While cardiotonic agents can be life-saving in certain clinical situations, they also carry the risk of significant adverse effects and safety considerations. Understanding these potential risks is essential for healthcare professionals, as it allows for the appropriate selection, dosing, and monitoring of these medications.
Cardiac glycosides, particularly digoxin, are associated with several significant adverse effects, primarily due to their narrow therapeutic index. Digoxin toxicity can manifest with a wide range of symptoms, including gastrointestinal symptoms such as nausea, vomiting, and abdominal pain; neurological symptoms such as headache, dizziness, and confusion; and visual disturbances such as blurred vision or yellow-green halos. Cardiac arrhythmias are perhaps the most serious manifestation of digoxin toxicity and can include virtually any type of arrhythmia, although ventricular arrhythmias and heart block are particularly concerning.
Several factors increase the risk of digoxin toxicity, including renal impairment (which reduces digoxin clearance), electrolyte imbalances (particularly hypokalemia, hypomagnesemia, and hypercalcemia), and drug interactions (such as with amiodarone, verapamil, and quinidine, which can increase digoxin levels). Careful dosing, monitoring of serum digoxin levels, and attention to these risk factors are essential for the safe use of digoxin.
Beta-adrenergic agonists such as dobutamine and dopamine are also associated with significant adverse effects. These agents can cause tachycardia (rapid heart rate), which can increase myocardial oxygen demand and potentially exacerbate ischemia in patients with coronary artery disease. They can also cause arrhythmias, particularly ventricular arrhythmias, which can be life-threatening. Other potential adverse effects include hypotension (due to vasodilation), hypertension (particularly with dopamine at higher doses), and nausea and vomiting.
Phosphodiesterase inhibitors such as milrinone and inamrinone are generally better tolerated than beta-adrenergic agonists but still carry significant risks. Hypotension is a common adverse effect due to their vasodilatory properties, particularly in patients who are volume-depleted or have pre-existing hypotension. Arrhythmias can also occur, although perhaps less frequently than with beta-adrenergic agonists. Inamrinone is associated with a higher risk of thrombocytopenia (low platelet count), which can limit its use.
Calcium sensitizers such as levosimendan have a more favorable adverse effect profile compared to traditional cardiotonic agents, but they are not without risks. Hypotension can occur due to their vasodilatory effects, particularly at higher doses. Headache and nausea are also relatively common. The long-acting metabolite of levosimendan can accumulate in patients with renal impairment, potentially prolonging its effects and increasing the risk of adverse effects.
Other agents with cardiotonic properties also carry risks. High-dose insulin can cause hypoglycemia, which can be severe if not carefully monitored. Vasopressin can cause excessive vasoconstriction, leading to ischemia in various organs. Glucagon can cause nausea and vomiting, and its use in patients with pheochromocytoma can precipitate a hypertensive crisis.
Several general safety considerations apply to the use of cardiotonic agents. These medications should generally be initiated at low doses and titrated carefully based on the patient’s response and tolerance. Hemodynamic monitoring is essential to assess efficacy and detect adverse effects early. Patients should be monitored for signs of ischemia, arrhythmias, and other adverse effects.
Drug interactions are another important safety consideration. Many cardiotonic agents interact with other medications, potentially altering their effects or increasing the risk of adverse effects. For example, digoxin interacts with numerous medications, including diuretics (which can cause electrolyte imbalances), antiarrhythmics (which can increase digoxin levels), and beta-blockers (which can alter heart rate and conduction).
Special populations require particular attention when using cardiotonic agents. Elderly patients may be more sensitive to the effects of these medications and may require lower doses. Patients with renal impairment may require dose adjustments for agents that are primarily eliminated by the kidneys, such as digoxin and milrinone. Patients with hepatic impairment may require dose adjustments for agents that are metabolized by the liver, such as levosimendan.
Despite these risks and considerations, cardiotonic agents remain essential tools in the management of various cardiovascular conditions. By understanding their adverse effect profiles and implementing appropriate safety measures, healthcare professionals can maximize their benefits while minimizing their risks.
Contraindications and Precautions
Cardiotonic agents, like all medications, have specific contraindications and precautions that must be considered before their use. Understanding these contraindications and precautions is essential for healthcare professionals, as it allows for the safe and appropriate use of these medications.
Cardiac glycosides such as digoxin have several important contraindications and precautions. They are contraindicated in patients with ventricular fibrillation, as they can exacerbate this life-threatening arrhythmia. They are also contraindicated in patients with known hypersensitivity to cardiac glycosides. Precautions should be taken in patients with renal impairment, as digoxin is primarily eliminated by the kidneys and can accumulate to toxic levels in this population. Electrolyte imbalances, particularly hypokalemia, hypomagnesemia, and hypercalcemia, can increase the risk of digoxin toxicity and should be corrected before initiating digoxin therapy. Digoxin should also be used with caution in patients with conduction abnormalities, such as heart block, as it can further impair conduction.
Beta-adrenergic agonists such as dobutamine and dopamine also have several contraindications and precautions. They are contraindicated in patients with tachyarrhythmias or ventricular fibrillation, as they can exacerbate these arrhythmias. They are also contraindicated in patients with known hypersensitivity to these medications. Precautions should be taken in patients with coronary artery disease, as these agents can increase myocardial oxygen demand and potentially exacerbate ischemia. They should also be used with caution in patients with hypertension, as they can increase blood pressure, particularly at higher doses. Patients with hyperthyroidism may be more sensitive to the effects of beta-adrenergic agonists and may require lower doses.
Phosphodiesterase inhibitors such as milrinone and inamrinone have their own set of contraindications and precautions. They are contraindicated in patients with severe hypotension, as their vasodilatory effects can further lower blood pressure. They are also contraindicated in patients with known hypersensitivity to these medications. Precautions should be taken in patients with renal impairment, as milrinone is primarily eliminated by the kidneys and can accumulate to toxic levels in this population. Inamrinone should be used with caution in patients with thrombocytopenia or a history of thrombocytopenia, as it can cause or exacerbate this condition. Phosphodiesterase inhibitors should also be used with caution in patients with arrhythmias, as they can increase the risk of arrhythmias.
Calcium sensitizers such as levosimendan have fewer contraindications and precautions compared to traditional cardiotonic agents, but they are not without risks. They are contraindicated in patients with severe hypotension, as their vasodilatory effects can further lower blood pressure. They are also contraindicated in patients with known hypersensitivity to levosimendan. Precautions should be taken in patients with renal impairment, as the active metabolite of levosimendan can accumulate in this population. They should also be used with caution in patients with hepatic impairment, as levosimendan is metabolized by the liver.
Other agents with cardiotonic properties also have specific contraindications and precautions. High-dose insulin is contraindicated in patients with hypoglycemia and should be used with caution in patients with renal impairment, as insulin is partially eliminated by the kidneys. Vasopressin is contraindicated in patients with known hypersensitivity to vasopressin and should be used with caution in patients with coronary artery disease, as it can cause vasoconstriction and potentially exacerbate ischemia. Glucagon is contraindicated in patients with pheochromocytoma, as it can precipitate a hypertensive crisis in this population.
Several general precautions apply to the use of cardiotonic agents. These medications should generally be used with caution in patients with arrhythmias, as they can increase the risk of arrhythmias. They should also be used with caution in patients with ischemic heart disease, as they can increase myocardial oxygen demand and potentially exacerbate ischemia. Patients with severe hypotension may not tolerate the vasodilatory effects of some cardiotonic agents, such as phosphodiesterase inhibitors and calcium sensitizers.
Special populations require particular attention when using cardiotonic agents. Elderly patients may be more sensitive to the effects of these medications and may require lower doses. Patients with renal impairment may require dose adjustments for agents that are primarily eliminated by the kidneys. Patients with hepatic impairment may require dose adjustments for agents that are metabolized by the liver. Pregnant and breastfeeding women should be treated with caution, as the safety of many cardiotonic agents in these populations has not been well established.
Drug interactions are another important consideration when using cardiotonic agents. Many cardiotonic agents interact with other medications, potentially altering their effects or increasing the risk of adverse effects. Healthcare professionals should carefully review a patient’s medication list before initiating a cardiotonic agent and monitor for potential interactions.
Despite these contraindications and precautions, cardiotonic agents remain essential tools in the management of various cardiovascular conditions. By carefully considering these factors and implementing appropriate precautions, healthcare professionals can ensure the safe and effective use of these medications.
Future Directions in Cardiotonic Therapy
The field of cardiotonic therapy continues to evolve, with ongoing research and development aimed at improving the efficacy and safety of these important medications. Several promising directions are currently being explored, with the potential to significantly impact the management of heart failure and other cardiovascular conditions in the future.
One area of active research is the development of new cardiotonic agents with novel mechanisms of action. For example, omecamtiv mecarbil, a cardiac myosin activator, represents a new approach to enhancing cardiac contractility. Unlike traditional cardiotonic agents, which work by increasing intracellular calcium concentrations, omecamtiv mecarbil directly stimulates the activity of cardiac myosin, the motor protein responsible for muscle contraction. This mechanism of action may enhance cardiac contractility without increasing myocardial oxygen demand, potentially offering advantages over traditional agents. Omecamtiv mecarbil is currently under investigation in large clinical trials, and if proven effective and safe, it could represent a significant advance in the management of heart failure.
Istaroxime is another investigational agent with a novel mechanism of action. It combines inhibition of the sodium-potassium pump (similar to cardiac glycosides) with stimulation of the sarcoplasmic reticulum calcium-ATPase. This dual mechanism of action enhances cardiac contractility while also promoting myocardial relaxation, potentially offering advantages over traditional cardiotonic agents. Early studies of istaroxime have shown promising results, and further research is ongoing.
Gene therapy represents another exciting frontier in cardiotonic therapy. Researchers are exploring the potential of gene therapy to enhance cardiac function by targeting specific genes involved in cardiac contraction and relaxation. For example, gene therapy aimed at increasing the expression of sarcoplasmic reticulum calcium-ATPase, a protein that plays a crucial role in myocardial relaxation, has shown promise in early studies. While still in the experimental stages, gene therapy could potentially offer a more targeted and durable approach to enhancing cardiac function.
Stem cell therapy is another area of active research in the field of cardiovascular medicine. While not strictly a cardiotonic therapy, stem cell therapy has the potential to improve cardiac function by regenerating damaged cardiac tissue. Early studies have shown that stem cell therapy can improve cardiac function in patients with heart failure, although the mechanisms underlying these improvements are not fully understood. Further research is needed to determine the optimal type of stem cells, delivery methods, and patient populations for this approach.
Personalized medicine represents another important direction in the future of cardiotonic therapy. Advances in genomics and other fields are making it possible to tailor treatments to individual patients based on their genetic makeup, clinical characteristics, and other factors. For example, genetic testing may help identify patients who are more likely to respond to specific cardiotonic agents or who are at higher risk of adverse effects. This personalized approach could improve the efficacy and safety of cardiotonic therapy.
Improved delivery systems are also being explored to enhance the efficacy and safety of cardiotonic agents. For example, researchers are investigating the potential of targeted delivery systems that could deliver cardiotonic agents directly to the heart, potentially reducing systemic side effects. Nanotechnology and other advanced delivery systems could also improve the bioavailability and duration of action of these medications.
Digital health technologies represent another promising direction in the management of heart failure and other cardiovascular conditions. Remote monitoring devices, mobile applications, and other digital tools can help healthcare providers monitor patients more closely, detect early signs of deterioration, and adjust treatments more promptly. These technologies could potentially improve the management of patients receiving cardiotonic therapy, allowing for more precise dosing and earlier detection of adverse effects.
Finally, a better understanding of the pathophysiology of heart failure and other cardiovascular conditions is driving the development of new therapeutic approaches. Researchers are increasingly recognizing the heterogeneity of heart failure and the importance of targeting specific underlying mechanisms. This more nuanced understanding of cardiovascular disease is leading to the development of more targeted and effective therapies.
The future of cardiotonic therapy is bright, with numerous promising avenues being explored. While traditional cardiotonic agents will continue to play an important role in the management of cardiovascular conditions, these new approaches have the potential to significantly improve outcomes for patients with heart failure and other conditions characterized by impaired cardiac function. Healthcare professionals must stay current with these developments to ensure that their patients benefit from the latest advances in cardiovascular medicine.
Conclusion
Cardiotonic agents represent a diverse and important class of medications in the management of various cardiovascular conditions, particularly heart failure. From the historical use of digitalis to the development of sophisticated synthetic agents with specific mechanisms of action, these medications have evolved significantly over time, offering healthcare professionals an ever-expanding array of options for enhancing cardiac contractility.
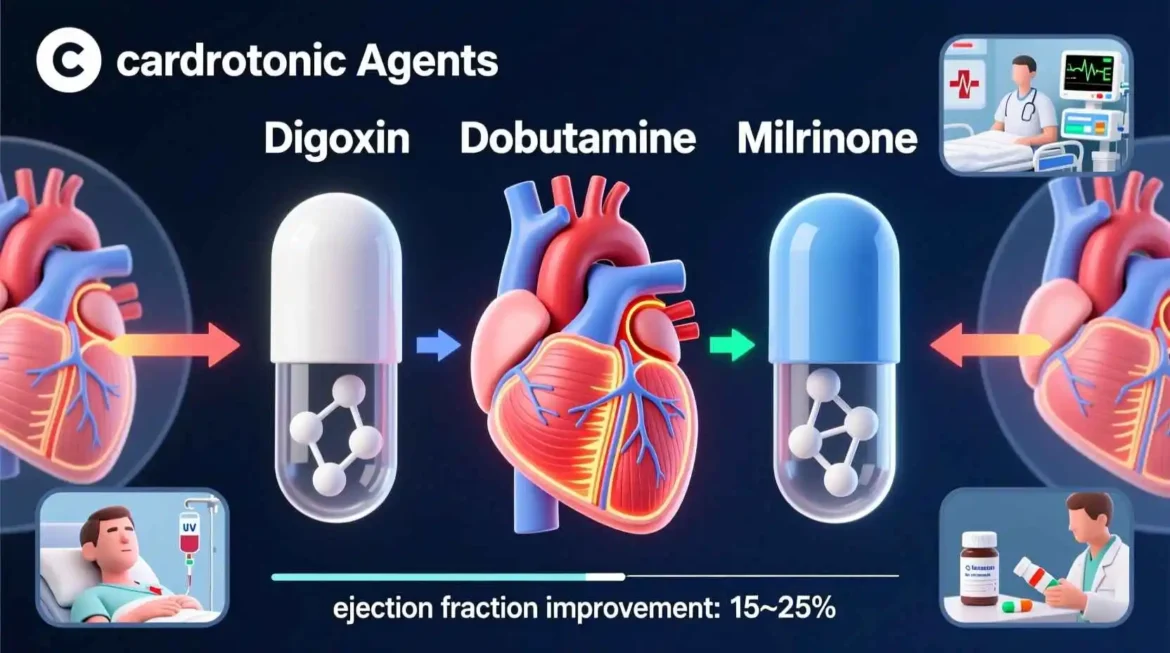
The major classes of cardiotonic agents, including cardiac glycosides, beta-adrenergic agonists, phosphodiesterase inhibitors, and calcium sensitizers, each have unique mechanisms of action, pharmacological profiles, and clinical applications. Understanding these differences is essential for healthcare professionals, as it allows for the appropriate selection of cardiotonic agents based on the specific pathophysiology of a patient’s condition.
While cardiotonic agents can be life-saving in certain clinical situations, they also carry the risk of significant adverse effects and safety considerations. Careful patient selection, dosing, and monitoring are essential to maximize the benefits of these medications while minimizing their risks. Contraindications and precautions must be carefully considered, and special attention must be paid to drug interactions and the needs of special populations.
The field of cardiotonic therapy continues to evolve, with ongoing research and development aimed at improving the efficacy and safety of these medications. Novel agents with new mechanisms of action, gene therapy, stem cell therapy, personalized medicine, improved delivery systems, digital health technologies, and a better understanding of cardiovascular pathophysiology all represent promising directions for the future.
Despite these advances, the fundamental goal of cardiotonic therapy remains the same: to enhance cardiac contractility and improve cardiac output in patients with impaired cardiac function. By combining the wisdom of traditional approaches with the innovations of modern medicine, healthcare professionals can provide the best possible care for patients with heart failure and other cardiovascular conditions.
As our understanding of cardiovascular disease continues to grow and new technologies and therapies emerge, the field of cardiotonic therapy will undoubtedly continue to evolve. Healthcare professionals must stay current with these developments to ensure that their patients benefit from the latest advances in cardiovascular medicine. Through continued research, education, and clinical application, cardiotonic agents will remain an essential tool in the management of cardiovascular disease for years to come.
30 Frequently Asked Questions About Cardiotonic Agents
- What are cardiotonic agents?
Cardiotonic agents, also known as inotropic agents, are medications that alter the force or energy of muscular contractions, particularly in the heart muscle. Their primary function is to enhance cardiac contractility, making them valuable in treating conditions characterized by impaired cardiac output and heart failure.
- How do cardiotonic agents work?
Cardiotonic agents work through various mechanisms to enhance cardiac contractility. Some increase the availability of calcium ions within cardiomyocytes, while others enhance the sensitivity of contractile proteins to calcium. Still others work through different pathways, such as inhibiting enzymes that break down cyclic AMP, a molecule that plays a crucial role in cardiac contraction.
- What are the main classes of cardiotonic agents?
The main classes of cardiotonic agents include cardiac glycosides, beta-adrenergic agonists, phosphodiesterase inhibitors, and calcium sensitizers. Each class works through a distinct mechanism and has unique pharmacological properties and clinical applications.
- What is the most commonly used cardiac glycoside?
Digoxin is the most commonly used cardiac glycoside in modern clinical practice. It is indicated for the treatment of mild to moderate heart failure and for controlling ventricular rate in patients with atrial fibrillation.
- How do cardiac glycosides work?
Cardiac glycosides work by inhibiting the sodium-potassium pump in cardiac cells, leading to increased intracellular sodium concentrations. This affects the sodium-calcium exchanger, resulting in increased intracellular calcium concentrations and enhanced cardiac contractility.
- What are the common side effects of digoxin?
Common side effects of digoxin include gastrointestinal symptoms such as nausea, vomiting, and abdominal pain; neurological symptoms such as headache, dizziness, and confusion; and visual disturbances such as blurred vision or yellow-green halos. Cardiac arrhythmias are the most serious side effect.
- What factors increase the risk of digoxin toxicity?
Several factors increase the risk of digoxin toxicity, including renal impairment, electrolyte imbalances (particularly hypokalemia, hypomagnesemia, and hypercalcemia), and drug interactions (such as with amiodarone, verapamil, and quinidine).
- What are beta-adrenergic agonists and how do they work?
Beta-adrenergic agonists are cardiotonic agents that stimulate beta-adrenergic receptors in the heart, leading to increased cyclic AMP levels and enhanced cardiac contractility. Examples include dobutamine, dopamine, and isoproterenol.
- What is dobutamine used for?
Dobutamine is primarily used for the short-term management of acute decompensated heart failure and cardiogenic shock. It enhances cardiac contractility with relatively minimal effects on heart rate and peripheral vascular resistance.
- How do phosphodiesterase inhibitors work?
Phosphodiesterase inhibitors work by inhibiting the enzyme phosphodiesterase, which breaks down cyclic AMP in cardiac cells. By preserving cyclic AMP levels, they enhance cardiac contractility. Examples include milrinone and inamrinone.
- What is the difference between milrinone and dobutamine?
Milrinone is a phosphodiesterase inhibitor, while dobutamine is a beta-adrenergic agonist. Both enhance cardiac contractility, but they work through different mechanisms. Milrinone also has vasodilatory effects, making it an inodilator, while dobutamine has more selective effects on cardiac contractility.
- What are calcium sensitizers and how do they work?
Calcium sensitizers are a newer class of cardiotonic agents that work by increasing the sensitivity of cardiac contractile proteins to calcium, rather than by increasing calcium concentrations themselves. Levosimendan is the most well-known example in this class.
- What are the advantages of calcium sensitizers over traditional cardiotonic agents?
Calcium sensitizers may have several advantages over traditional cardiotonic agents, including a more favorable effect on myocardial oxygen consumption, improved coronary blood flow, and potentially fewer arrhythmias. However, they are not without risks and limitations.
- What are the clinical applications of cardiotonic agents?
Cardiotonic agents have a wide range of clinical applications, primarily centered around the management of acute decompensated heart failure, cardiogenic shock, cardiac surgery, and certain cardiac arrhythmias. They may also be used in selected patients with chronic heart failure.
- How are cardiotonic agents administered?
The administration of cardiotonic agents varies depending on the specific agent and the clinical situation. Some agents, such as digoxin, can be administered orally and are used for long-term management. Others, such as dobutamine and milrinone, are administered intravenously and are generally reserved for short-term use in acute settings.
- How are patients monitored when receiving cardiotonic agents?
Patients receiving cardiotonic agents require careful monitoring to ensure efficacy and safety. This typically includes assessment of hemodynamic parameters, such as blood pressure, heart rate, and cardiac output, as well as monitoring for adverse effects, such as arrhythmias and signs of toxicity.
- What are the contraindications for cardiotonic agents?
Contraindications for cardiotonic agents vary depending on the specific agent but may include ventricular fibrillation, severe hypotension, known hypersensitivity to the medication, and certain arrhythmias. Healthcare professionals must carefully consider contraindications before initiating cardiotonic therapy.
- What precautions should be taken when using cardiotonic agents?
Precautions when using cardiotonic agents include careful patient selection, dosing, and monitoring; attention to drug interactions; consideration of special populations such as elderly patients and those with renal or hepatic impairment; and awareness of the potential for adverse effects such as arrhythmias and ischemia.
- Can cardiotonic agents be used during pregnancy?
The use of cardiotonic agents during pregnancy requires careful consideration of the potential risks and benefits. Some cardiotonic agents, such as digoxin, have been used in pregnancy with relative safety, while others have less established safety profiles. Healthcare professionals must weigh the risks and benefits for each individual patient.
- Can cardiotonic agents be used in patients with renal impairment?
Many cardiotonic agents require dose adjustments in patients with renal impairment, particularly those that are primarily eliminated by the kidneys, such as digoxin and milrinone. Healthcare professionals must carefully consider renal function when selecting and dosing cardiotonic agents in these patients.
- Can cardiotonic agents be used in patients with hepatic impairment?
Some cardiotonic agents require dose adjustments in patients with hepatic impairment, particularly those that are metabolized by the liver, such as levosimendan. Healthcare professionals must carefully consider hepatic function when selecting and dosing cardiotonic agents in these patients.
- What are the drug interactions with cardiotonic agents?
Cardiotonic agents can interact with numerous other medications, potentially altering their effects or increasing the risk of adverse effects. For example, digoxin interacts with many medications, including diuretics, antiarrhythmics, and beta-blockers. Healthcare professionals must carefully review a patient’s medication list before initiating a cardiotonic agent.
- What is the role of cardiotonic agents in chronic heart failure?
The role of cardiotonic agents in chronic heart failure is limited. Digoxin is used in selected patients to improve symptoms and reduce hospitalizations, although it has not been shown to improve survival. Other cardiotonic agents are generally avoided in chronic heart failure due to concerns about long-term safety and efficacy.
- What is the role of cardiotonic agents in acute heart failure?
Cardiotonic agents play a more significant role in acute heart failure, where they can be used to enhance cardiac contractility and improve hemodynamics. Agents such as dobutamine, milrinone, and levosimendan are commonly used in this setting.
- What is the role of cardiotonic agents in cardiogenic shock?
Cardiotonic agents are essential in the management of cardiogenic shock, where they can enhance cardiac contractility and improve cardiac output. Agents such as dobutamine, dopamine, and epinephrine are commonly used in this setting, often in combination with vasopressors and other supportive measures.
- What is the role of cardiotonic agents in cardiac surgery?
Cardiotonic agents are commonly used in cardiac surgery to support cardiac function during and after the procedure. Patients undergoing cardiac surgery often experience temporary impairment of cardiac function due to the effects of cardiopulmonary bypass, myocardial ischemia during the procedure, and other factors.
- What are the future directions in cardiotonic therapy?
Future directions in cardiotonic therapy include the development of new agents with novel mechanisms of action, gene therapy, stem cell therapy, personalized medicine, improved delivery systems, digital health technologies, and a better understanding of cardiovascular pathophysiology.
- What is omecamtiv mecarbil?
Omecamtiv mecarbil is an investigational cardiotonic agent that works by directly stimulating the activity of cardiac myosin, the motor protein responsible for muscle contraction. Unlike traditional cardiotonic agents, it enhances cardiac contractility without increasing intracellular calcium concentrations or myocardial oxygen consumption.
- What is istaroxime?
Istaroxime is an investigational cardiotonic agent that combines inhibition of the sodium-potassium pump (similar to cardiac glycosides) with stimulation of the sarcoplasmic reticulum calcium-ATPase. This dual mechanism of action enhances cardiac contractility while also promoting myocardial relaxation.
- How can healthcare professionals stay current with developments in cardiotonic therapy?
Healthcare professionals can stay current with developments in cardiotonic therapy by reading medical journals, attending conferences and continuing education programs, participating in professional organizations, and consulting clinical practice guidelines. Staying current is essential to ensure that patients receive the most up-to-date and effective care.
Medical Disclaimer:
The information provided on this website is for general educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.