Understanding Gangrene: A Comprehensive Guide to Its Types, Causes, and Treatments
When we hear the word “gangrene,” it often conjures stark and frightening images. While it is indeed a severe and potentially life-threatening condition, understanding it is the first step toward prevention and effective treatment. Gangrene is, at its core, the death of body tissue due to a lack of blood flow or a serious bacterial infection. In this article, we will delve into the complexities of this condition, exploring what it is, its various forms, the underlying causes, the critical symptoms to watch for, and the modern medical interventions used to combat it.
What Exactly is Gangrene? A Comprehensive Overview
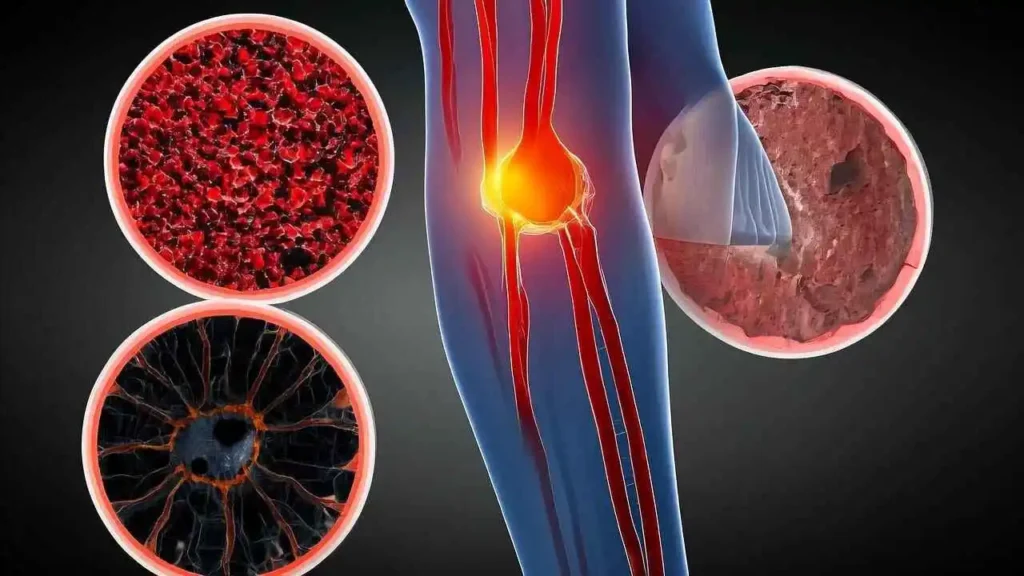
At the most fundamental level, our body is a complex network of living cells, each requiring a constant supply of oxygen and nutrients to function and survive. This vital lifeline is the circulatory system, with blood acting as the delivery service. When this vital blood supply to any part of the body is cut off or severely restricted—whether due to a traumatic injury, a persistent infection, or an underlying chronic illness—the affected tissue is starved. Without oxygen, cellular machinery grinds to a halt, and cells begin to decay and die. This process of tissue death is known as necrosis. When necrosis affects a significant, localized area of tissue, we call it gangrene.
While we most commonly associate gangrene with extremities like the toes, feet, fingers, and hands—areas furthest from the heart and most vulnerable to circulatory issues—it is a condition that can also occur deep inside the body, affecting muscles and even internal organs like the gallbladder or intestines. Recognizing its signs early is paramount, as gangrene can progress with alarming speed, leading to severe, life-threatening complications, including systemic infection (sepsis), shock, and the necessity for amputation.
The Different Types of Gangrene: A Comprehensive Overview
Gangrene, the death of body tissue due to a lack of blood flow or a severe bacterial infection, is a word that rightly evokes a sense of urgency and fear. However, it is not a single, uniform disease. Gangrene presents in several distinct forms, each with its own underlying causes, characteristic symptoms, and level of threat. Understanding these differences is crucial for recognizing the signs and appreciating the need for immediate medical intervention. Let’s explore the primary types in detail.
• Dry Gangrene
Dry gangrene is the form most commonly associated with chronic circulatory problems. It occurs when blood flow to an extremity, such as a toe, foot, or hand, is slowly and progressively impaired over a long period. This is not typically caused by a sudden injury but by underlying conditions that narrow or block arteries.
Causes and Risk Factors: The leading causes are atherosclerosis (hardening of the arteries), peripheral artery disease (PAD), and complications from diabetes, which damages both blood vessels and nerves. Smokers and individuals with severe frostbite are also at high risk.
Progression and Appearance: The process is gradual. The affected tissue, starved of oxygen and nutrients, begins to die. It first becomes cold, pale, and numb due to nerve damage. Over time, the tissue dehydrates, shrivels, and undergoes a distinct color change, moving from red to dark brown and finally to a black, leathery, and “mummified” appearance. A clear line of demarcation often forms between the dead tissue and the adjacent healthy tissue.
Infection and Threat: A key feature of dry gangrene is that it usually does not involve a bacterial infection. Because of this, it tends to progress more slowly and is less of an immediate systemic threat than other forms. However, the dead tissue is highly susceptible to secondary infection, which can transform it into the much more dangerous wet gangrene. Therefore, it still constitutes a serious condition requiring urgent medical evaluation and management.
• Wet Gangrene
In stark contrast to dry gangrene, wet gangrene is characterized by a combination of tissue death and a rampant bacterial infection. If a body part suffers an injury that suddenly cuts off blood flow—such as a severe burn, crush injury, or deep cut—and bacteria invade the vulnerable, dying tissue, wet gangrene can develop.
Mechanism: The bacteria thrive in the moist, oxygen-deprived environment of the dead tissue. They multiply rapidly, releasing potent toxins that cause the tissue to break down, liquefy, and decay in a process known as putrefaction.
Symptoms: The affected area becomes swollen, tense, and may develop blisters or weeping sores that release a foul-smelling, pus-like fluid. The skin color can range from red to brown to black, and the area is often painful. Unlike dry gangrene, there is no clear line separating it from healthy tissue, as the infection spreads aggressively.
Medical Emergency: Wet gangrene is a life-threatening medical emergency. The bacterial toxins and inflammatory byproducts can easily enter the bloodstream, leading to sepsis—a widespread, overwhelming immune response that can cause a catastrophic drop in blood pressure (septic shock), organ failure, and death.
• Gas Gangrene
Gas gangrene is a particularly dangerous and rapidly progressing subtype of wet gangrene. It is most famously caused by the bacterium Clostridium perfringens, although other species can be involved.
The Culprit and its Environment: Clostridium bacteria are anaerobes, meaning they thrive in low-oxygen environments. They are commonly found in soil and can contaminate deep, traumatic wounds where the blood supply has been compromised, such as those from car accidents, combat injuries, or certain surgeries.
Hallmark Symptoms: As these bacteria multiply, their metabolic process releases toxins and produces significant amounts of gas. This gas becomes trapped within the tissues, causing the skin to become pale and then evolve to a gray or purplish-red color. The most distinctive sign is crepitus—a crackling or bubbling sensation that can be felt and sometimes heard when the affected skin is pressed. A brownish, frothy, and foul-smelling discharge may also be present.
Urgency and Treatment: As the U.S. Centers for Disease Control and Prevention (CDC) notes, “The toxins made by Clostridium perfringens cause tissue death, which is what gangrene is. If the conditions are right, the bacteria can produce toxins very quickly.” This rapid progression can lead to widespread tissue destruction, shock, and death within hours, making gas gangrene a dire medical emergency that requires immediate and aggressive treatment, including surgery to remove all dead tissue and high-dose intravenous antibiotics.
• Internal Gangrene
While other forms of gangrene affect the skin and extremities, internal gangrene occurs when blood flow to an internal organ is blocked. This can affect organs like the intestines, gallbladder, or appendix.
Causes: Common causes include an incarcerated hernia (where a portion of the intestine becomes trapped and its blood supply is cut off), a volvulus (twisting of the intestine), or a blood clot that blocks a major artery supplying an organ (mesenteric ischemia).
Symptoms and Diagnosis: Because the condition is internal, there are no visible skin changes. Instead, symptoms often include sudden, severe pain in the affected area (usually the abdomen), fever, nausea, and vomiting. If not treated, it can quickly lead to shock, characterized by low blood pressure, rapid heart rate, and confusion. Diagnosis can be challenging and often relies on imaging tests like CT scans.
• Fournier’s Gangrene
Fournier’s gangrene is a rare but extremely severe and aggressive form of necrotizing fasciitis (flesh-eating disease) that specifically affects the perineal, genital, or perianal regions.
Pathology and Risk: It is a polymicrobial infection, meaning it’s caused by a mix of aerobic and anaerobic bacteria that work together to rapidly destroy tissue. While it can occur in anyone, it is most common in older men, particularly those with underlying conditions that compromise the immune system, such as diabetes, chronic alcoholism, or malignancy.
Progression and Treatment: The infection spreads rapidly along the fascial planes—the connective tissue layers beneath the skin—causing intense pain, swelling, and discoloration of the genital and surrounding areas. Fournier’s gangrene is a urological and surgical emergency with a high mortality rate. Treatment requires immediate and extensive surgical debridement of all necrotic tissue, alongside powerful broad-spectrum antibiotics.
Unpacking the Causes and Risk Factors of Gangrene: A Deeper Look
At its core, all gangrene is the result of a critical failure in the body’s logistics: a compromised or completely halted blood supply. Blood is the vital transport system that delivers oxygen, nutrients, and immune cells to every part of our body. When that supply is cut off, tissues are starved, suffocate, and begin to die—a process known as necrosis. This tissue death is what we call gangrene.
While the fundamental cause is simple, numerous conditions and factors can create the perilous environment for this to happen. Understanding these pathways is crucial, as awareness is the first step toward prevention and timely intervention.
Major Causes: The Direct Triggers of Tissue Death
Three primary events can directly initiate the process of gangrene:
1. Lack of Blood Supply (Ischemia) This is the most common pathway to “dry gangrene.” When blood vessels become narrowed or blocked over time, blood flow slows to a trickle and may eventually stop. The affected tissue, most often in the extremities like toes, feet, and fingers, slowly dries up, shrivels, and darkens in color. Key conditions responsible for this include:
Atherosclerosis: Often called “hardening of the arteries,” this is a process where fatty deposits, cholesterol, and other substances build up into plaques on the inner walls of arteries. These plaques narrow the channel for blood flow.
Peripheral Artery Disease (PAD): This is a specific manifestation of atherosclerosis where the plaques build up in the arteries that supply blood to the limbs. It is a leading cause of gangrene in the legs and feet.
Blood Clots (Thrombosis or Embolism): A blood clot can form directly within a vessel (thrombosis) or travel from another part of the body and get lodged in a smaller artery (embolism), causing an abrupt and complete blockage of blood flow.
2. Overwhelming Infection When bacteria invade tissue, especially through a wound, they can multiply rapidly. If blood flow is already poor, the body’s immune system cannot deliver enough white blood cells to fight the invasion. The bacteria then release toxins that destroy tissue directly and cause massive inflammation, which further chokes off the blood supply. This leads to “wet gangrene,” characterized by swelling, blisters, pus, and a foul odor. If the infection is caused by gas-producing bacteria like Clostridium, it can result in “gas gangrene,” a particularly aggressive form where gas builds up in the tissue, leading to rapid spread and extreme toxicity.
3. Severe Trauma Sudden, severe physical injury can cause immediate and extensive damage to blood vessels, cutting off circulation instantly. The tissue death that follows is often swift. Examples include:
Crush Injuries: The sheer force of a heavy object can physically obliterate blood vessels.
Serious Burns or Frostbite: Extreme temperatures can destroy skin, underlying tissue, and the blood vessels within them.
Deep, Lacerating Wounds: A cut that severs a major artery will immediately deprive the downstream tissue of its blood supply.
Key Risk Factors: The Conditions That Set the Stage
While the causes above are the direct triggers, certain chronic conditions and lifestyle factors dramatically increase a person’s vulnerability.
Diabetes: This is arguably the single most significant risk factor for gangrene. Diabetes creates a dangerous triad of problems:
Vascular Damage: Persistently high blood sugar levels damage the lining of blood vessels, accelerating atherosclerosis and impairing circulation, especially in the small vessels of the feet and hands.
Nerve Damage (Neuropathy): High blood sugar also damages peripheral nerves, leading to a loss of sensation. A person with diabetic neuropathy might not feel a small cut, blister, or pressure sore on their foot.
Weakened Immune Response: Diabetes can impair the function of immune cells, making the body less effective at fighting off infections. This combination means a small, unfelt injury can easily become infected, and with poor circulation preventing a proper immune response, the infection can rapidly escalate into gangrene.
Smoking and Tobacco Use: The chemicals in tobacco are profoundly damaging to the vascular system. Nicotine is a potent vasoconstrictor, meaning it tightens blood vessels and restricts blood flow. Furthermore, smoking promotes the development of atherosclerosis and thickens the blood, making it harder to circulate. This chronic reduction in blood flow makes smokers highly susceptible to PAD and subsequent gangrene.
Obesity: Carrying significant excess weight places immense strain on the entire cardiovascular system. It is a major contributor to high blood pressure, high cholesterol, and Type 2 diabetes—all of which are independent risk factors for the vascular diseases that cause gangrene.
Weakened Immune System (Immunosuppression): When the body’s defense mechanisms are weak, it cannot effectively combat bacterial invasions. Any condition or treatment that suppresses the immune system—such as HIV/AIDS, chemotherapy, radiation therapy, or long-term steroid use—leaves a person vulnerable. A minor skin infection that a healthy individual would easily fight off can spiral out of control and lead to wet gangrene.
Recent Surgery or Injury: Any event that creates a wound site is a potential entry point for infection. The post-operative or post-injury swelling can also temporarily compress blood vessels, reducing circulation to the area and creating an ideal environment for gangrene to develop if an infection takes hold.
Raynaud’s Phenomenon: This condition causes brief episodes of vasospasm, where the small blood vessels in the fingers and toes narrow dramatically, usually in response to cold or stress. While these episodes are typically temporary, severe and frequent attacks can, over time, cause permanent damage to the arterial walls, leading to chronic circulatory problems and an increased risk of tissue death.
Recognizing the Symptoms of Gangrene: A Critical Guide on When to Seek Immediate Help
Gangrene is a medical emergency where body tissue dies, either due to a lack of blood flow or a severe bacterial infection. The absolute most critical factor in successfully treating this condition and preventing devastating outcomes—such as limb amputation or even death—is early detection. The progression can be frighteningly rapid, so recognizing the initial signs is paramount.
If you or someone you know exhibits any of the following symptoms, especially if they have underlying risk factors like diabetes, peripheral artery disease, a recent surgery, or a traumatic injury, you must seek immediate medical attention. Do not “wait and see” if it gets better.
Key Symptoms to Watch For:
1. Dramatic Skin Discoloration One of the most telling signs of gangrene is a visible and often rapid change in skin color. This isn’t just a simple rash; it’s a chilling spectrum that signals advancing tissue death.
Initial Stage: The affected area may first appear unusually pale or develop a bluish, waxy tint, a sign that oxygenated blood is not reaching the tissue.
Progression: As the condition worsens, the color deepens, moving through shades of red or bronze before turning a dark purple or mottled color.
Final Stage: The final stage is the most alarming: the skin turns black. This indicates that the tissue is necrotic, or completely dead.
2. Pain That Progresses to Numbness The pain associated with gangrene can be deceptive.
Sudden, Severe Pain: Initially, there might be an onset of sudden and excruciating pain in the affected area as the tissue is starved of oxygen.
The Disappearance of Pain: Paradoxically, this intense pain may later subside and be replaced by a complete loss of sensation. This is not a sign of improvement. It is a treacherous red flag indicating that the local nerves have died, severing communication with the brain. This numbness can give a false sense of security while the tissue destruction silently continues.
3. Persistent Numbness or a “Pins and Needles” Sensation Even before the complete loss of sensation, you may experience a persistent feeling of numbness or a tingling “pins and needles” sensation (paresthesia) in the limb or digit. This is an early warning that circulation and nerve function are severely compromised.
4. A Palpable Coldness Because gangrene is fundamentally a problem of blood flow, the affected area will lose its warmth. The limb, finger, or toe will feel significantly colder to the touch than the rest of the body. You can often feel a distinct line or demarcation where the cold, compromised tissue begins.
5. Swelling, Blisters, and Gas in the Tissues These signs are particularly common in “wet gangrene,” which involves a bacterial infection.
Swelling and Blisters: The skin may become swollen, and blisters (bullae) may form. These blisters are often filled with a dark, foul-smelling fluid.
Crepitus: In a specific type called gas gangrene, a crackling sensation may be felt when the skin is pressed. This is caused by gas bubbles produced by the bacteria within the dying tissue.
6. A Foul, Putrid Odor One of the hallmarks of gangrene, particularly wet gangrene, is a distinct and deeply unpleasant smell coming from a wound or the affected area. This putrid odor is the result of bacteria breaking down the decaying tissue and is an unmistakable sign that a serious infectious process is underway.
A Life-Threatening Emergency: Signs of Spreading Infection (Sepsis)
If the bacteria from the gangrenous tissue enter the bloodstream, the infection can spread throughout the entire body, leading to sepsis. Sepsis is a life-threatening medical emergency that can rapidly progress to organ failure and death. If you see any of the localized symptoms above in addition to the following systemic signs, call 911 or go to the nearest emergency room immediately:
Fever or Low Body Temperature: A high fever or, conversely, a body temperature that is abnormally low.
Low Blood Pressure (Hypotension): Often causing dizziness or fainting.
Rapid Heart Rate: The heart beats faster to try to compensate for the low blood pressure.
Shortness of Breath or Rapid Breathing: The body is struggling to get enough oxygen.
Confusion or Altered Mental State: Sudden disorientation, lethargy, or difficulty staying awake.
When it comes to gangrene, time is not on your side. Time lost is tissue lost, and potentially, a life lost. Trust your instincts. If something looks, feels, or smells alarmingly wrong, the only safe course of action is to seek professional medical help without delay.
The Comprehensive Treatment Pathway for Gangrene
Gangrene is a serious and potentially life-threatening medical condition characterized by the death of body tissue. It occurs when the blood supply to an area is cut off, depriving the tissue of oxygen and nutrients, or as the result of a severe bacterial infection. Treating gangrene requires a swift, aggressive, and multi-pronged approach that focuses on three primary goals: removing the dead tissue, treating the infection, and addressing the underlying cause to restore blood flow and prevent recurrence.
The specific treatment plan is tailored to the individual patient, depending on the type of gangrene (dry, wet, or gas), its location, its severity, and the patient’s overall health. Below is a detailed exploration of the key treatment methods employed by medical professionals in the race against time to save limbs and lives.
Core Treatment Interventions
1. Surgical Debridement: Clearing the Battlefield
Purpose: To remove all dead and infected tissue.
Description: Surgical debridement is the cornerstone of gangrene management. A surgeon meticulously cuts away all the necrotic (dead) and infected tissue. This process is crucial for several reasons. Firstly, it physically removes the source of infection and the toxins being produced by bacteria. Secondly, it prevents the gangrene from spreading to adjacent healthy tissue. Finally, by creating a clean wound bed, it prepares the area for healing or further reconstructive procedures. Depending on the extent of the tissue death, multiple debridement procedures may be necessary over several days to ensure all non-viable tissue is gone.
2. Amputation: The Life-Saving Last Resort
Purpose: To save a patient’s life when tissue damage is extensive and irreversible.
Description: In the most severe cases of gangrene, tissue damage is so profound that the limb cannot be salvaged. When debridement is not enough to control the spread, or when the entire limb has lost its blood supply, amputation becomes a necessary, life-saving measure. The decision to amputate is never taken lightly but is essential to stop a raging infection and the systemic release of toxins that can lead to sepsis and death. The surgery aims to remove the limb at a level where the remaining tissue is healthy and has adequate blood flow, which is critical for the healing of the surgical wound (the stump).
3. Antibiotic Therapy: Combating the Infection from Within
Purpose: To fight the systemic bacterial infection.
Description: For wet or gas gangrene, where bacterial infection is a primary driver, antibiotic therapy is critical. Patients are typically administered powerful, broad-spectrum antibiotics directly into the bloodstream through an intravenous (IV) line. This method ensures the medication is delivered rapidly and in high concentrations throughout the body to fight the infection. Whenever possible, tissue and fluid samples from the wound are sent to a lab to identify the specific bacteria responsible. This allows doctors to switch to more targeted antibiotics that are most effective against the identified pathogen, helping to prevent the development of sepsis—a life-threatening overreaction of the body to infection.
4. Vascular Surgery: Restoring Critical Blood Flow
Purpose: To restore blood supply to the affected area, treating the root cause.
Description: Since most cases of gangrene (especially dry gangrene) are caused by a lack of blood flow due to peripheral artery disease, addressing this underlying circulatory problem is vital for healing and preventing recurrence. Vascular surgeons can perform several procedures to re-establish circulation:
Angioplasty: A thin tube with a balloon at its tip is threaded into the blocked artery. The balloon is inflated, compressing the plaque against the artery walls and widening the vessel.
Stent Placement: Often performed with angioplasty, a tiny wire-mesh tube called a stent is placed inside the artery to prop it open and ensure it remains clear.
Bypass Surgery: A surgeon creates a new pathway for blood to flow by grafting a blood vessel from another part of the body (or a synthetic tube) to circumvent the blocked section of the artery.
Adjunctive and Supportive Therapies
5. Hyperbaric Oxygen Therapy (HBOT)
Purpose: To promote healing and kill oxygen-intolerant bacteria.
Description: This therapy involves the patient lying in a special chamber that is pressurized with 100% pure oxygen. The high-pressure environment allows the lungs to gather up to three times more oxygen than normal, which saturates the blood plasma. This oxygen-rich blood can better penetrate tissues with poor circulation, promoting the growth of new skin cells and blood vessels. For gas gangrene, HBOT is particularly effective because the bacteria that cause it (Clostridium) are anaerobic, meaning they cannot survive in a high-oxygen environment.
6. Maggot Therapy (Biodebridement)
Purpose: A form of natural, highly precise debridement.
Description: While it may sound unsettling, maggot therapy is a highly effective and well-established medical practice. Medical-grade, sterile larvae of the green bottle fly are placed on the wound and covered with a special dressing. These maggots have a unique ability to consume only the dead, necrotic tissue, leaving healthy tissue completely unharmed. As they work, they also secrete substances that have antimicrobial properties, effectively disinfecting the wound and promoting healing. This method can be a gentler and more precise alternative to surgical debridement for certain types of non-healing wounds.





