will delve into the fundamental principles of arthroscopic surgery, explore its applications across various joints and injury types, examine the latest technological advances, and provide insights into rehabilitation protocols and future directions in the field.
Whether you are a medical student, healthcare professional, patient, or simply someone interested in orthopedic medicine, this comprehensive resource will provide valuable information about how arthroscopic techniques are changing the landscape of trauma care, offering patients less invasive options, faster recoveries, and improved functional outcomes.
The Evolution of Arthroscopic Surgery
The history of arthroscopy reflects the ingenuity and persistence of orthopedic surgeons seeking less invasive ways to visualize and treat joint pathology. This journey from early diagnostic tools to sophisticated therapeutic interventions has transformed orthopedic practice, particularly in the management of traumatic joint injuries.
Early Beginnings
The concept of looking inside a joint without fully opening it dates back to the early 20th century. In 1919, Japanese physician Kenji Takagi performed the first recorded arthroscopy using a cystoscope to examine the knee joint of a patient with tuberculosis. This pioneering effort laid the groundwork for minimally invasive joint examination, though the technology was rudimentary by today’s standards.
Throughout the 1930s and 1940s, Takagi and his colleagues continued to refine their techniques, developing instruments with improved optics and illumination. However, these early arthroscopes had significant limitations, including poor image quality, limited field of view, and cumbersome designs that made practical application challenging.
Mid-Century Advances
The 1950s and 1960s saw significant improvements in arthroscopic technology, largely driven by innovations in optics and fiber optics. In 1957, Masaki Watanabe, who had studied under Takagi, developed the first practical arthroscope using improved optical systems. Watanabe’s instrument featured a wider field of view and better illumination, making it more useful for both diagnosis and simple therapeutic procedures.
During this period, arthroscopy remained primarily a diagnostic tool, with limited therapeutic applications. Surgeons could visualize joint pathology but had few instruments capable of performing interventions through the small arthroscopic portals. The first arthroscopic surgical procedures were relatively simple, such as removing loose bodies or performing biopsies.
The Arthroscopic Revolution
The true revolution in arthroscopic surgery began in the 1970s and accelerated through the 1980s and 1990s. Several key developments drove this transformation:
Improved Optics: Advances in rod-lens optics and fiber optic lighting dramatically improved image quality, allowing surgeons to see joint structures with unprecedented clarity.
Miniaturization: The development of smaller, more flexible arthroscopes enabled access to tighter joint spaces and reduced tissue trauma during portal placement.
Specialized Instruments: As surgeons recognized the potential for therapeutic arthroscopy, instrument manufacturers developed an expanding array of tools designed specifically for arthroscopic procedures, including probes, graspers, shavers, and eventually powered instruments.
Video Technology: The integration of video cameras with arthroscopes was perhaps the most significant advance. Instead of looking directly through the eyepiece, surgeons could now view the joint on a monitor, allowing for better visualization, improved ergonomics, and the ability to involve the entire surgical team in the procedure.
Modern Arthroscopy
Today’s arthroscopic systems bear little resemblance to those early instruments. High-definition cameras, sophisticated light sources, and specialized instruments have made arthroscopy one of the most commonly performed orthopedic procedures. The technology continues to evolve, with innovations such as:
Digital Imaging: High-definition and even 4K digital imaging systems provide exceptional detail, allowing surgeons to identify subtle pathology that might be missed with older systems.
Three-Dimensional Arthroscopy: Some systems now offer 3D visualization, providing improved depth perception and spatial orientation during complex procedures.
Navigation Systems: Computer-assisted navigation can help guide arthroscopic procedures, particularly in cases involving complex anatomy or precise placement of implants.
Robotic Assistance: While still in early stages, robotic systems are being developed to enhance the precision of arthroscopic procedures, particularly for tasks requiring extreme accuracy.
Arthroscopy in Trauma Care
The application of arthroscopic techniques to trauma care has followed a similar evolutionary path. Initially used primarily for diagnostic purposes in traumatic joint injuries, arthroscopy has gradually expanded to become a primary treatment modality for many traumatic conditions.
In the early days, trauma cases were often considered contraindications for arthroscopic surgery due to concerns about fluid extravasation, compartment syndrome, and the technical challenges of operating in acutely injured joints. As techniques improved and surgeons gained experience, these concerns were largely addressed, and arthroscopy became an integral part of trauma management.
Today, arthroscopic techniques are used to treat a wide range of traumatic conditions, including ligament tears, meniscal injuries, fractures, cartilage defects, and instability patterns across multiple joints. The minimally invasive nature of arthroscopy is particularly beneficial in trauma cases, where additional surgical trauma can potentially compromise healing and recovery.
Fundamental Principles of Arthroscopic Surgery
Arthroscopic surgery relies on several fundamental principles that distinguish it from traditional open surgical techniques. Understanding these principles is essential for appreciating how arthroscopy has transformed the management of traumatic joint injuries.
Minimally Invasive Approach
The core principle of arthroscopic surgery is the minimally invasive approach, which aims to achieve therapeutic goals while minimizing damage to surrounding tissues. This is accomplished through:
Small Incisions: Arthroscopic procedures typically use incisions measuring only a few millimeters, called portals, through which instruments are introduced. This contrasts sharply with open procedures, which may require incisions of several centimeters or more.
Tissue Preservation: By avoiding large incisions and extensive dissection, arthroscopic procedures preserve blood supply to tissues, minimize damage to soft tissues, and reduce postoperative pain and scarring.
Targeted Intervention: Arthroscopy allows surgeons to directly visualize and address specific pathology without disturbing unaffected structures. This precision is particularly valuable in trauma cases, where the goal is to repair damaged structures while preserving healthy tissue.
Fluid Management
Arthroscopic procedures rely on fluid management to create and maintain a working space within the joint. This involves several key components:
Distention: The joint is distended with irrigation fluid to create space for instrument manipulation and visualization. This distention helps separate soft tissue structures, allowing for better visualization and access.
Irrigation: Continuous flow of irrigation fluid clears the surgical field of blood and debris, maintaining a clear view for the surgeon. The irrigation fluid also helps control minor bleeding through hydrostatic pressure.
Pressure Control: Maintaining appropriate pressure within the joint is crucial for adequate visualization while preventing complications such as fluid extravasation into surrounding tissues. Modern arthroscopy systems include sophisticated pumps that precisely control fluid pressure and flow.
Triangulation
Triangulation is a fundamental concept in arthroscopic surgery that refers to the positioning of instruments and the arthroscope to effectively manipulate structures within the joint. This principle involves:
Portal Placement: Strategic placement of portals allows instruments to approach the target structure from different angles, facilitating manipulation and treatment.
Instrument Orientation: Surgeons must develop a three-dimensional understanding of instrument position based on two-dimensional images on the screen. This spatial orientation is a skill that requires significant experience to master.
Coordinated Movement: Effective triangulation requires coordinated movement between the arthroscope and instruments, allowing the surgeon to work efficiently while maintaining visualization.
Magnification and Visualization
Arthroscopic procedures provide magnified views of joint structures, offering several advantages:
Detailed Visualization: The magnification provided by arthroscopes allows surgeons to see fine details of joint pathology that might be missed with the naked eye during open procedures.
Improved Diagnosis: The ability to visualize structures directly and dynamically (moving the joint through ranges of motion) enhances diagnostic accuracy, particularly in complex trauma cases.
Documentation: Modern arthroscopic systems allow for high-quality photo and video documentation, which is valuable for patient education, research, and quality improvement.
Ergonomics and Operator Fatigue
Arthroscopic surgery presents unique ergonomic challenges that differ from traditional open procedures:
Body Positioning: Surgeons must maintain comfortable, stable positions during often lengthy procedures to minimize fatigue and ensure precise instrument control.
Monitor Placement: Proper positioning of video monitors is essential to reduce neck strain and optimize visualization. Many operating rooms now feature multiple monitors positioned for optimal viewing by the surgical team.
Instrument Design: Modern arthroscopic instruments are designed with ergonomics in mind, featuring handles that reduce hand fatigue and improve control during delicate procedures.
Applications in Trauma Care
These fundamental principles make arthroscopy particularly valuable in the management of traumatic joint injuries:
Reduced Additional Trauma: In patients who have already sustained traumatic injuries, the minimally invasive nature of arthroscopy minimizes additional surgical trauma, potentially improving outcomes.
Early Intervention: Arthroscopy allows for earlier intervention in some traumatic conditions, as the risks associated with the procedure are generally lower than with open surgery.
Comprehensive Assessment: The ability to thoroughly visualize the joint allows for comprehensive assessment of traumatic pathology, including injuries that might not be apparent on preoperative imaging.
Combined Procedures: Arthroscopy can be combined with other surgical techniques in trauma cases, such as percutaneous fixation of fractures, providing a comprehensive approach to complex injuries.
Understanding these fundamental principles provides a foundation for appreciating how arthroscopic techniques have advanced the field of trauma care, offering patients less invasive options with potentially faster recoveries and improved outcomes.
Arthroscopic Anatomy and Joint Access
Successful arthroscopic surgery requires a thorough understanding of normal joint anatomy and the principles of safe joint access. This knowledge is particularly critical in trauma cases, where normal anatomical relationships may be disrupted by injury. This section explores the anatomical considerations and access techniques essential for arthroscopic procedures across various joints.
Anatomical Considerations
Arthroscopic surgery demands a detailed knowledge of joint anatomy, including:
Bony Landmarks: Understanding the relationship between superficial bony landmarks and deeper joint structures is essential for safe portal placement and navigation during arthroscopic procedures. In trauma cases, these landmarks may be altered by fractures or dislocations.
Neurovascular Structures: Awareness of the location of nerves and blood vessels relative to standard portal sites is crucial to avoid iatrogenic injury during portal placement and instrument manipulation. This is particularly important in trauma cases where swelling or hematoma may make these structures less palpable.
Joint Capsule and Ligaments: The joint capsule and ligaments serve as important boundaries during arthroscopic procedures. In traumatic injuries, these structures may be torn, lax, or disrupted, affecting joint stability and the surgeon’s ability to maintain adequate distention.
Muscle and Tendon Anatomy: Understanding the relationship between muscles, tendons, and the joint is important for planning portal placement and avoiding injury to these structures during instrument introduction and manipulation.
Knee Arthroscopy Anatomy and Access
The knee is the most commonly accessed joint for arthroscopic procedures, with well-established anatomical considerations and portal placements:
Standard Portals: The anterolateral and anteromedial portals are the primary working portals for knee arthroscopy. These are positioned just lateral or medial to the patellar tendon, approximately 1 cm above the joint line. Proper placement avoids injury to the patellar tendon, infrapatellar fat pad, and neurovascular structures.
Accessory Portals: Additional portals may be used for specific procedures, including posteromedial, posterolateral, and suprapatellar portals. Each has specific anatomical considerations to avoid neurovascular injury.
Compartmental Anatomy: The knee is divided into three compartments—medial and lateral tibiofemoral compartments and the patellofemoral compartment. Each must be systematically examined during diagnostic arthroscopy, with particular attention to areas commonly affected by trauma such as the menisci, cruciate ligaments, and articular cartilage.
Trauma-Specific Considerations: In traumatic knee injuries, the anatomy may be significantly altered. Hemarthrosis can obscure visualization, ligamentous injuries may affect joint stability, and fractures may create loose bodies or alter normal anatomical relationships. The surgeon must be prepared to adapt standard techniques to these altered conditions.
Shoulder Arthroscopy Anatomy and Access
Shoulder arthroscopy presents unique anatomical challenges due to the joint’s complexity and proximity to neurovascular structures:
Beach Chair vs. Lateral Decubitus: Shoulder arthroscopy can be performed in either the beach chair or lateral decubitus position, each with advantages and disadvantages. The beach chair position allows easier conversion to open surgery if needed, while the lateral decubitus position provides better traction and visualization of the inferior joint.
Standard Portals: The posterior portal is typically established first, located approximately 2 cm inferior and 1 cm medial to the posterolateral corner of the acromion. From this starting point, additional portals including anterior, anterosuperior, and lateral portals can be established under direct visualization.
Neurovascular Considerations: The axillary nerve and posterior circumflex humeral artery are at particular risk during shoulder arthroscopy, especially during establishment of the posterior portal and when working in the inferior aspect of the joint. The musculocutaneous nerve is also at risk during anterior portal placement.
Trauma-Specific Considerations: In traumatic shoulder conditions such as instability or rotator cuff tears, the surgeon must be prepared to address altered anatomy. Bankart lesions, Hill-Sachs defects, and rotator cuff tears all require specific approaches and may necessitate additional portals or specialized instruments.
Ankle Arthroscopy Anatomy and Access
Ankle arthroscopy requires careful attention to the dense neurovascular network surrounding the joint:
Standard Portals: The anteromedial and anterolateral portals are the primary working portals for anterior ankle arthroscopy. These must be placed carefully to avoid injury to the superficial peroneal nerve laterally and the saphenous nerve and great saphenous vein medially.
Posterior Portals: Posterior ankle arthroscopy uses posteromedial and posterolateral portals, placed with particular attention to avoiding the posterior neurovascular bundle, which includes the tibial nerve, posterior tibial artery, and veins.
Anatomical Landmarks: Key landmarks for portal placement include the medial and lateral malleoli, the Achilles tendon, the extensor hallucis longus tendon, and the peroneal tendons. These landmarks may be obscured by swelling or hematoma in trauma cases.
Trauma-Specific Considerations: Traumatic ankle conditions such as osteochondral lesions, syndesmotic injuries, and intra-articular fractures require specialized approaches. The surgeon must be prepared to address altered anatomy and may need to adapt standard techniques based on the specific injury pattern.
Wrist Arthroscopy Anatomy and Access
Wrist arthroscopy is technically demanding due to the small joint size and proximity of neurovascular structures:
Standard Portals: The 3-4 and 4-5 portals are the primary working portals for wrist arthroscopy, named for their location between the dorsal extensor compartments. The 6R portal is also commonly used, particularly for radial-sided pathology.
Anatomical Considerations: The superficial branches of the radial nerve and the dorsal sensory branch of the ulnar nerve are at risk during portal placement. The extensor tendons must also be carefully avoided during portal establishment.
Joint Anatomy: The wrist is divided into radiocarpal and midcarpal compartments, each requiring separate examination. The triangular fibrocartilage complex (TFCC) is a common site of pathology and requires careful evaluation.
Trauma-Specific Considerations: Traumatic wrist conditions such as TFCC tears, scapholunate ligament injuries, and intra-articular fractures present unique challenges. The small joint size makes visualization and instrument manipulation more difficult, particularly in the presence of swelling or hematoma.
Hip Arthroscopy Anatomy and Access