Hip arthroscopy is technically challenging due to the joint’s deep location and constrained ball-and-socket configuration:
Traction Requirements: Hip arthroscopy typically requires traction to separate the femoral head from the acetabulum, creating space for instrument introduction. This must be carefully balanced against the risk of neurovascular injury from excessive traction.
Portal Placement: Standard portals include the anterolateral, anterior, and posterolateral portals. Each must be placed carefully to avoid injury to neurovascular structures, including the femoral nerve, lateral femoral cutaneous nerve, and superior gluteal nerve.
Compartmental Anatomy: The hip joint is divided into central and peripheral compartments, each requiring separate examination. The labrum, acetabular cartilage, and femoral head cartilage are key structures to evaluate.
Trauma-Specific Considerations: Traumatic hip conditions such as labral tears, ligamentum teres injuries, and femoroacetabular impingement (FAI) may result from acute trauma. The surgeon must be prepared to address these conditions while navigating the complex anatomy of the hip joint.
Elbow Arthroscopy Anatomy and Access
Elbow arthroscopy is considered one of the more technically demanding arthroscopic procedures due to the joint’s complex anatomy and proximity to neurovascular structures:
Portal Placement: Common portals include the anteromedial, anterolateral, direct lateral, and posterior portals. Each must be placed with careful attention to avoiding neurovascular structures, particularly the median nerve, radial nerve, and ulnar nerve.
Anatomical Considerations: The elbow is a complex joint with multiple articulations, including humeroulnar, humeroradial, and proximal radioulnar joints. The capsule is relatively tight, making joint distention challenging.
Compartmental Anatomy: The elbow is typically divided into anterior and posterior compartments, each requiring separate examination and potentially different portal placements.
Trauma-Specific Considerations: Traumatic elbow conditions such as loose bodies, osteochondral lesions, and capsular injuries present unique challenges. The surgeon must be particularly cautious about neurovascular structures in the swollen, traumatized elbow.
General Principles of Safe Joint Access
Regardless of the specific joint, several general principles apply to safe arthroscopic access:
Skin Marking: Preoperative marking of anatomical landmarks and planned portal sites is essential, particularly in trauma cases where normal anatomy may be distorted.
Joint Distention: Adequate joint distention before portal placement helps protect intra-articular structures from inadvertent injury during instrument introduction.
Blunt Dissection: Using blunt trocars for initial portal establishment helps protect neurovascular structures from sharp injury.
Direct Visualization: Whenever possible, portals should be established under direct visualization, with initial portals created using anatomical landmarks and subsequent portals created under direct arthroscopic visualization.
Pressure Monitoring: Monitoring fluid pressure during the procedure helps prevent complications such as compartment syndrome, particularly in trauma cases where tissue compliance may be altered.
Understanding these anatomical considerations and access techniques is fundamental to safe and effective arthroscopic surgery, particularly in the management of traumatic joint injuries where normal anatomy may be disrupted and the risks of complications may be higher.
Arthroscopic Management of Specific Traumatic Conditions
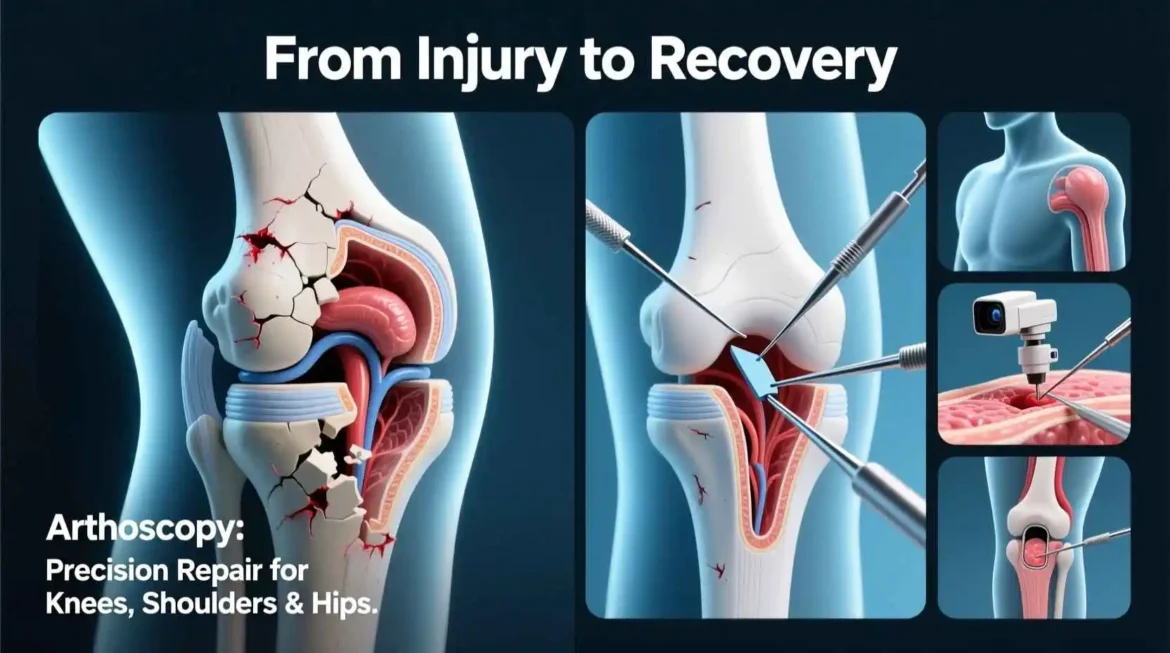
Arthroscopic techniques have become integral to the management of many traumatic joint conditions, offering minimally invasive solutions that preserve tissue integrity while addressing the pathological changes resulting from injury. This section examines the application of arthroscopic approaches to specific traumatic conditions across various joints.
Knee Trauma
The knee is perhaps the most frequently addressed joint in arthroscopic trauma surgery, with several common conditions amenable to arthroscopic management:
Anterior Cruciate Ligament (ACL) Tears: ACL tears are among the most common traumatic knee injuries, particularly in sports-related trauma. Arthroscopic ACL reconstruction has become the gold standard for treating these injuries, with techniques continuing to evolve.
Diagnostic Arthroscopy: Initial arthroscopic evaluation confirms the diagnosis and allows assessment of associated injuries such as meniscal tears, chondral damage, or other ligamentous injuries that may affect treatment planning.
Graft Preparation and Placement: Various graft options exist, including patellar tendon autograft, hamstring autograft, and allograft options. The arthroscopic approach allows precise anatomical placement of the graft, with attention to tunnel position, graft tension, and fixation.
Rehabilitation Considerations: Postoperative rehabilitation protocols have evolved significantly, with earlier weight-bearing and range of motion now emphasized in many cases. The arthroscopic approach facilitates this accelerated rehabilitation by minimizing surgical trauma.
Meniscal Tears: Traumatic meniscal tears often occur in conjunction with ligamentous injuries or as isolated injuries from twisting mechanisms.
Meniscal Repair vs. Meniscectomy: The arthroscopic approach allows detailed evaluation of tear pattern, location, and tissue quality, informing the decision between repair and partial meniscectomy. Repair is generally preferred for tears in the vascularized red-red or red-white zones, particularly in younger patients.
Repair Techniques: Various arthroscopic repair techniques exist, including inside-out, outside-in, and all-inside approaches. Each has specific indications and technical considerations.
Complex Tears: Bucket-handle tears, radial tears, and root tears present specific challenges that require specialized arthroscopic techniques and careful consideration of repairability.
Patellar Dislocations: Acute patellar dislocations can result in medial patellofemoral ligament (MPFL) injury, osteochondral fractures, and loose bodies.
Diagnostic Evaluation: Arthroscopy allows detailed evaluation of associated pathology, including osteochondral fractures of the patella or lateral femoral condyle and loose bodies that may require removal.
MPFL Reconstruction: For recurrent dislocations or cases with significant MPFL injury, arthroscopic or arthroscopically assisted MPFL reconstruction may be indicated. This procedure typically involves graft fixation at the patella and femur with careful attention to isometry and graft tension.
Loose Body Removal: Loose bodies resulting from osteochondral injury can be effectively removed arthroscopically, preventing mechanical symptoms and further joint damage.
Tibial Plateau Fractures: Certain tibial plateau fractures can be addressed with arthroscopic assistance, particularly low-energy fractures with minimal comminution.
Arthroscopic Assessment: Direct visualization of the articular surface allows for more accurate assessment of fracture reduction than fluoroscopy alone.
Reduction and Fixation: Arthroscopic guidance can assist with fracture reduction and placement of subchondral screws, potentially improving the accuracy of reduction while minimizing soft tissue dissection.
Associated Injuries: Arthroscopy allows for identification and treatment of associated meniscal or ligamentous injuries that may not be apparent on preoperative imaging.
Shoulder Trauma
The shoulder joint is particularly susceptible to traumatic injury, with several conditions amenable to arthroscopic management:
Bankart Lesions and Instability: Anterior shoulder instability often results from traumatic dislocation, with Bankart lesions (detachment of the anterior labrum and inferior glenohumeral ligament from the glenoid rim) being the most common pathological finding.
Diagnostic Arthroscopy: Arthroscopy provides detailed evaluation of the labral injury, capsular laxity, and associated pathology such as Hill-Sachs defects or rotator cuff tears.
Labral Repair: Arthroscopic Bankart repair involves reattachment of the labrum and capsule to the glenoid rim using suture anchors. This technique has evolved significantly, with improved anchors and instrumentation leading to better outcomes.
Capsular Plication: In cases of significant capsular laxity, arthroscopic capsular plication (tightening) may be performed in conjunction with labral repair to address multidirectional instability.
Rotator Cuff Tears: Traumatic rotator cuff tears can result from falls, direct blows, or forceful abduction/external rotation injuries.
Tear Pattern Assessment: Arthroscopy allows detailed evaluation of tear size, pattern, tissue quality, and retraction, informing decisions about repairability and technique.
Repair Techniques: Various arthroscopic repair techniques exist, including single-row, double-row, and transosseous equivalent repairs. The choice depends on tear pattern, tissue quality, and surgeon preference.
Subacromial Decompression: In cases with associated impingement, arthroscopic subacromial decompression may be performed concurrently with rotator cuff repair to address contributing factors.
SLAP Lesions: Superior labral anterior to posterior (SLAP) lesions can result from traumatic superior compression of the shoulder, such as from a fall onto an outstretched arm.
Classification and Treatment: SLAP lesions are classified into several types based on the pattern of labral involvement. Treatment varies from debridement to repair, depending on the type and patient factors.
Biceps Tenodesis: In cases of SLAP lesions with associated biceps pathology, biceps tenodesis (detachment and reattachment of the biceps tendon) may be performed in conjunction with labral repair.
Ankle Trauma
Ankle arthroscopy has become increasingly valuable in the management of traumatic ankle conditions:
Osteochondral Lesions: Osteochondral lesions of the talus (OLTs) often result from traumatic ankle injuries, particularly inversion injuries.
Diagnostic Evaluation: Arthroscopy provides the most accurate assessment of lesion size, location, depth, and stability of the cartilage flap, informing treatment decisions.
Treatment Options: Depending on lesion characteristics, treatment may include debridement and microfracture for smaller lesions, or more advanced techniques such as osteochondral autograft transfer (OATS) or autologous chondrocyte implantation (ACI) for larger lesions.
Syndesmotic Injuries: Syndesmotic (high ankle) sprains can result from external rotation or dorsiflexion injuries, often occurring in sports activities.
Diagnostic Arthroscopy: Arthroscopy allows direct visualization of the syndesmotic ligaments and assessment of diastasis (separation) of the tibia and fibula, which can be difficult to evaluate accurately with imaging alone.
Stabilization: In cases of significant syndesmotic instability, arthroscopic or arthroscopically assisted stabilization can be performed, typically using syndesmotic screws or tightrope constructs.
Loose Bodies: Traumatic ankle injuries can result in osteochondral loose bodies that cause mechanical symptoms and joint damage.
Identification and Removal: Arthroscopy allows for thorough identification and removal of loose bodies from all recesses of the ankle joint, including areas that may be difficult to access with open techniques.
Wrist Trauma
Wrist arthroscopy is particularly valuable for evaluating and treating traumatic wrist injuries:
Triangular Fibrocartilage Complex (TFCC) Tears: TFCC tears often result from falls onto an outstretched hand or forceful rotation injuries.
Classification and Treatment: TFCC tears are classified based on location and pattern of injury. Peripheral tears (Palmer Class 1B) are typically repairable, while central tears (Palmer Class 1A) are typically debrided.
Repair Techniques: Arthroscopic repair of peripheral TFCC tears can be performed using inside-out or outside-in techniques, with attention to protecting the ulnar nerve and neurovascular structures.
Scapholunate Ligament Injuries: Scapholunate ligament injuries can result from falls onto an outstretched hand or forceful dorsiflexion injuries.
Diagnostic Evaluation: Arthroscopy provides the most accurate assessment of scapholunate ligament integrity and dynamic instability, which can be difficult to evaluate with imaging alone.
Treatment Options: Treatment varies from debridement for partial tears to pinning or ligament reconstruction for complete tears with significant instability.
Intra-articular Fractures: Certain intra-articular fractures of the distal radius or carpal bones can be addressed with arthroscopic assistance.
Reduction and Fixation: Arthroscopic guidance can assist with fracture reduction and placement of fixation, allowing for direct visualization of the articular surface and assessment of associated soft tissue injuries.
Hip Trauma
Hip arthroscopy has expanded the treatment options for several traumatic hip conditions:
Labral Tears: Traumatic labral tears can result from injuries such as falls, motor vehicle accidents, or sports-related trauma.
Diagnostic Evaluation: Arthroscopy allows detailed evaluation of labral tears, including size, location, and pattern, as well as assessment of associated conditions such as femoroacetabular impingement (FAI).
Repair Techniques: Arthroscopic labral repair typically involves refixation of the labrum to the acetabular rim using suture anchors. In cases of irreparable labral tissue, reconstruction or reconstruction techniques may be employed.
Ligamentum Teres Injuries: The ligamentum teres can be injured in traumatic hip dislocations or subluxations.
Diagnostic Evaluation: Arthroscopy provides the most accurate assessment of ligamentum teres integrity, with partial tears, complete tears, and avulsions being the most common patterns.
Treatment Options: Treatment varies from debridement for partial tears to reconstruction for complete tears in symptomatic patients.
Femoroacetabular Impingement (FAI): While often considered a developmental condition, FAI can become symptomatic following traumatic injuries that cause cam or pincer lesions to impact against the acetabular rim.
Diagnostic Evaluation: Arthroscopy allows detailed evaluation of cam lesions (femoral head-neck junction abnormalities) and pincer lesions (acetabular overcoverage), as well as assessment of resulting labral and chondral damage.
Treatment Options: Arthroscopic treatment typically involves reshaping of the femoral head-neck junction (cam resection) and/or acetabular rim (pincer resection), with concurrent labral repair or reconstruction as needed.
Elbow Trauma
Elbow arthroscopy can be valuable in the management of certain traumatic elbow conditions:
Loose Bodies: Traumatic elbow injuries can result in osteochondral loose bodies that cause mechanical symptoms and joint damage.
Identification and Removal: Arthroscopy allows for thorough identification and removal of loose bodies from all compartments of the elbow joint, including the anterior, posterior, and radiocapitellar compartments.
Osteochondral Lesions: Osteochondral lesions of the capitellum or radial head can result from traumatic injuries.
Diagnostic Evaluation: Arthroscopy provides the most accurate assessment of lesion size, location, depth, and stability, informing treatment decisions.
Treatment Options: Depending on lesion characteristics, treatment may include debridement and microfracture for smaller lesions or more advanced techniques for larger lesions.
Capsular Release: Post-traumatic elbow stiffness can result in significant functional limitation.
Arthroscopic Release: Arthroscopic capsular release can be performed to address post-traumatic contractures, with release of the anterior and/or posterior capsule as indicated. This technique allows for precise release while protecting neurovascular structures.
The arthroscopic management of traumatic joint conditions continues to evolve, with advances in technology, instrumentation, and surgical techniques expanding the indications for minimally invasive approaches. These developments have improved outcomes for patients with traumatic joint injuries, offering the benefits of reduced surgical trauma, faster recovery, and improved functional results.
Rehabilitation and Recovery After Arthroscopic Trauma Surgery
Successful outcomes after arthroscopic trauma surgery depend not only on the technical success of the procedure but also on appropriate rehabilitation and recovery protocols. This section explores the principles and practices of rehabilitation following arthroscopic management of traumatic joint injuries, with specific considerations for different joints and injury types.
General Principles of Rehabilitation
Several fundamental principles guide rehabilitation after arthroscopic trauma surgery:
Progressive Loading: Rehabilitation follows a progressive approach, gradually increasing loads on healing tissues to stimulate appropriate healing responses without causing damage. This progression must be tailored to the specific tissue type, injury pattern, and surgical procedure.
Tissue Healing Times: Different tissues heal at different rates, and rehabilitation protocols must respect these biological timelines. For example, ligament and tendon healing typically progresses through inflammatory, proliferative, and remodeling phases, each with specific rehabilitation considerations.
Patient-Specific Factors: Rehabilitation must be individualized based on patient factors such as age, general health, pre-injury activity level, comorbidities, and specific goals. A professional athlete’s rehabilitation will differ significantly from that of a sedentary older adult.
Pain and Inflammation Management: Appropriate management of pain and inflammation is essential for facilitating participation in rehabilitation exercises. This may include modalities such as ice, compression, elevation, and judicious use of medications.
Neuromuscular Control: Restoration of neuromuscular control is a critical component of rehabilitation, particularly after traumatic injuries that disrupt normal movement patterns. This includes proprioception, balance, and coordinated muscle activation.
Knee Rehabilitation Protocols
Rehabilitation after arthroscopic knee surgery for traumatic injuries follows specific protocols based on the procedure performed:
ACL Reconstruction: ACL rehabilitation has evolved significantly, with modern protocols emphasizing early motion and weight-bearing:
Phase I (0-2 weeks): Focus on controlling swelling and pain, achieving full knee extension, and activating quadriceps. Early weight-bearing as tolerated is now commonly encouraged, with bracing for support.
Phase II (2-6 weeks): Progression of range of motion and strengthening exercises, with emphasis on closed kinetic chain exercises that protect the healing graft. Proprioception and balance exercises are introduced.
Phase III (6-12 weeks): Continued strengthening with progression to open kinetic chain exercises, advanced proprioception training, and initiation of sport-specific movements.
Phase IV (3-6 months): Sport-specific training with gradual return to running, cutting, and jumping activities. Criteria-based progression rather than time-based progression is emphasized.
Phase V (6+ months): Return to full sport participation, typically requiring demonstration of adequate strength, stability, and functional performance through objective testing.
Meniscal Repair: Rehabilitation after meniscal repair is more conservative than after meniscectomy due to the need to protect the repair:
Weight-Bearing Restrictions: Depending on tear location and repair technique, weight-bearing may be restricted for 4-6 weeks to protect the repair.
Range of Motion Limitations: Flexion may be limited to 90 degrees for the first 4-6 weeks to reduce stress on the repair site.
Gradual Progression: Return to activities is typically slower than after ACL reconstruction, with a focus on protecting the meniscus during the healing phase.
Patellar Instability: Rehabilitation after patellar stabilization procedures focuses on restoring normal patellar tracking and quadriceps function:
Early Motion: Emphasis on achieving full extension and progressive flexion while protecting the repair.
Quadriceps Activation: Specific focus on vastus medialis obliquus (VMO) activation to restore medial patellar stabilization.
Patellar Mobility: Manual therapy techniques to maintain patellar mobility and prevent adhesions.
Functional Progression: Gradual return to activities with attention to avoiding positions that risk redislocation.
Shoulder Rehabilitation Protocols
Shoulder rehabilitation after arthroscopic trauma surgery varies based on the specific procedure:
Instability Repair (Bankart Repair): Rehabilitation after instability surgery follows a structured progression to protect the repair while restoring function:
Phase I (0-6 weeks): Immobilization in a sling, with passive range of motion exercises within protected ranges. Active motion is typically avoided to protect the repair.
Phase II (6-12 weeks): Progressive active-assisted and active range of motion exercises, with gradual strengthening of rotator cuff and scapular stabilizers.
Phase III (12-16 weeks): Progressive strengthening with resistance exercises, emphasizing dynamic stabilization and neuromuscular control.
Phase IV (16+ weeks): Sport-specific training with gradual return to overhead activities, typically requiring 6-9 months for full return to contact sports.
Rotator Cuff Repair: Rehabilitation after rotator cuff repair is more conservative due to the tendon healing process:
Phase I (0-6 weeks): Strict immobilization, with only passive range of motion exercises within surgeon-specified limits. Active motion is avoided to protect the repair.
Phase II (6-12 weeks): Progressive active-assisted range of motion, with gentle isometric strengthening exercises. Active motion is gradually introduced as healing progresses.
Phase III (12-20 weeks): Progressive strengthening with resistance exercises, focusing on restoring balanced rotator cuff function and scapular mechanics.
Phase IV (20+ weeks): Advanced strengthening and functional training, with return to overhead activities typically requiring 6-9 months for small tears and longer for larger tears.
SLAP Repair: Rehabilitation after SLAP repair balances protection of the biceps-labral complex with restoration of motion:
Early Protection: Limitation of elbow extension and shoulder external rotation to protect the repair for the first 4-6 weeks.
Gradual Progression: Careful progression of range of motion and strengthening, with particular attention to avoiding provocative positions for the biceps-labral complex.
Sport-Specific Considerations: Return to overhead sports requires careful progression, with particular attention to throwing mechanics for throwing athletes.
Ankle Rehabilitation Protocols
Ankle rehabilitation after arthroscopic trauma surgery focuses on restoring stability and function:
Osteochondral Lesion Treatment: Rehabilitation after OLT treatment varies based on the specific procedure performed:
Microfracture: Protected weight-bearing for 4-6 weeks to allow for clot formation and mesenchymal cell ingrowth, followed by progressive weight-bearing and motion.
OATS or ACI: More protected rehabilitation with longer periods of non-weight-bearing (6-12 weeks) to protect the graft, followed by gradual progression of weight-bearing and motion.
Functional Progression: Return to impact activities is typically delayed for 6-9 months to allow for adequate cartilage healing and maturation.
Syndesmotic Stabilization: Rehabilitation after syndesmotic stabilization follows a structured protocol:
Weight-Bearing Progression: Typically non-weight-bearing for 4-6 weeks to allow for ligament healing, followed by progressive weight-bearing in a boot.
Range of Motion: Early protected range of motion, with avoidance of excessive dorsiflexion or external rotation that could stress the repair.
Functional Return: Gradual return to activities with emphasis on proprioception and stability, typically requiring 3-6 months for full return to sports.
Wrist Rehabilitation Protocols
Wrist rehabilitation after arthroscopic trauma surgery focuses on restoring motion and function:
TFCC Repair: Rehabilitation after TFCC repair is relatively conservative due to the importance of the TFCC in wrist stability:
Immobilization: Typically 4-6 weeks of immobilization in a neutral or slightly ulnar-deviated position to protect the repair.
Gradual Motion: Progressive range of motion exercises after immobilization, with avoidance of forceful supination or pronation that could stress the repair.
Strengthening: Progressive strengthening with focus on grip strength and forearm rotation, typically beginning 8-12 weeks postoperatively.
Scapholunate Ligament Treatment: Rehabilitation after scapholunate ligament treatment varies based on the specific procedure:
Debridement: Relatively accelerated rehabilitation with early motion and progressive strengthening.
Repair or Reconstruction: More protected rehabilitation with longer periods of immobilization (6-8 weeks) followed by gradual progression of motion and strengthening.
Hip Rehabilitation Protocols
Hip rehabilitation after arthroscopic trauma surgery follows specific protocols based on the procedure:
Labral Repair: Rehabilitation after labral repair balances protection of the repair with restoration of motion:
Weight-Bearing: Typically touchdown weight-bearing for 2-4 weeks, followed by progressive weight-bearing as tolerated.
Range of Motion: Protected range of motion with avoidance of extreme flexion, adduction, and internal rotation that could stress the repair.
Strengthening: Progressive strengthening with focus on hip abductors, external rotators, and core stability.
Femoroacetabular Impingement (FAI) Treatment: Rehabilitation after FAI treatment focuses on restoring normal joint mechanics:
Early Motion: Emphasis on achieving full range of motion while protecting the labrum if repaired.
Gait Training: Attention to normalizing gait patterns and addressing any compensatory mechanisms.
Sport-Specific Progression: Gradual return to activities with attention to movements that may recreate impingement.
Adjunctive Rehabilitation Modalities
Various modalities can complement traditional rehabilitation exercises:
Manual Therapy: Techniques such as joint mobilization, soft tissue mobilization, and manual stretching can help restore normal joint mechanics and tissue flexibility.
Neuromuscular Electrical Stimulation (NMES): Can be used to facilitate muscle activation, particularly in cases of significant muscle inhibition or atrophy.
Aquatic Therapy: Water-based exercises can provide early weight-bearing and resistance with reduced joint compression forces.
Blood Flow Restriction (BFR) Training: Emerging technique that allows for strength gains with lighter loads, potentially beneficial in early rehabilitation phases.
Psychological Support: Addressing fear of movement, kinesiophobia, and other psychological factors that can impact rehabilitation progress.
Return to Activity Criteria
Return to activity after arthroscopic trauma surgery should be based on objective criteria rather than arbitrary time frames:
Strength Testing: Objective measurement of strength compared to the uninjured side, typically requiring at least 85-90% symmetry for safe return to activity.
Functional Testing: Sport-specific functional tests that simulate the demands of the intended activity, with performance compared to normative data or pre-injury baseline when available.
Psychological Readiness: Assessment of confidence, fear of reinjury, and psychological readiness to return to activity.
Gradual Progression: Structured progression with gradual increase in intensity, duration, and complexity of activities, with monitoring for symptoms or functional decline.
Long-Term Considerations
Long-term outcomes after arthroscopic trauma surgery depend on several factors:
Adherence to Rehabilitation: Patient adherence to rehabilitation protocols significantly impacts outcomes, with better adherence generally associated with improved results.
Lifestyle Modifications: Activity modifications, weight management, and appropriate conditioning can help preserve joint health and prevent reinjury.
Ongoing Maintenance: Continued attention to strength, flexibility, and neuromuscular control can help maintain the benefits of surgery and prevent future problems.
Monitoring for Late Complications: Awareness of potential late complications such as arthritis, instability, or stiffness allows for early intervention if problems develop.
Rehabilitation after arthroscopic trauma surgery is a complex process that requires careful planning, individualized progression, and close monitoring. When properly executed, rehabilitation protocols can optimize outcomes and help patients return to their desired activities with restored function and minimized risk of reinjury.
Complications and Risk Management in Arthroscopic Trauma Surgery
While arthroscopic surgery offers numerous benefits over traditional open techniques, it is not without risks and potential complications. Understanding these complications and implementing strategies for risk management is essential for surgeons performing arthroscopic procedures in trauma cases. This section examines the potential complications associated with arthroscopic trauma surgery and approaches to minimize these risks.
General Complications
Several complications can occur with any arthroscopic procedure, regardless of the specific joint or indication:
Infection: Despite being minimally invasive, arthroscopic procedures carry a risk of infection, though the incidence is generally lower than with open surgery.
Superficial Infections: These typically occur at portal sites and present with localized redness, swelling, and pain. They usually respond well to oral antibiotics and local wound care.
Deep Infections: Intra-articular infections are more serious and can lead to significant joint damage if not promptly recognized and treated. They may require arthroscopic or open irrigation and debridement, along with intravenous antibiotics.
Risk Factors: Diabetes, immunosuppression, prolonged operative time, and poor sterile technique increase the risk of infection.
Prevention Strategies: Strict adherence to sterile technique, prophylactic antibiotics for certain procedures, and minimizing operative time can help reduce infection risk.
Thromboembolic Events: Deep vein thrombosis (DVT) and pulmonary embolism (PE) are potential complications of arthroscopic surgery, particularly lower extremity procedures.
Risk Factors: Prolonged tourniquet time, lower extremity trauma, history of thromboembolism, and certain genetic factors increase risk.
Prevention Strategies: Mechanical prophylaxis (compression devices), chemical prophylaxis (anticoagulants), early mobilization, and adequate hydration can help reduce thromboembolic risk.
Neurovascular Injury: The close proximity of nerves and blood vessels to joint spaces creates risk for iatrogenic injury during arthroscopic procedures.
Nerve Injuries: These can result from direct trauma during portal placement, instrument manipulation, or fluid extravasation causing compression. Common examples include peroneal nerve injury during knee arthroscopy and axillary nerve injury during shoulder arthroscopy.
Vascular Injuries: Though less common than nerve injuries, vascular injuries can occur during portal placement or instrument manipulation. Examples include popliteal artery injury during posterior knee arthroscopy and axillary artery injury during shoulder arthroscopy.
Prevention Strategies: Thorough knowledge of anatomy, careful portal placement under direct visualization when possible, and awareness of neurovascular structures during instrument manipulation can help reduce the risk of neurovascular injury.
Fluid Complications: The use of irrigation fluid during arthroscopy can lead to specific complications:
Fluid Extravasation: Leakage of fluid into surrounding soft tissues can cause swelling, compartment syndrome, or respiratory compromise in extreme cases.
Compartment Syndrome: Increased pressure within fascial compartments can compromise neurovascular function, particularly in the lower leg during knee arthroscopy or forearm during elbow or wrist arthroscopy.
Prevention Strategies: Careful control of inflow and outflow, appropriate pressure settings, limited operative time, and close monitoring during procedures can help minimize fluid-related complications.
Joint-Specific Complications
Different joints present specific risks and potential complications:
Knee Arthroscopy Complications:
Portal Site Problems: Poorly placed portals can cause damage to the infrapatellar fat pad, patellar tendon, or menisci, leading to persistent pain or limited motion.
Iatrogenic Cartilage Injury: Accidental scuffing or penetration of articular cartilage with instruments can lead to chondral damage and potential long-term consequences.
Graft-Related Complications: In ACL reconstruction, graft failure, tunnel malposition, and fixation problems can lead to recurrent instability or limited motion.
Arthrofibrosis: Excessive scar tissue formation can lead to loss of motion, particularly flexion, requiring aggressive rehabilitation or additional procedures.
Shoulder Arthroscopy Complications:
Chondrolysis: Postoperative loss of articular cartilage, particularly in the glenohumeral joint, can lead to painful arthritis. This has been associated with thermal energy use and excessive fluid pressure.
Stiffness: Loss of motion, particularly internal rotation, can occur after instability procedures or rotator cuff repair.
Instability Recurrence: Failure of Bankart repairs or capsular shifts can lead to recurrent instability, particularly in patients with underlying capsular laxity or bony deficiencies.
Ankle Arthroscopy Complications:
Nerve Injury: The superficial peroneal nerve, saphenous nerve, and sural nerve are at particular risk during portal placement.
Complex Regional Pain Syndrome (CRPS): This chronic pain condition can develop after ankle surgery, leading to significant disability.
Stiffness: Loss of ankle and subtalar motion can occur, particularly after prolonged immobilization or aggressive rehabilitation.
Wrist Arthroscopy Complications:
Extensor Tendon Injury: The extensor tendons are at risk during portal placement and instrument manipulation.
Stiffness: Loss of wrist and finger motion can occur, particularly after prolonged immobilization or inadequate rehabilitation.
Complex Regional Pain Syndrome: As with ankle arthroscopy, CRPS can develop after wrist arthroscopic procedures.
Hip Arthroscopy Complications:
Iatrogenic Chondrolabral Damage: The tight confines of the hip joint make chondrolabral damage more likely during instrument introduction and manipulation.
Traction-Related Complications: Nerve injury (particularly sciatic and pudendal nerves), skin breakdown, and pressure sores can result from excessive traction.
Fluid Extravasation: The hip joint’s deep location and surrounding musculature make fluid extravasation a significant concern, potentially leading to abdominal compartment syndrome in extreme cases.
Elbow Arthroscopy Complications:
Neurovascular Injury: The proximity of multiple nerves (radial, median, ulnar, and anterior interosseous) and vessels makes neurovascular injury a significant concern.
Portal Site Problems: Poorly placed portals can cause damage to the articular surface, collateral ligaments, or common extensor/flexor tendons.
Trauma-Specific Complications
Arthroscopic management of traumatic injuries presents additional considerations and potential complications:
Acute vs. Chronic Injuries: The timing of arthroscopic intervention after trauma can impact complication rates. Very early intervention may be complicated by swelling, hematoma, and tissue friability, while delayed intervention may allow for the development of stiffness, adhesions, or progressive joint damage.
Complex Injury Patterns: Traumatic injuries often involve multiple structures (e.g., ACL tear with meniscal tear and chondral injury), making comprehensive treatment more complex and potentially increasing complication risk.
Technical Challenges: Altered anatomy from trauma can make standard arthroscopic techniques more challenging, potentially increasing the risk of iatrogenic injury or inadequate treatment.
Risk Management Strategies
Effective risk management in arthroscopic trauma surgery involves multiple strategies:
Preoperative Planning:
Thorough Evaluation: Comprehensive preoperative assessment including imaging, physical examination, and patient factors that may influence complication risk.
Patient Selection: Appropriate patient selection based on injury characteristics, patient factors, and surgeon experience.
Informed Consent: Detailed discussion of potential risks and benefits, including alternative treatment options and realistic expectations.
Intraoperative Considerations:
Proper Positioning: Careful patient positioning to avoid neurovascular compression or pressure injuries.
Tourniquet Management: Appropriate tourniquet pressure and duration to minimize nerve injury and muscle damage.
Fluid Management: Careful control of irrigation fluid pressure and flow to minimize extravasation and compartment syndrome risk.
Instrumentation: Appropriate selection and use of instruments to minimize iatrogenic injury to joint structures.
Technical Expertise: Procedures should be performed within the surgeon’s level of experience, with consultation or assistance available for complex cases.
Postoperative Management:
Rehabilitation Protocols: Structured rehabilitation protocols tailored to the specific procedure and patient factors, with appropriate progression based on healing timelines.
Monitoring for Complications: Regular assessment for signs of infection, DVT, neurovascular compromise, or other complications.
Early Intervention: Prompt recognition and management of complications when they occur, including appropriate referrals when necessary.
Managing Specific Complications
When complications do occur, prompt recognition and appropriate management are essential:
Infection Management:
Superficial Infections: Oral antibiotics, local wound care, and close monitoring for resolution.
Deep Infections: Arthroscopic or open irrigation and debridement, with intravenous antibiotics based on culture results. May require multiple procedures and prolonged antibiotic therapy.
Neurovascular Injury Management:
Nerve Injuries: Observation for minor neurapraxias, surgical exploration for complete transections or compressive lesions. Referral to neurology or neurosurgery as indicated.
Vascular Injuries: Immediate vascular surgery consultation for suspected arterial injuries. Control of bleeding and repair of injured vessels when necessary.
Fluid Complication Management:
Fluid Extravasation: Discontinuation of procedure, monitoring of compartment pressures, and fasciotomy if compartment syndrome develops.
Compartment Syndrome: Emergent fasciotomy for established compartment syndrome, with careful monitoring and rehabilitation afterward.
Stiffness Management:
Early Stiffness: Aggressive rehabilitation, possibly with manipulation under anesthesia or arthroscopic lysis of adhesions.
Late Stiffness: More extensive surgical release may be necessary, with prolonged rehabilitation afterward.
Legal and Ethical Considerations
Complications in arthroscopic trauma surgery can have legal and ethical implications:
Informed Consent: Ensuring that patients have realistic expectations about outcomes and potential complications is essential for avoiding misunderstandings and potential legal issues.
Documentation: Thorough documentation of the informed consent process, surgical findings, and postoperative course is critical for legal protection.
Communication: Open and honest communication with patients when complications occur, including explanation of what happened, why it happened, and what steps are being taken to address the problem.
Quality Improvement: Using complications as opportunities for quality improvement, including root cause analysis and implementation of changes to prevent similar problems in the future.
By understanding the potential complications associated with arthroscopic trauma surgery and implementing strategies for risk management, surgeons can minimize risks and optimize outcomes for their patients. This requires ongoing education, attention to detail, and a commitment to continuous quality improvement in surgical practice.
Future Directions and Emerging Technologies in Arthroscopic Trauma Surgery
The field of arthroscopic trauma surgery continues to evolve rapidly, driven by technological advances, improved understanding of joint pathology and healing, and innovative surgical techniques. This section explores emerging technologies and future directions that are likely to shape the practice of arthroscopic trauma surgery in the coming years.
Advanced Imaging and Navigation
Imaging and navigation technologies are enhancing the precision and outcomes of arthroscopic procedures:
Three-Dimensional (3D) Arthroscopy: Traditional arthroscopy provides two-dimensional visualization, requiring surgeons to mentally reconstruct three-dimensional anatomy. 3D arthroscopic systems are being developed that provide stereoscopic visualization, improving depth perception and spatial orientation during complex procedures.
Benefits: Improved depth perception can enhance the precision of surgical tasks such as suture placement, anchor positioning, and tissue debridement.
Current Limitations: Early 3D systems have been limited by bulky equipment, reduced image quality compared to standard HD systems, and surgeon adaptation to the new visualization method.
Future Developments: Next-generation 3D systems are likely to feature improved image quality, more ergonomic designs, and better integration with other surgical technologies.
Augmented Reality (AR) Integration: AR technology overlays digital information onto the surgeon’s view of the surgical field, potentially enhancing arthroscopic procedures:
Applications: AR could overlay preoperative imaging data, anatomical landmarks, or surgical plans onto the arthroscopic view, providing real-time guidance during procedures.
Current Status: Early AR applications in arthroscopy are being developed and tested, with promising results in preclinical and early clinical studies.
Challenges: Integration of AR into the surgical workflow, ensuring accuracy of overlay information, and avoiding visual distraction are ongoing challenges.
Computer-Assisted Navigation: Navigation systems that track instrument position relative to patient anatomy are becoming more common in orthopedic surgery:
Current Applications: Navigation has been primarily used in joint replacement surgery but is being adapted for arthroscopic procedures, particularly for precise tunnel placement in ligament reconstruction.
Arthroscopic Applications: Potential uses include guidance for fracture reduction, tunnel positioning in ligament reconstruction, and placement of implants for fracture fixation.
Benefits: Improved accuracy of surgical tasks, reduced radiation exposure compared to fluoroscopic guidance, and enhanced ability to reproduce anatomical landmarks.
Future Directions: Miniaturization of tracking systems, improved integration with arthroscopic equipment, and development of arthroscopy-specific navigation software are likely future developments.
Robotic and Assisted Surgery
Robotic technology is beginning to influence arthroscopic surgery, though applications in trauma are still emerging:
Robotic-Assisted Arthroscopy: Robotic systems designed specifically for arthroscopic surgery are in development:
Current Status: Several companies are developing robotic systems for arthroscopic procedures, with some in early clinical trials.
Potential Applications: Robotic assistance could enhance precision in tasks such as meniscal repair, ligament reconstruction, and cartilage procedures.
Benefits: Improved precision, reduced surgeon fatigue, enhanced visualization, and the ability to perform tasks beyond human dexterity limits.
Challenges: High cost, steep learning curve, limited adaptability to unexpected findings, and the need for specialized training are current limitations.
Haptic Feedback Systems: Advanced robotic systems with haptic feedback allow surgeons to feel tissue resistance during robotic procedures:
Applications: Haptic feedback could enhance the surgeon’s ability to differentiate tissue types, apply appropriate forces during tissue manipulation, and avoid excessive pressure on delicate structures.
Current Status: Haptic technology is well-established in industrial robotics but is still being adapted for surgical applications, including arthroscopy.
Future Potential: Integration of haptic feedback with robotic-assisted arthroscopy could enhance the surgeon’s ability to perform delicate tasks with appropriate force application.
Surgical Robotics for Training: Robotic systems are being developed for surgical training and simulation:
Applications: Training systems that provide realistic haptic feedback and performance metrics could enhance arthroscopic skills acquisition.
Benefits: Safe environment for learning complex procedures, objective assessment of surgical skills, and ability to practice rare or complex cases.
Current Status: Several arthroscopic training simulators are available, with increasing sophistication in haptic feedback and procedural realism.
Advanced Instrumentation and Implants
Innovations in arthroscopic instrumentation and implants are expanding the capabilities of minimally invasive trauma surgery:
Smart Instruments: Instruments with integrated sensors and feedback mechanisms are being developed:
Applications: Smart instruments could provide real-time feedback on forces applied during tissue manipulation, suture tension, or instrument position relative to critical structures.
Examples: Force-sensing shavers, smart suture anchors that provide feedback on fixation strength, and instruments with integrated navigation tracking.
Current Status: Early prototypes of smart instruments are being tested, with some already in limited clinical use.
Bioabsorbable and Biocompatible Implants: Advances in materials science are leading to improved implants for arthroscopic trauma surgery:
Bioabsorbable Implants: Suture anchors, interference screws, and fixation devices made from materials that gradually absorb and are replaced by native tissue are becoming more common.
Benefits: Reduced long-term foreign body reaction, elimination of need for hardware removal, and potential for improved tissue integration.
Future Directions: Development of bioabsorbable materials with optimized strength profiles, degradation rates, and biocompatibility.
3D-Printed Custom Implants: Additive manufacturing technology allows for creation of patient-specific implants:
Applications: Custom implants for complex fracture fixation, osteochondral defects, or ligament reconstruction based on patient-specific anatomy.
Benefits: Improved anatomical fit, potentially better biomechanical properties, and ability to address complex or unusual pathology.
Current Status: 3D-printed implants are being used in some orthopedic applications, with arthroscopic applications in development.
Nanotechnology in Implants and Coatings: Nanoscale modifications to implants and instruments are being explored:
Applications: Antibacterial coatings for implants to reduce infection risk, surface modifications to enhance tissue integration, and drug-eluting implants for localized therapeutic delivery.
Benefits: Reduced infection rates, improved healing, and potential for targeted therapy delivery.
Current Status: Several nanotechnology-enhanced implants are in clinical use or testing, with ongoing research into new applications.
Biologics and Regenerative Medicine
Biologic therapies and regenerative medicine approaches are transforming the treatment of traumatic joint injuries:
Platelet-Rich Plasma (PRP) and Autologous Conditioned Serum: Concentrated preparations of autologous growth factors are being used to enhance healing:
Applications: PRP is being used as an adjunct to various arthroscopic procedures, including rotator cuff repair, ACL reconstruction, and treatment of tendinopathies.
Evidence: Clinical evidence for PRP efficacy is mixed, with some studies showing benefits in specific applications while others show no significant difference compared to controls.
Future Directions: Standardization of preparation protocols, better understanding of optimal formulations for specific conditions, and identification of patients most likely to benefit.
Mesenchymal Stem Cells (MSCs): Stem cell therapies are being investigated for their potential to enhance tissue healing:
Applications: MSCs are being studied for treatment of cartilage defects, ligament and tendon healing, and osteoarthritis.
Delivery Methods: Various delivery methods are being explored, including direct injection, scaffold-based delivery, and combination with growth factors.
Current Status: Early clinical studies show promise, but larger, well-controlled trials are needed to establish efficacy and optimal protocols.
Gene Therapy: Genetic approaches to enhance tissue healing are in development:
Applications: Gene therapy could be used to deliver growth factors or other healing-promoting factors directly to injured tissues.
Methods: Viral vectors, non-viral delivery systems, and ex vivo gene therapy approaches are being investigated.
Current Status: Primarily in preclinical development, with some early clinical trials showing promise for specific applications.
Tissue Engineering: Combination of scaffolds, cells, and bioactive factors to create functional tissue replacements:
Applications: Engineered cartilage, ligament, and meniscus tissue could provide alternatives to traditional repair techniques.
Progress: Significant advances have been made in tissue engineering, but challenges remain in creating tissue with appropriate mechanical properties and integration with native tissue.
Future Outlook: Tissue engineering approaches are likely to become more clinically relevant in the coming decades, potentially revolutionizing the treatment of traumatic joint injuries.
Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning (ML) technologies are beginning to influence arthroscopic practice:
Diagnostic Assistance: AI systems are being developed to assist with diagnosis based on imaging and clinical data:
Applications: AI algorithms can analyze medical images to detect and classify pathology, potentially improving diagnostic accuracy and efficiency.
Current Status: Several AI systems have demonstrated diagnostic accuracy comparable to or exceeding that of human experts for specific conditions, though widespread clinical implementation is still limited.
Future Potential: Integration of AI with arthroscopic imaging could provide real-time diagnostic assistance during procedures.
Surgical Planning and Guidance: AI systems can help optimize surgical planning and provide intraoperative guidance:
Applications: Preoperative planning based on patient-specific anatomy and pathology, intraoperative guidance for instrument placement, and real-time feedback on surgical tasks.
Current Status: Early AI-assisted planning systems are in development and testing, with some already in limited clinical use.
Benefits: Improved surgical precision, reduced variability in surgical technique, and potential for better outcomes.
Outcome Prediction: Machine learning algorithms can analyze patient data to predict outcomes and guide treatment decisions:
Applications: Predicting which patients are likely to benefit from specific interventions, identifying risk factors for complications, and personalizing rehabilitation protocols.
Current Status: Outcome prediction models are being developed and validated, with some showing promising results in early studies.
Future Directions: Integration of outcome prediction with electronic health records and clinical decision support systems could enhance personalized treatment approaches.
Training and Education Innovations
Advances in technology are transforming how surgeons learn and maintain arthroscopic skills:
Virtual Reality (VR) and Simulation: High-fidelity simulators are becoming more sophisticated and widely available:
Applications: Training for basic arthroscopic skills, practice of specific procedures, and simulation of rare or complex cases.
Benefits: Safe environment for learning, objective assessment of skills, ability to practice without time constraints, and reduced need for cadaveric specimens.
Current Status: VR simulators are increasingly used in residency training and continuing education, with growing evidence for their effectiveness in skills acquisition.
Augmented Reality (AR) Training: AR technology is being applied to surgical education:
Applications: Overlaying instructional information onto the surgical field, providing real-time guidance during training procedures, and enhancing anatomical understanding.
Current Status: Early AR training systems are in development and testing, with promising initial results.
Future Potential: AR could transform surgical education by providing personalized, real-time guidance during learning procedures.
Remote Mentoring and Telementoring: Technology-enabled remote guidance is expanding surgical education:
Applications: Expert surgeons can provide real-time guidance to less experienced surgeons during procedures, regardless of geographic location.
Technology Requirements: High-quality video transmission, stable internet connectivity, and specialized software platforms are needed for effective telementoring.
Current Status: Telementoring has been successfully used in various surgical specialties, including orthopedics, with growing interest in arthroscopic applications.
Challenges and Considerations for Implementation
While these emerging technologies offer exciting possibilities, several challenges must be addressed for successful implementation:
Cost and Accessibility: Many advanced technologies are expensive, potentially limiting access to well-funded institutions or creating disparities in care:
Cost-Benefit Analysis: Careful evaluation of the added value of new technologies relative to their cost is essential.
Reimbursement Considerations: Development of appropriate reimbursement models for new technologies is needed to ensure sustainability.
Training and Education: Implementing new technologies requires significant investment in training and education:
Learning Curves: Surgeons and operating room staff must develop proficiency with new technologies, which can be time-consuming.
Resistance to Change: Overcoming resistance to adoption of new techniques and technologies requires effective change management strategies.
Evidence-Based Implementation: New technologies should be implemented based on evidence of improved outcomes rather than novelty alone:
Clinical Trials: Rigorous evaluation of new technologies through well-designed clinical trials is essential.
Regulatory Approval: Appropriate regulatory oversight ensures safety and efficacy before widespread adoption.
Ethical Considerations: The implementation of new technologies raises several ethical questions:
Equity and Access: Ensuring equitable access to beneficial technologies across different patient populations and healthcare settings.
Privacy and Data Security: Protecting patient data collected by advanced technologies and AI systems.
The future of arthroscopic trauma surgery is likely to be shaped by these emerging technologies, offering the potential for improved precision, better outcomes, and expanded treatment options for patients with traumatic joint injuries. However, realizing this potential will require careful implementation, ongoing evaluation, and a commitment to evidence-based practice.
Frequently Asked Questions
- What is arthroscopic surgery?
Arthroscopic surgery is a minimally invasive surgical technique that allows orthopedic surgeons to visualize, diagnose, and treat problems inside a joint using a small camera called an arthroscope and specialized instruments inserted through small incisions called portals. This approach results in less tissue damage, reduced pain, and faster recovery compared to traditional open surgery.
- How is arthroscopy used in trauma cases?
In trauma cases, arthroscopy is used to diagnose and treat various joint injuries resulting from accidents, falls, sports injuries, and other traumatic events. It allows surgeons to directly visualize the extent of injury, remove loose bodies, repair torn ligaments or tendons, treat cartilage damage, and sometimes assist in fracture fixation, all through minimally invasive techniques.
- Which joints can be treated arthroscopically after trauma?
Arthroscopic techniques can be applied to most joints in the body, including the knee, shoulder, ankle, wrist, hip, elbow, and even smaller joints like the temporomandibular joint. The knee and shoulder are the most commonly treated joints arthroscopically, particularly for traumatic injuries.
- What are the benefits of arthroscopic surgery for trauma patients?
Arthroscopic surgery offers several benefits for trauma patients, including smaller incisions, less postoperative pain, reduced risk of infection, shorter hospital stays, faster recovery times, and better cosmetic results. The minimally invasive approach also allows for earlier rehabilitation and potentially improved functional outcomes.
- How long does recovery take after arthroscopic trauma surgery?
Recovery time varies depending on the specific joint, type of injury, and procedure performed. Simple arthroscopic procedures like loose body removal may allow return to normal activities within a few weeks, while more complex procedures like ligament reconstruction may require 6-12 months for full recovery. Your surgeon will provide a specific timeline based on your individual case.
- Is arthroscopic surgery safe for traumatic injuries?
Arthroscopic surgery is generally safe when performed by experienced surgeons. Like any surgical procedure, it carries risks such as infection, blood clots, nerve or blood vessel damage, and complications related to anesthesia. However, the minimally invasive nature of arthroscopy typically results in fewer complications than open surgery.
- Can all traumatic joint injuries be treated arthroscopically?
While arthroscopic techniques have expanded significantly, not all traumatic joint injuries can be treated arthroscopically. Some complex fractures, severe dislocations, or injuries requiring extensive reconstruction may still require open surgery. The decision to use arthroscopic versus open techniques depends on the specific injury pattern, patient factors, and surgeon expertise.
- What types of knee trauma can be treated arthroscopically?
Common traumatic knee injuries treated arthroscopically include anterior cruciate ligament (ACL) tears, meniscal tears, patellar dislocations, loose bodies, cartilage injuries, and certain types of fractures. Arthroscopy allows for precise diagnosis and treatment of these conditions with minimal tissue damage.
- How is arthroscopy used for shoulder trauma?
Arthroscopy is commonly used for traumatic shoulder conditions including rotator cuff tears, shoulder instability (Bankart lesions), labral tears (SLAP lesions), AC joint separations, and certain types of fractures. The arthroscopic approach allows for detailed evaluation and treatment of these injuries with less postoperative pain and stiffness.
- Can ankle injuries be treated arthroscopically?
Yes, many traumatic ankle injuries can be treated arthroscopically, including osteochondral lesions of the talus, ankle impingement, loose bodies, syndesmotic injuries, and certain types of fractures. Ankle arthroscopy allows for precise treatment with less damage to surrounding soft tissues compared to open surgery.
- What is the recovery like after arthroscopic ACL reconstruction?
Recovery after arthroscopic ACL reconstruction typically involves several phases: initial protection and motion (0-2 weeks), progressive strengthening (2-6 weeks), advanced strengthening and neuromuscular training (6-12 weeks), sport-specific training (3-6 months), and return to full activity (6-9 months). Modern protocols emphasize early motion and weight-bearing when appropriate.
- Are there age restrictions for arthroscopic trauma surgery?
There are no absolute age restrictions for arthroscopic trauma surgery. The decision to proceed with surgery depends on the patient’s overall health, functional demands, specific injury, and expected benefits rather than age alone. Both young athletes and older adults can undergo arthroscopic procedures when indicated.
- How soon after a traumatic injury can arthroscopic surgery be performed?
The timing of arthroscopic surgery after trauma depends on the specific injury, swelling, and patient factors. Some acute injuries like ACL tears may be treated after initial swelling subsides (1-3 weeks), while other conditions like fractures or locked knees may require more urgent intervention. Your surgeon will determine the optimal timing based on your individual case.
- What are the risks of arthroscopic trauma surgery?
Risks of arthroscopic trauma surgery include infection, blood clots, nerve or blood vessel injury, stiffness, persistent pain, instrument breakage, fluid extravasation, and risks related to anesthesia. While serious complications are rare, it’s important to discuss potential risks with your surgeon before proceeding with surgery.
- How should I prepare for arthroscopic trauma surgery?
Preparation for arthroscopic trauma surgery typically includes preoperative medical evaluation, medication adjustments (especially blood thinners), fasting before surgery, arranging for transportation home, and preparing your home for recovery. Your surgeon will provide specific instructions based on your procedure and medical history.
- Will I need physical therapy after arthroscopic trauma surgery?
Most patients will need some form of rehabilitation after arthroscopic trauma surgery, ranging from simple home exercises to formal physical therapy. The intensity and duration of rehabilitation depend on the specific procedure performed, with more complex surgeries like ligament reconstruction requiring more extensive therapy.
- Can arthroscopic surgery be performed on patients with previous joint surgeries?
Yes, arthroscopic surgery can often be performed on patients with previous joint surgeries, though it may be more technically challenging due to scar tissue and altered anatomy. Your surgeon will evaluate your specific situation to determine if arthroscopic surgery is appropriate.
- What type of anesthesia is used for arthroscopic trauma surgery?
Arthroscopic trauma surgery can be performed under general anesthesia (completely asleep), regional anesthesia (spinal or epidural), or local anesthesia with sedation, depending on the specific joint, procedure, patient factors, and surgeon preference. Your anesthesiologist will discuss the best option for your case.
- How long does arthroscopic trauma surgery typically take?
The duration of arthroscopic trauma surgery varies depending on the complexity of the procedure. Simple diagnostic arthroscopy or procedures like loose body removal may take 30-60 minutes, while more complex procedures like ligament reconstruction or fracture fixation may take 2-3 hours or longer.
- What are the signs of complications after arthroscopic trauma surgery?
Signs of potential complications after arthroscopic surgery include fever, increasing pain, swelling, redness or drainage from incisions, numbness or tingling, inability to move the joint, calf pain or swelling (which could indicate a blood clot), and difficulty breathing. Contact your surgeon if you experience any concerning symptoms.
- Can I drive after arthroscopic trauma surgery?
The ability to drive after arthroscopic surgery depends on the joint involved, type of procedure, pain control, and any restrictions on weight-bearing or motion. Generally, patients should not drive while taking pain medications or until they can safely control the vehicle, which may take several days to weeks depending on the procedure.
- When can I return to work after arthroscopic trauma surgery?
Return to work after arthroscopic trauma surgery depends on the type of work you do and the procedure performed. Desk jobs may allow return within a few days to a week, while physically demanding jobs may require 6-12 weeks or longer. Your surgeon will provide specific guidance based on your individual case.
- Can arthroscopic surgery be performed on children with traumatic injuries?
Yes, arthroscopic surgery can be performed on children with traumatic injuries, though special considerations apply regarding anatomy, growth plates, and rehabilitation. Pediatric orthopedic surgeons with experience in arthroscopic techniques typically perform these procedures.
- How successful is arthroscopic surgery for traumatic injuries?
Success rates for arthroscopic surgery vary depending on the specific injury and procedure performed. Many common arthroscopic procedures like ACL reconstruction and meniscal repair have success rates of 85-95% in terms of patient satisfaction and return to activities. Your surgeon can provide more specific success rates for your particular condition.
- What new technologies are being developed for arthroscopic trauma surgery?
Emerging technologies in arthroscopic trauma surgery include 3D arthroscopy, augmented reality navigation, robotic-assisted surgery, advanced imaging techniques, smart instruments with integrated sensors, biologic therapies to enhance healing, and artificial intelligence for surgical planning and assistance. These technologies aim to improve precision, outcomes, and patient recovery.
- How do I choose a surgeon for arthroscopic trauma surgery?
When choosing a surgeon for arthroscopic trauma surgery, consider factors such as board certification in orthopedic surgery, fellowship training in sports medicine or arthroscopy, experience with your specific injury, surgical volume, hospital affiliations, and communication style. Don’t hesitate to ask about the surgeon’s experience and outcomes with your specific procedure.
- Will I have scars after arthroscopic trauma surgery?
Arthroscopic surgery typically results in small scars (usually 0.5-1 cm in length) at the portal sites where instruments were inserted. These scars are usually much smaller and less noticeable than those from open surgery. Over time, these scars typically fade and become less visible.
- Can arthroscopic surgery be repeated if needed?
Yes, arthroscopic surgery can be repeated if necessary, such as for revision ligament reconstruction, treatment of new injuries, or management of persistent problems. However, each surgery carries risks, and the decision to perform repeat surgery should be carefully considered based on potential benefits and risks.
- How much does arthroscopic trauma surgery cost?
The cost of arthroscopic trauma surgery varies widely depending on the specific procedure, geographic location, surgeon fees, hospital or surgical center fees, anesthesia costs, and insurance coverage. Contact your insurance provider and surgeon’s office for specific cost information related to your procedure.
- What are the long-term outcomes after arthroscopic trauma surgery?
Long-term outcomes after arthroscopic trauma surgery are generally favorable for most procedures, with many patients returning to their pre-injury activity levels. However, outcomes depend on factors such as the severity of the initial injury, specific procedure performed, patient adherence to rehabilitation, and presence of pre-existing joint degeneration. Your surgeon can provide more specific information about expected long-term outcomes for your particular condition.
Medical Disclaimer:
The information provided on this website is for general educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.