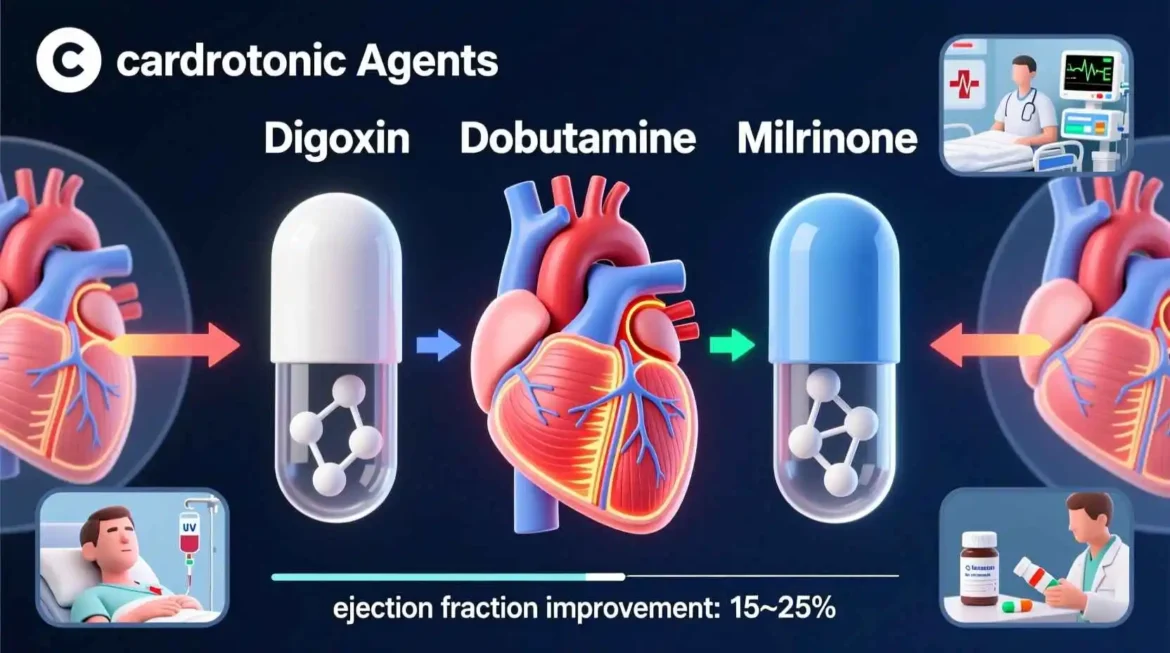
Cardiotonic Agents: Examples, Uses, and Clinical Applications
Cardiotonic agents represent a crucial class of medications in modern pharmacology, playing an indispensable role in the management of various cardiovascular conditions. These agents, also known as inotropic agents, are substances that alter the force or energy of muscular contractions, particularly in the heart muscle. Their primary function is to enhance cardiac contractility, making them invaluable in treating conditions characterized by impaired cardiac output and heart failure.
The field of cardiotonic agents has evolved significantly over the past century, from the early use of digitalis compounds to the development of sophisticated synthetic agents with specific mechanisms of action. Today, healthcare professionals have access to a diverse array of cardiotonic agents, each with unique pharmacological profiles, indications, and considerations for use.
This comprehensive guide explores the world of cardiotonic agents in depth, examining their mechanisms of action, classification, specific examples with detailed pharmacological profiles, clinical applications, adverse effects, contraindications, and future directions in research and development. Additionally, this guide addresses frequently asked questions about these important medications, providing healthcare professionals, students, and interested readers with a thorough understanding of their role in cardiovascular medicine.
Understanding Cardiac Function and the Role of Cardiotonic Agents
Before delving into the specifics of cardiotonic agents, it is essential to understand the fundamental aspects of cardiac function that these medications aim to influence. The heart functions as a muscular pump that circulates blood throughout the body, delivering oxygen and nutrients to tissues while removing waste products. This pumping action is the result of coordinated contractions of cardiac muscle cells, or cardiomyocytes.
Cardiac contraction is a complex process involving electrical, chemical, and mechanical events. It begins with an electrical impulse that spreads through the heart, triggering the release of calcium ions within cardiomyocytes. These calcium ions interact with contractile proteins, ultimately resulting in muscle contraction and the ejection of blood from the heart’s chambers.
In certain pathological conditions, this process becomes impaired, leading to decreased cardiac output and the clinical syndrome of heart failure. Heart failure affects millions of people worldwide and is associated with significant morbidity and mortality. It is in this context that cardiotonic agents become therapeutically valuable, as they can enhance the force of cardiac contraction, thereby improving cardiac output and alleviating the symptoms of heart failure.
Cardiotonic agents work through various mechanisms to enhance cardiac contractility. Some increase the availability of calcium ions within cardiomyocytes, while others enhance the sensitivity of contractile proteins to calcium. Still others work through different pathways, such as inhibiting enzymes that break down cyclic AMP, a molecule that plays a crucial role in cardiac contraction.
Understanding these mechanisms is essential for healthcare professionals, as it allows for the appropriate selection of cardiotonic agents based on the specific pathophysiology of a patient’s condition. It also helps in anticipating and managing potential adverse effects, which can vary significantly among different classes of cardiotonic agents.
Classification of Cardiotonic Agents
Cardiotonic agents can be classified into several categories based on their mechanisms of action, chemical structures, and pharmacological properties. This classification is not merely academic; it has important clinical implications, as agents within the same class often share similar therapeutic effects, adverse effect profiles, and considerations for use.
The major classes of cardiotonic agents include:
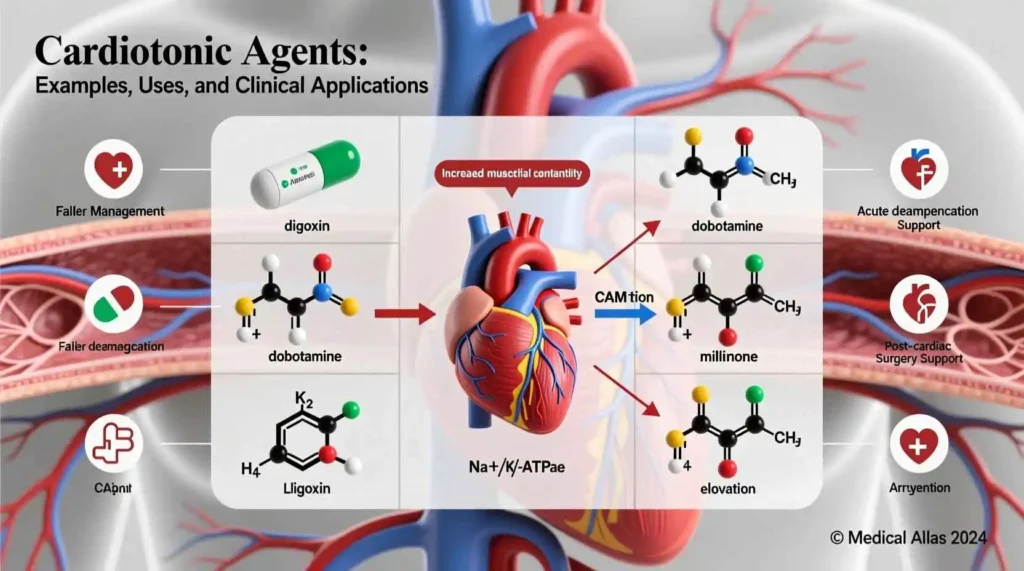
Cardiac glycosides: This class includes some of the oldest known cardiotonic agents, such as digoxin and digitoxin. These compounds work by inhibiting the sodium-potassium pump in cardiac cells, leading to increased intracellular calcium concentrations and enhanced cardiac contractility.
Beta-adrenergic agonists: These agents stimulate beta-adrenergic receptors in the heart, leading to increased cyclic AMP levels and enhanced cardiac contractility. Examples include dobutamine, dopamine, and isoproterenol.
Phosphodiesterase inhibitors: These medications work by inhibiting the enzyme phosphodiesterase, which breaks down cyclic AMP. By preserving cyclic AMP levels, they enhance cardiac contractility. Examples include milrinone and inamrinone.
Calcium sensitizers: This newer class of cardiotonic agents works by increasing the sensitivity of cardiac contractile proteins to calcium, rather than by increasing calcium concentrations themselves. Levosimendan is the most well-known example in this class.
Thyroid hormones: Although not typically classified as cardiotonic agents, thyroid hormones have significant effects on cardiac contractility and may be used in specific clinical situations.
Each of these classes will be explored in detail in subsequent sections, with particular attention to their mechanisms of action, specific examples, clinical applications, and considerations for use.
Cardiac Glycosides: Mechanism and Clinical Applications
Cardiac glycosides represent one of the oldest classes of cardiotonic agents, with a history dating back centuries. The use of digitalis, a plant extract containing cardiac glycosides, was first described in the treatment of heart conditions in the 18th century. Today, the most commonly used cardiac glycoside is digoxin, which remains an important medication in the management of certain cardiovascular conditions.
The mechanism of action of cardiac glycosides is both elegant and complex. These compounds work by inhibiting the sodium-potassium pump, also known as Na+/K+-ATPase, in cardiac cell membranes. This inhibition leads to an increase in intracellular sodium concentrations, which in turn affects the sodium-calcium exchanger, a protein that normally removes calcium from cells in exchange for sodium. As intracellular sodium levels rise, less calcium is removed from the cell, resulting in increased intracellular calcium concentrations.
This increase in intracellular calcium has several effects on cardiac function. Most importantly, it enhances the force of cardiac contraction by increasing the amount of calcium available to interact with contractile proteins. Additionally, cardiac glycosides have effects on the electrical conduction system of the heart, particularly the atrioventricular node, where they slow conduction. This effect is valuable in controlling certain cardiac arrhythmias.
Digoxin is the most widely used cardiac glycoside in modern clinical practice. It is indicated for the treatment of mild to moderate heart failure and for controlling ventricular rate in patients with atrial fibrillation. In heart failure, digoxin improves symptoms and reduces hospitalizations, although it has not been shown to significantly improve survival. In atrial fibrillation, digoxin helps control the ventricular rate by slowing conduction through the atrioventricular node.
The pharmacokinetics of digoxin are characterized by relatively slow absorption, extensive tissue distribution, and primarily renal elimination. This profile has important clinical implications, particularly in patients with renal impairment, who may require dose adjustments to avoid toxicity.
Cardiac glycosides have a narrow therapeutic index, meaning that the difference between therapeutic and toxic doses is small. This characteristic necessitates careful dosing and monitoring, particularly in patients with renal impairment, electrolyte imbalances, or those taking other medications that may interact with digoxin.
Despite their long history of use, cardiac glycosides remain relevant in modern cardiovascular medicine. Their unique combination of inotropic and electrophysiological effects makes them particularly valuable in certain clinical scenarios, and they continue to be included in treatment guidelines for heart failure and atrial fibrillation.
Beta-Adrenergic Agonists as Cardiotonic Agents
Beta-adrenergic agonists represent another important class of cardiotonic agents, working through a mechanism distinct from that of cardiac glycosides. These medications stimulate beta-adrenergic receptors in the heart, leading to a cascade of intracellular events that ultimately enhance cardiac contractility.
The mechanism of action of beta-adrenergic agonists begins with their binding to beta-adrenergic receptors on cardiac cell membranes. This binding activates a G-protein, which in turn stimulates the enzyme adenylate cyclase. Adenylate cyclase converts ATP to cyclic AMP (cAMP), a crucial second messenger in cardiac cells. Increased cAMP levels activate protein kinase A, which phosphorylates various proteins involved in cardiac contraction, including L-type calcium channels and phospholamban.
The phosphorylation of L-type calcium channels increases calcium influx into cardiac cells during each heartbeat, while the phosphorylation of phospholamban enhances calcium uptake into the sarcoplasmic reticulum, a specialized organelle that stores and releases calcium in cardiac cells. Both of these effects lead to increased intracellular calcium concentrations during contraction, enhancing the force of cardiac contraction.
Dobutamine is one of the most commonly used beta-adrenergic agonists with cardiotonic properties. It is a synthetic catecholamine that primarily stimulates beta-1 adrenergic receptors in the heart, with lesser effects on beta-2 and alpha-1 receptors. This selectivity makes dobutamine particularly valuable as a cardiotonic agent, as it enhances cardiac contractility with relatively minimal effects on heart rate and peripheral vascular resistance.
Dobutamine is primarily used in the short-term management of acute decompensated heart failure and cardiogenic shock. It is administered intravenously and typically reserved for situations where oral medications are insufficient or inappropriate. The effects of dobutamine are rapid in onset, making it valuable in acute settings, but also short-lived, necessitating continuous infusion for sustained effect.
Dopamine is another beta-adrenergic agonist with cardiotonic properties, although its effects are more complex than those of dobutamine. At low doses, dopamine primarily stimulates dopamine receptors, leading to vasodilation in certain vascular beds. At moderate doses, it stimulates beta-adrenergic receptors, enhancing cardiac contractility. At high doses, it stimulates alpha-adrenergic receptors, causing vasoconstriction. This dose-dependent effect profile makes dopamine a versatile medication, but also necessitates careful dosing and monitoring.
Isoproterenol is a non-selective beta-adrenergic agonist that stimulates both beta-1 and beta-2 receptors. It has potent cardiotonic effects but also significantly increases heart rate and can cause vasodilation. These effects limit its use as a pure cardiotonic agent, but it remains valuable in certain specific situations, such as the management of bradycardia or heart block.
Beta-adrenergic agonists are generally reserved for short-term use in acute settings due to several limitations. Prolonged use can lead to receptor downregulation, reducing their effectiveness over time. Additionally, their stimulatory effects on the heart can increase myocardial oxygen demand, potentially exacerbating ischemia in patients with coronary artery disease. They can also cause arrhythmias, particularly at higher doses.
Despite these limitations, beta-adrenergic agonists remain essential tools in the management of acute cardiac conditions. Their rapid onset of action and potent effects make them invaluable in situations where immediate enhancement of cardiac contractility is necessary, such as in cardiogenic shock or severe acute decompensated heart failure.
Phosphodiesterase Inhibitors: Mechanism and Clinical Use
Phosphodiesterase inhibitors represent a third major class of cardiotonic agents, working through a mechanism that complements those of cardiac glycosides and beta-adrenergic agonists. These medications have gained importance in clinical practice, particularly for the management of acute heart failure and cardiogenic shock.
The mechanism of action of phosphodiesterase inhibitors centers on their ability to inhibit the enzyme phosphodiesterase, which is responsible for breaking down cyclic AMP (cAMP) in cardiac cells. By inhibiting this enzyme, phosphodiesterase inhibitors increase intracellular cAMP levels, similar to the effect of beta-adrenergic agonists but through a different pathway.
Increased cAMP levels activate protein kinase A, which phosphorylates various proteins involved in cardiac contraction, including L-type calcium channels and phospholamban. The phosphorylation of L-type calcium channels increases calcium influx into cardiac cells during each heartbeat, while the phosphorylation of phospholamban enhances calcium uptake into the sarcoplasmic reticulum. Both of these effects lead to increased intracellular calcium concentrations during contraction, enhancing the force of cardiac contraction.
In addition to their inotropic effects, phosphodiesterase inhibitors also have vasodilatory properties, making them inodilators. This combination of enhanced cardiac contractility and reduced peripheral vascular resistance can be particularly beneficial in patients with heart failure, as it improves cardiac output while reducing the workload on the heart.
Milrinone is the most commonly used phosphodiesterase inhibitor in modern clinical practice. It is a selective inhibitor of phosphodiesterase type III, the predominant form found in cardiac and vascular smooth muscle. Milrinone is administered intravenously and is primarily used for the short-term management of acute decompensated heart failure and cardiogenic shock.
The pharmacokinetics of milrinone are characterized by rapid onset of action and a half-life of approximately 2-4 hours in patients with normal renal function. It is primarily eliminated by renal excretion, necessitating dose adjustments in patients with renal impairment.
Inamrinone (formerly known as amrinone) is another phosphodiesterase inhibitor, although it is used less frequently than milrinone due to a higher incidence of adverse effects, particularly thrombocytopenia. Its mechanism of action and clinical applications are similar to those of milrinone.
Phosphodiesterase inhibitors are generally well-tolerated, although they can cause several adverse effects. The most common include hypotension, due to their vasodilatory effects, and arrhythmias, due to their stimulatory effects on the heart. Other potential adverse effects include headache, nausea, and, in the case of inamrinone, thrombocytopenia.
The use of phosphodiesterase inhibitors is generally reserved for short-term management of acute heart failure and cardiogenic shock. They are particularly valuable in patients who have not responded adequately to other treatments, such as diuretics and beta-adrenergic agonists. Their vasodilatory effects make them particularly useful in patients with elevated systemic vascular resistance.
Phosphodiesterase inhibitors represent an important addition to the armamentarium of cardiotonic agents. Their unique combination of inotropic and vasodilatory effects makes them particularly valuable in certain clinical scenarios, and they continue to play an important role in the management of acute cardiac conditions.
Calcium Sensitizers: A Newer Class of Cardiotonic Agents
Calcium sensitizers represent a relatively newer class of cardiotonic agents, working through a mechanism distinct from those of cardiac glycosides, beta-adrenergic agonists, and phosphodiesterase inhibitors. These medications have generated significant interest in recent years due to their unique mechanism of action and potential advantages over traditional cardiotonic agents.
The mechanism of action of calcium sensitizers centers on their ability to increase the sensitivity of cardiac contractile proteins to calcium, rather than by increasing intracellular calcium concentrations themselves. This distinction is important, as many of the adverse effects associated with traditional cardiotonic agents are related to increased intracellular calcium levels.
Calcium sensitizers work by binding to cardiac troponin C, a protein that plays a crucial role in cardiac contraction. When calcium binds to troponin C, it initiates a conformational change that allows actin and myosin to interact, resulting in muscle contraction. Calcium sensitizers stabilize the calcium-bound conformation of troponin C, enhancing the interaction between actin and myosin and increasing the force of contraction without increasing intracellular calcium concentrations.
Levosimendan is the most well-known calcium sensitizer and has been approved for use in several countries, although it is not yet available in the United States. In addition to its calcium-sensitizing effects, levosimendan also has vasodilatory properties, making it an inodilator similar to phosphodiesterase inhibitors.
The pharmacokinetics of levosimendan are characterized by rapid onset of action and a half-life of approximately 1 hour in patients with normal hepatic function. It is metabolized to an active metabolite with a much longer half-life of approximately 75-80 hours, which contributes to its sustained hemodynamic effects.
Levosimendan is primarily used for the short-term management of acute decompensated heart failure. It has been shown to improve cardiac output and reduce pulmonary capillary wedge pressure, while also having beneficial effects on renal function and neurohormonal activation.
One of the potential advantages of levosimendan over traditional cardiotonic agents is its more favorable effect on myocardial oxygen consumption. By enhancing cardiac contractility without increasing intracellular calcium concentrations, levosimendan may improve cardiac output with less increase in myocardial oxygen demand compared to agents that increase intracellular calcium.
Another potential advantage is its effect on coronary blood flow. Levosimendan has been shown to dilate coronary arteries, potentially improving myocardial oxygen supply. This combination of reduced oxygen demand and increased supply may be particularly beneficial in patients with ischemic heart disease.
Despite these potential advantages, levosimendan is not without limitations. It can cause hypotension due to its vasodilatory effects, and it may also cause headache and nausea. Additionally, its long-acting metabolite can accumulate in patients with renal impairment, necessitating dose adjustments or avoidance in this population.
Calcium sensitizers represent an exciting development in the field of cardiotonic agents. Their unique mechanism of action and potential advantages over traditional agents make them a valuable addition to the armamentarium for the management of acute heart failure. As research continues, it is likely that additional agents in this class will be developed, further expanding the options available to clinicians.
Other Agents with Cardiotonic Properties
In addition to the major classes of cardiotonic agents discussed above, several other medications and substances have cardiotonic properties and may be used in specific clinical situations. While not typically classified primarily as cardiotonic agents, their effects on cardiac contractility make them worthy of consideration in a comprehensive discussion of this topic.
Thyroid hormones, particularly triiodothyronine (T3), have significant effects on cardiac function. They enhance cardiac contractility by several mechanisms, including increasing the expression of sarcoplasmic reticulum calcium-ATPase, enhancing beta-adrenergic receptor density, and improving myocardial energy metabolism. In patients with hypothyroidism, thyroid hormone replacement can improve cardiac function. Additionally, intravenous T3 has been studied as a treatment for patients with heart failure, although its use remains investigational.
Insulin has been recognized to have cardiotonic properties, particularly at high doses. It enhances cardiac contractility by several mechanisms, including increasing intracellular calcium concentrations and improving myocardial glucose utilization. High-dose insulin has been studied as a treatment for acute decompensated heart failure and cardiogenic shock, with some promising results. However, its use is limited by the risk of hypoglycemia and the need for careful monitoring of blood glucose levels.
Vasopressin, also known as antidiuretic hormone, has complex effects on cardiovascular function. While primarily known for its vasoconstrictive effects, it also has been shown to have positive inotropic effects in some studies. These effects may be mediated through V1 receptors in the heart, although the exact mechanism remains unclear. Vasopressin is primarily used for the management of vasodilatory shock, but its potential cardiotonic effects may contribute to its hemodynamic benefits.
Glucagon has cardiotonic properties that have been recognized for decades. It enhances cardiac contractility by increasing intracellular cAMP levels through a mechanism distinct from that of beta-adrenergic agonists. Glucagon is primarily used for the treatment of severe hypoglycemia, but it has also been used as a cardiotonic agent in patients with beta-blocker overdose, where it can overcome the beta-blockade and enhance cardiac contractility.
Levosimendan, while primarily classified as a calcium sensitizer, also has phosphodiesterase inhibitory effects at higher concentrations. This dual mechanism of action contributes to its cardiotonic effects and may provide additional benefits in certain clinical situations.
Istaroxime is an investigational agent that combines inhibition of the sodium-potassium pump (similar to cardiac glycosides) with stimulation of the sarcoplasmic reticulum calcium-ATPase. This dual mechanism of action enhances cardiac contractility while also promoting myocardial relaxation, potentially offering advantages over traditional cardiotonic agents. While still under investigation, istaroxime represents an exciting new approach to the management of heart failure.
Omecamtiv mecarbil is another investigational agent that enhances cardiac contractility through a unique mechanism. It is a cardiac myosin activator that directly stimulates the activity of cardiac myosin, the motor protein responsible for muscle contraction. By increasing the rate of transition of myosin to the force-producing state, omecamtiv mecarbil enhances cardiac contractility without increasing intracellular calcium concentrations or myocardial oxygen consumption. This mechanism of action has generated significant interest, and omecamtiv mecarbil is currently under investigation in large clinical trials.
These diverse agents with cardiotonic properties highlight the complexity of cardiac function and the multiple pathways through which it can be modulated. While many of these agents are not yet widely used in clinical practice, they represent the cutting edge of cardiovascular pharmacology and may offer new options for the management of heart failure and other conditions in the future.
Clinical Applications of Cardiotonic Agents
Cardiotonic agents have a wide range of clinical applications, primarily centered around the management of heart failure and other conditions characterized by impaired cardiac function. Understanding these applications is essential for healthcare professionals, as it allows for the appropriate selection and use of these medications in various clinical scenarios.
The most common application of cardiotonic agents is in the management of acute decompensated heart failure. This condition, characterized by a rapid onset of symptoms due to worsening cardiac function, often requires immediate intervention to improve cardiac output and relieve symptoms. Cardiotonic agents such as dobutamine, milrinone, and levosimendan can be used in this setting to enhance cardiac contractility and improve hemodynamics.
Cardiogenic shock represents another critical application of cardiotonic agents. This life-threatening condition, characterized by inadequate cardiac output despite adequate intravascular volume, often requires aggressive intervention to support cardiac function. Cardiotonic agents such as dobutamine, dopamine, and milrinone are commonly used in this setting, often in combination with vasopressors and other supportive measures.
Cardiotonic agents may also be used in the management of chronic heart failure, although their role in this setting is more limited. Digoxin, for example, is used in selected patients with chronic heart failure to improve symptoms and reduce hospitalizations, although it has not been shown to improve survival. Other cardiotonic agents are generally avoided in chronic heart failure due to concerns about long-term safety and efficacy.
Cardiac surgery represents another important clinical application of cardiotonic agents. Patients undergoing cardiac surgery often experience temporary impairment of cardiac function due to the effects of cardiopulmonary bypass, myocardial ischemia during the procedure, and other factors. Cardiotonic agents such as dobutamine, milrinone, and epinephrine are commonly used in this setting to support cardiac function during and after surgery.
Cardiotonic agents may also be used in the management of certain cardiac arrhythmias. Digoxin, for example, is used to control ventricular rate in patients with atrial fibrillation, taking advantage of its effects on the atrioventricular node. Other cardiotonic agents may be used in specific arrhythmia situations, although their use in this context is generally limited.
The selection of a specific cardiotonic agent depends on several factors, including the clinical scenario, the patient’s underlying condition, and the specific hemodynamic goals. For example, a patient with acute decompensated heart failure and low cardiac output might benefit from dobutamine or milrinone, while a patient with cardiogenic shock and hypotension might require dopamine or epinephrine.
The dosing and administration of cardiotonic agents also vary depending on the specific agent and the clinical situation. Some agents, such as digoxin, can be administered orally and are used for long-term management. Others, such as dobutamine and milrinone, are administered intravenously and are generally reserved for short-term use in acute settings.
Monitoring of patients receiving cardiotonic agents is essential to ensure efficacy and safety. This monitoring typically includes assessment of hemodynamic parameters, such as blood pressure, heart rate, and cardiac output, as well as monitoring for adverse effects, such as arrhythmias and signs of toxicity.
The clinical applications of cardiotonic agents continue to evolve as new agents are developed and new evidence emerges. Healthcare professionals must stay current with the latest research and guidelines to ensure the optimal use of these important medications.
Adverse Effects and Safety Considerations