What Are the Different Types of Asthma Inhalers — And What Comes Next?
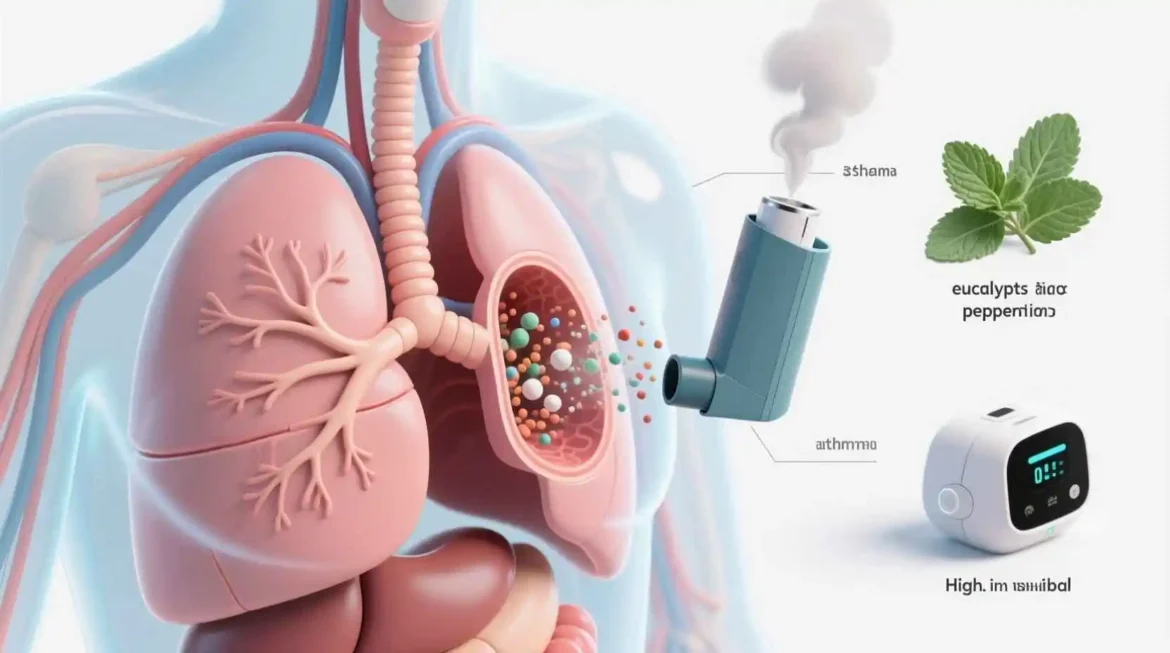
Asthma is a chronic respiratory condition that affects millions of people worldwide, causing inflammation and narrowing of the airways, which leads to difficulty in breathing. One of the most effective ways to manage asthma symptoms is through the use of inhalers. These portable devices deliver medication directly to the lungs, providing quick relief or long-term control of asthma symptoms. In this comprehensive guide, we will explore what asthma inhalers are, the different types available, their potential side effects, and when it’s crucial to seek medical help. Additionally, we’ll address thirty frequently asked questions to provide a thorough understanding of these essential medical devices.
What Are Inhalers?
Inhalers are medical devices designed to deliver medication directly into the lungs through inhalation. They are the primary treatment method for asthma and other respiratory conditions like chronic obstructive pulmonary disease (COPD). The direct delivery system allows the medication to act quickly on the airways with fewer systemic side effects compared to oral medications.
Inhalers work by converting liquid medication into a fine mist or powder that can be easily inhaled. This ensures that the medication reaches the lungs where it’s needed most, rather than circulating throughout the body. The portability of inhalers makes them convenient for asthma patients to carry and use whenever needed, whether at home, work, school, or on the go.
The effectiveness of inhalers depends heavily on proper technique. Studies have shown that many patients do not use their inhalers correctly, which can significantly reduce the amount of medication reaching the lungs. This is why healthcare providers spend time educating patients on the correct inhalation technique and may recommend devices like spacers or valved holding chambers to improve medication delivery.
Inhalers have revolutionized asthma management since their introduction in the mid-20th century. Before inhalers, asthma treatments were less effective and often had more significant side effects. Today, these devices allow people with asthma to lead active, normal lives by providing rapid symptom relief and preventing asthma attacks when used as prescribed.
Types of Asthma Inhalers
Asthma inhalers can be broadly categorized into two main groups based on their function: relievers (or rescue inhalers) and controllers (or preventers). Within these categories, there are different types of inhaler devices, each with its own mechanism of action and advantages.
Reliever Inhalers (Rescue Inhalers)
Reliever inhalers are used for quick relief of asthma symptoms such as wheezing, coughing, chest tightness, and shortness of breath. They contain medications called short-acting bronchodilators, which work rapidly to relax the muscles around the airways, making breathing easier within minutes.
The most common medication in reliever inhalers is albuterol (also known as salbutamol in some countries). Other short-acting bronchodilators include levalbuterol and pirbuterol. These medications typically provide relief for 4-6 hours and are meant to be used only when needed, not on a regular schedule.
Reliever inhalers come in various forms, including metered-dose inhalers (MDIs), dry powder inhalers (DPIs), and sometimes as nebulizer solutions for severe asthma attacks. It’s important for patients to always carry their reliever inhaler with them in case of sudden asthma symptoms.
Controller Inhalers (Preventers)
Controller inhalers are used on a daily basis to prevent asthma symptoms and reduce the frequency and severity of asthma attacks. They contain anti-inflammatory medications that help reduce swelling and mucus production in the airways over time.
The most common type of controller inhalers contains inhaled corticosteroids (ICS), such as fluticasone, budesonide, beclomethasone, and mometasone. These medications are the most effective long-term control therapy for asthma and are generally safe when used as prescribed.
Other types of controller medications include:
Long-acting bronchodilators (LABAs) such as salmeterol and formoterol, which relax the airway muscles for up to 12 hours. These are always used in combination with inhaled corticosteroids in asthma management.
Combination inhalers that contain both an inhaled corticosteroid and a long-acting bronchodilator. Examples include Advair (fluticasone/salmeterol), Symbicort (budesonide/formoterol), and Breo (fluticasone/vilanterol).
Leukotriene modifiers are sometimes delivered through inhalers, though they are more commonly available as oral medications.
Mast cell stabilizers like cromolyn sodium, which help prevent asthma attacks by reducing inflammation.
Types of Inhaler Devices
Beyond the medication categories, asthma inhalers come in different device types, each requiring specific techniques for proper use:
Metered-Dose Inhalers (MDIs): These are the most common type of inhaler. They consist of a pressurized canister containing medication that releases a pre-measured dose of medication when activated. MDIs require coordination between pressing the canister and inhaling the medication, which can be challenging for some patients. Using a spacer or valved holding chamber with MDIs can improve medication delivery and reduce coordination requirements.
Dry Powder Inhalers (DPIs): These inhalers deliver medication in powder form that is activated by the user’s breath. DPIs don’t require coordination between actuation and inhalation, making them easier for some patients to use. However, they require a strong, fast inhalation to properly disperse the powder. Examples of DPIs include Diskus, Turbuhaler, and Twisthaler.
Soft Mist Inhalers (SMIs): These devices release a slow-moving cloud of medication that is easier to inhale than the fast spray from MDIs. The Respimat inhaler is an example of this type, which uses a spring mechanism to create a soft mist without propellants.
Nebulizers: While not technically handheld inhalers, nebulizers are devices that convert liquid medication into a fine mist that can be inhaled through a mask or mouthpiece. They are often used for infants, young children, or during severe asthma attacks when patients have difficulty using handheld inhalers.
Breath-Actuated Inhalers: These are similar to MDIs but are activated by the user’s breath rather than by pressing a canister. This eliminates the need for coordination between actuation and inhalation.
Each type of inhaler device has its advantages and disadvantages, and the choice depends on the patient’s age, ability to use the device correctly, personal preference, and the specific medication prescribed. Healthcare providers work with patients to find the most suitable inhaler device and ensure proper technique through demonstration and practice.
How to Use Asthma Inhalers Correctly
Proper inhaler technique is crucial for effective asthma management. Studies indicate that up to 90% of patients do not use their inhalers correctly, which can lead to poor asthma control and increased risk of exacerbations. The following sections provide detailed instructions on how to use different types of inhalers properly.
Using Metered-Dose Inhalers (MDIs)
Remove the cap and shake the inhaler well for about 5 seconds. If using the inhaler for the first time or if it hasn’t been used for a while, prime it by spraying a test dose into the air. Stand or sit up straight and breathe out fully to empty your lungs. Hold the inhaler upright with your index finger on top and your thumb supporting the bottom. Place the mouthpiece between your teeth and close your lips around it, creating a tight seal. As you begin to breathe in slowly and deeply through your mouth, press down firmly on the canister to release the medication. Continue to breathe in slowly for 3-5 seconds to ensure the medication reaches deep into your lungs. Hold your breath for 10 seconds or as long as comfortable, then breathe out slowly. If a second dose is prescribed, wait about 30 seconds to 1 minute before repeating the process. Replace the cap and clean the mouthpiece regularly according to the manufacturer’s instructions.
Using MDIs with Spacers or Valved Holding Chambers
Spacers or valved holding chambers are recommended for most patients using MDIs, especially children and those who have difficulty coordinating inhalation with actuation. These devices attach to the inhaler and hold the medication in a chamber, allowing the patient to inhale it at their own pace.
Attach the spacer to the mouthpiece of the MDI. Shake the inhaler well. Remove the caps from both the inhaler and spacer. If using a spacer with a mask, place the mask securely over the nose and mouth. If using a mouthpiece, place it between the teeth and close lips around it. Press down on the canister to release one puff of medication into the spacer. Breathe in slowly and deeply through the mouthpiece or mask. If using a spacer without a mask, some spacers make a whistling sound if you’re breathing in too quickly. Hold your breath for 10 seconds or as long as comfortable, then breathe out slowly. If multiple puffs are prescribed, wait about 30 seconds to 1 minute between puffs and repeat the process. After use, detach the spacer from the inhaler and replace the caps. Clean the spacer regularly according to the manufacturer’s instructions.
Using Dry Powder Inhalers (DPIs)
Remove the cap and load the medication according to the specific device instructions. Some DPIs require twisting or clicking to prepare the dose. Stand or sit up straight and breathe out fully away from the device to avoid moisture affecting the powder. Place the mouthpiece between your teeth and close your lips tightly around it. Inhale quickly and deeply through your mouth. The force of your inhalation will pull the powder into your lungs. Remove the inhaler from your mouth and hold your breath for 10 seconds or as long as comfortable. Breathe out slowly away from the inhaler. If multiple doses are prescribed, repeat the process. Close the device according to the manufacturer’s instructions and store it properly.
Using Soft Mist Inhalers (SMIs)
Remove the cap by holding the inhaler upright and twisting in the direction of the arrows. If using the inhaler for the first time, prime it by pointing the inhaler toward the ground and pressing the dose-release button until a cloud of medication is visible. Hold the inhaler upright with the colored side up and the clear side pointing toward your mouth. Breathe out slowly and fully, away from the inhaler. Place the mouthpiece between your teeth and close your lips around it, creating a tight seal. Point the inhaler toward the back of your throat. While taking a slow, deep breath through your mouth, press the dose-release button completely. Continue to breathe in slowly for as long as comfortable. Hold your breath for 10 seconds or as long as comfortable, then breathe out slowly. Close the cap until you hear a click. If a second dose is prescribed, repeat the process after about a minute.
Common Mistakes in Inhaler Technique
Not shaking the inhaler before use. Breathing out into the inhaler before inhaling. Not coordinating inhalation with actuation (for MDIs). Inhaling too quickly or too slowly. Not holding breath long enough after inhalation. Not waiting the recommended time between multiple puffs. Not cleaning the inhaler regularly. Using an empty inhaler without realizing it. Storing the inhaler improperly, exposing it to extreme temperatures or moisture. Not checking the dose counter (if available) to track remaining doses.
Healthcare providers should regularly assess and demonstrate proper inhaler technique during follow-up appointments. Patients are encouraged to demonstrate their technique at each visit to ensure they are using their inhalers correctly. Video tutorials and written instructions can also serve as helpful reminders between appointments.
Side Effects of Asthma Inhalers
While asthma inhalers are generally safe and effective when used as prescribed, like all medications, they can cause side effects. The type and severity of side effects depend on the medication, dosage, frequency of use, and individual patient factors. Understanding potential side effects can help patients recognize and manage them appropriately.
Side Effects of Reliever Inhalers (Short-Acting Bronchodilators)
Reliever inhalers containing short-acting bronchodilators like albuterol are generally well-tolerated, but they can cause:
Common Side Effects: Tremor or shakiness, especially in the hands Increased heart rate (tachycardia) Palpitations or feeling of a racing heart Nervousness or anxiety Headache Dizziness Muscle cramps Dry mouth or throat Irritation or burning sensation in the mouth
Less Common Side Effects: Chest pain or tightness Irregular heart rhythms (arrhythmias) Sleep disturbances or insomnia Changes in taste Nausea or vomiting Sweating Weakness or fatigue
These side effects are usually mild and temporary, resolving within a few hours after use. They tend to be more pronounced with higher doses or frequent use.
Side Effects of Controller Inhalers (Inhaled Corticosteroids)
Controller inhalers containing inhaled corticosteroids (ICS) are the most effective long-term control therapy for asthma. Since they deliver medication directly to the lungs, systemic side effects are minimized compared to oral corticosteroids. However, potential side effects include:
Common Side Effects: Oral thrush (fungal infection in the mouth) Hoarseness or voice changes Sore throat or cough Dry mouth Unpleasant taste
Less Common Side Effects: Nausea or vomiting Headache Dizziness Nosebleeds Difficulty speaking
Rare Side Effects (usually with long-term use at high doses): Suppression of the body’s natural cortisol production Osteoporosis or reduced bone density Cataracts or glaucoma Growth suppression in children Skin thinning and easy bruising Increased risk of infections
The risk of systemic side effects with inhaled corticosteroids is dose-dependent and generally low when used at recommended doses. Using a spacer with MDIs and rinsing the mouth with water after use can significantly reduce the risk of oral thrush and other local side effects.
Side Effects of Combination Inhalers
Combination inhalers contain both an inhaled corticosteroid and a long-acting bronchodilator (LABA). The side effects are generally a combination of those associated with each component:
Common Side Effects: Headache Sore throat Hoarseness Oral thrush Tremor Palpitations Muscle cramps Nausea or vomiting
Less Common Side Effects: Dizziness Anxiety or nervousness Sleep disturbances Chest pain or discomfort Increased heart rate Irregular heart rhythms
Rare Side Effects: Paradoxical bronchospasm (worsening of breathing after inhalation) Allergic reactions Cardiovascular events Ocular effects (cataracts, glaucoma) Bone density reduction
Managing and Minimizing Side Effects
Several strategies can help minimize the side effects of asthma inhalers:
Use the lowest effective dose of medication to maintain asthma control. Always use proper inhaler technique to ensure maximum medication delivery to the lungs and minimal deposition in the mouth and throat. Use a spacer or valved holding chamber with MDIs to improve medication delivery and reduce local side effects. Rinse your mouth with water and spit it out after using inhaled corticosteroids to prevent oral thrush. Clean your inhaler regularly according to the manufacturer’s instructions. Report persistent or bothersome side effects to your healthcare provider, who may adjust your medication or recommend alternative treatments. Do not stop using your controller inhaler without consulting your healthcare provider, as this could lead to worsening asthma control. Monitor children using inhaled corticosteroids for growth and have regular check-ups with their healthcare provider. If you have a history of heart problems, discuss the use of bronchodilators with your healthcare provider, as these medications can affect heart rate and rhythm. Keep a record of your side effects, including when they occur and their severity, to share with your healthcare provider during appointments.
When Side Effects Warrant Medical Attention
While most side effects of asthma inhalers are mild and manageable, some require prompt medical attention:
Seek immediate medical help if you experience: Chest pain or pressure Severe palpitations or irregular heartbeat Severe allergic reactions, including rash, hives, swelling of the face, lips, tongue, or throat, or difficulty breathing Worsening breathing difficulties after using your inhaler (paradoxical bronchospasm) Severe dizziness or fainting Vision changes or eye pain
Contact your healthcare provider if you experience: Persistent oral thrush that doesn’t improve with rinsing your mouth Hoarseness that lasts more than a few weeks Frequent headaches that interfere with daily activities Tremor that makes it difficult to perform daily tasks Significant changes in mood or behavior Unexplained weight gain or swelling Frequent infections Any side effect that concerns you or significantly affects your quality of life
Remember that the benefits of properly controlled asthma generally far outweigh the risks of medication side effects. Work closely with your healthcare provider to find the right balance of effective asthma control with minimal side effects.
When to Seek Medical Help for Asthma
Asthma is a variable condition, and symptoms can change over time. Recognizing when your asthma is worsening or when you’re experiencing a potentially life-threatening asthma attack is crucial for timely intervention and prevention of complications. The following guidelines will help you determine when to seek medical help for your asthma.
Signs of Worsening Asthma
Be alert to these signs that your asthma may be getting worse:
Increasing frequency of symptoms such as wheezing, coughing, chest tightness, or shortness of breath Waking up at night due to asthma symptoms Needing to use your reliever inhaler more frequently than usual (e.g., more than three times per week) Decreased effectiveness of your reliever inhaler Reduced ability to perform normal activities Decreased peak flow readings (if you monitor your peak flow) Increased variability in peak flow readings Increased mucus production, especially if it’s yellow, green, or bloody
If you notice these signs, contact your healthcare provider. They may need to adjust your asthma treatment plan to prevent further worsening of your condition.
Signs of an Asthma Attack Requiring Immediate Action
An asthma attack (also called an exacerbation or flare-up) is a sudden worsening of asthma symptoms. Mild to moderate asthma attacks can often be managed at home with your action plan, but severe attacks require emergency medical attention. Seek immediate medical help if you experience:
Severe shortness of breath at rest Inability to speak in full sentences Straining your chest muscles to breathe (retractions) No improvement after using your reliever inhaler as prescribed in your asthma action plan Peak flow reading less than 50% of your personal best Blue or gray color of the lips, fingernails, or face (cyanosis) Severe anxiety or panic due to breathing difficulties Walking, talking, or other activities become impossible due to shortness of breath Rapid breathing with a respiratory rate greater than 30 breaths per minute Rapid heart rate greater than 120 beats per minute Sweating profusely Feeling confused or drowsy
These signs indicate a severe, potentially life-threatening asthma attack that requires immediate emergency medical treatment. Call emergency services or go to the nearest emergency department.
Managing Asthma Attacks at Home
For mild to moderate asthma attacks, follow your asthma action plan, which typically includes:
Using your reliever inhaler as prescribed (usually 2-4 puffs) If symptoms don’t improve, repeat the reliever inhaler after 20-30 minutes If symptoms persist, contact your healthcare provider or seek medical attention If you have a peak flow meter, monitor your readings and compare them to your personal best Stay calm and try to control your breathing, as panic can worsen symptoms Remove yourself from any known triggers if possible Sit upright in a comfortable position, as lying down can make breathing more difficult
When to Contact Your Healthcare Provider
Contact your healthcare provider if:
Your asthma symptoms are interfering with your daily activities or sleep You’re using your reliever inhaler more than twice a week Your peak flow readings are consistently lower than usual or vary significantly You’re experiencing side effects from your asthma medications You need to refill your reliever inhaler more often than every few months You have been exposed to a known trigger and are experiencing symptoms You have a cold or respiratory infection that is worsening your asthma You’re planning to travel and need to adjust your asthma management plan You’re pregnant or planning to become pregnant and have asthma You have questions about your asthma or its treatment
Regular follow-up appointments with your healthcare provider are essential for good asthma control, even when your symptoms are well-managed. These appointments allow for assessment of your asthma control, adjustment of medications as needed, and review of your inhaler technique.
Creating an Asthma Action Plan
Work with your healthcare provider to develop a personalized asthma action plan. This written plan outlines:
Your daily medications and when to take them How to recognize worsening asthma symptoms What to do when symptoms worsen, including specific medication adjustments When to call your healthcare provider When to seek emergency medical care Your personal best peak flow reading (if you use a peak flow meter)
Keep your asthma action plan readily available and share it with family members, caregivers, and school or work personnel. Review and update your plan regularly with your healthcare provider.
Special Considerations for Children
Children may have difficulty recognizing and communicating their asthma symptoms. Parents and caregivers should watch for:
Increased coughing, especially at night or during activity Wheezing or whistling sounds when breathing Shortness of breath during play or exercise Complaints of chest pain or tightness Fatigue or lack of energy Difficulty feeding in infants Reluctance to participate in physical activities Frequent respiratory infections
Children with asthma may also display behavioral changes when their asthma is worsening, such as irritability, restlessness, or withdrawal from activities. These subtle signs should prompt parents to check the child’s breathing and follow their asthma action plan.
Asthma and Pregnancy
Pregnant women with asthma should be especially vigilant about their symptoms, as uncontrolled asthma can pose risks to both mother and fetus. Contact your healthcare provider if:
Your asthma symptoms worsen during pregnancy You’re using your reliever inhaler more frequently You notice decreased fetal movement You experience any signs of an asthma attack
With proper management, most women with asthma can have healthy pregnancies. It’s important to continue your controller medications as prescribed, as the risks of uncontrolled asthma generally outweigh the risks of asthma medications during pregnancy.
Long-Term Asthma Management
Regular medical follow-up is essential for long-term asthma management, even when symptoms are well-controlled. Schedule appointments with your healthcare provider:
At least every 1-6 months, depending on your asthma severity and control Before making any changes to your medication regimen After an asthma attack or hospitalization Before traveling or starting a new exercise program When you have concerns about your asthma or its treatment
During these appointments, your healthcare provider will assess your asthma control, review your symptoms and medication use, check your inhaler technique, and adjust your treatment plan as needed. They may also recommend lung function tests like spirometry to objectively assess your lung function.
By recognizing when your asthma is worsening and seeking appropriate medical help, you can prevent severe asthma attacks, maintain good asthma control, and enjoy a better quality of life.
Frequently Asked Questions
- What is an asthma inhaler? An asthma inhaler is a handheld medical device that delivers medication directly to the lungs. It’s the primary treatment method for asthma, allowing medication to act quickly on the airways with fewer systemic side effects compared to oral medications.
- How do asthma inhalers work? Asthma inhalers work by converting liquid medication into a fine mist or powder that can be easily inhaled. This direct delivery system ensures that the medication reaches the lungs where it’s needed most, providing either quick relief of symptoms or long-term control of inflammation.
- What are the different types of asthma inhalers? The main types of asthma inhalers are reliever inhalers (for quick relief of symptoms) and controller inhalers (for long-term control). These come in various device types, including metered-dose inhalers (MDIs), dry powder inhalers (DPIs), soft mist inhalers (SMIs), and nebulizers.
- What is the difference between reliever and controller inhalers? Reliever inhalers contain short-acting bronchodilators that quickly relax the muscles around the airways, providing immediate relief of asthma symptoms. Controller inhalers contain anti-inflammatory medications that reduce airway inflammation over time, preventing asthma symptoms and attacks when used regularly.
- How often should I use my reliever inhaler? Reliever inhalers should only be used when needed to relieve asthma symptoms. If you find yourself needing your reliever inhaler more than twice a week, it may indicate that your asthma is not well-controlled, and you should consult your healthcare provider.
- Can I become dependent on my reliever inhaler? No, you cannot become dependent on reliever inhalers in the way people become dependent on certain drugs. However, over-reliance on reliever inhalers may indicate poorly controlled asthma that requires better long-term management with controller medications.
- How do I know if I’m using my inhaler correctly? Proper inhaler technique is crucial for effective treatment. Your healthcare provider should demonstrate the correct technique and have you demonstrate it back during appointments. Signs of incorrect technique include continued symptoms despite medication use or needing to use your reliever inhaler frequently.
- What is a spacer and do I need one? A spacer is a device that attaches to a metered-dose inhaler (MDI) and holds the medication in a chamber, allowing you to inhale it at your own pace. Spacers improve medication delivery to the lungs and are recommended for most people using MDIs, especially children and those who have difficulty coordinating inhalation with actuation.
- How do I clean my inhaler? Cleaning instructions vary by inhaler type. For MDIs, remove the canister and rinse the plastic actuator with warm water at least once a week, then air dry completely. For DPIs, wipe the mouthpiece with a dry cloth. Always follow the manufacturer’s instructions for cleaning your specific inhaler.
- How can I tell if my inhaler is empty? Many inhalers have dose counters that show how many doses remain. If your inhaler doesn’t have a counter, you can track how many doses you’ve used. Alternatively, you can shake the inhaler to feel if there’s still liquid inside, but this method is less reliable.
- Can I use someone else’s inhaler in an emergency? No, you should never use someone else’s inhaler. Asthma medications are prescribed based on individual needs, and using someone else’s inhaler could be ineffective or harmful. Always carry your own prescribed inhaler with you.
- Are there any side effects of asthma inhalers? Like all medications, asthma inhalers can cause side effects. Reliever inhalers may cause tremor, increased heart rate, and nervousness. Controller inhalers may cause oral thrush, hoarseness, and sore throat. Most side effects are mild and can be minimized with proper technique.
- How can I reduce the side effects of my inhaler? To reduce side effects, use the lowest effective dose, maintain proper inhaler technique, use a spacer with MDIs, rinse your mouth after using inhaled corticosteroids, and clean your inhaler regularly. If side effects persist, consult your healthcare provider.
- Can asthma inhalers affect my growth? Studies have shown that high doses of inhaled corticosteroids may cause a small reduction in growth velocity in children. However, this effect is generally minimal (about 1 cm on average) and is outweighed by the benefits of well-controlled asthma. Most children achieve normal adult height.
- Is it safe to use asthma inhalers during pregnancy? Yes, it’s generally safe and important to continue using asthma inhalers during pregnancy. Uncontrolled asthma poses greater risks to both mother and fetus than asthma medications. Always consult your healthcare provider about your asthma management during pregnancy.
- Can I exercise if I use asthma inhalers? Yes, exercise is encouraged for people with asthma. If you experience exercise-induced bronchoconstriction, your healthcare provider may recommend using your reliever inhaler 15-30 minutes before exercise. Regular exercise can actually improve asthma control over time.
- What should I do if my asthma inhaler isn’t working? If your inhaler doesn’t seem to be relieving your symptoms, first check your technique and ensure the inhaler isn’t empty. If technique and medication are not the issue, contact your healthcare provider, as this may indicate worsening asthma that requires treatment adjustment.
- Can I overdose on asthma inhaler medication? While rare, it’s possible to overdose on asthma medication, especially reliever inhalers. Symptoms of overdose may include chest pain, fast or irregular heartbeat, nervousness, headache, tremor, and nausea. If you suspect an overdose, seek immediate medical attention.
- How should I store my inhalers? Store inhalers at room temperature away from direct sunlight, heat, and moisture. Do not store inhalers in bathrooms or cars, as temperature and humidity extremes can affect their performance. Keep inhalers out of reach of children and pets.
- Can I travel with my asthma inhalers? Yes, you can and should travel with your asthma inhalers. Keep them in your carry-on luggage, along with a copy of your prescription. Check airline regulations regarding medical devices, and consider bringing a letter from your healthcare provider if traveling internationally.
- Are generic inhalers as effective as brand-name ones? Yes, generic inhalers contain the same active ingredients as brand-name inhalers and are held to the same standards of quality, safety, and effectiveness. However, the device may be different, so ensure you know how to use the generic inhaler correctly.
- How long does it take for controller inhalers to work? Controller inhalers, particularly those containing inhaled corticosteroids, typically take several days to weeks to reach their full effect. They are not meant for immediate relief and must be used consistently as prescribed to maintain asthma control.
- Can I stop using my controller inhaler if I feel better? No, you should not stop using your controller inhaler without consulting your healthcare provider, even if you feel better. Controller medications work by reducing underlying inflammation, and stopping them can lead to worsening asthma and increased risk of attacks.
- What is the difference between an MDI and a DPI? A metered-dose inhaler (MDI) releases a pre-measured spray of medication when activated, requiring coordination between pressing the canister and inhaling. A dry powder inhaler (DPI) delivers medication in powder form that is activated by the user’s breath, requiring a strong, fast inhalation.
- Can children use asthma inhalers? Yes, children can use asthma inhalers. Young children often use MDIs with spacers and masks to ensure proper medication delivery. The type of inhaler and technique should be appropriate for the child’s age and ability.
- Are there alternatives to inhalers for asthma treatment? While inhalers are the primary treatment for asthma, there are alternative medications like leukotriene modifiers and biologics for severe asthma. However, most alternatives are oral medications that may have more systemic side effects than inhaled medications.
- Can I use my inhaler if I have a cold or respiratory infection? Yes, you should continue using your inhalers as prescribed when you have a cold or respiratory infection. In fact, respiratory infections can trigger asthma symptoms, so maintaining your medication regimen is important. Contact your healthcare provider if symptoms worsen.
- How often should I replace my inhalers? Replace your inhalers when they’re empty or past their expiration date. Even if there’s medication left, inhalers may not deliver the correct dose after the expiration date. Some MDIs should be replaced after a certain number of doses or time, even if they still contain medication.
- Can asthma inhalers interact with other medications? Asthma inhalers can interact with other medications, particularly beta-blockers, which can interfere with bronchodilators. Always inform all your healthcare providers about all medications you take, including over-the-counter drugs and supplements, to check for potential interactions.
- How can I remember to use my controller inhaler regularly? To remember to use your controller inhaler, try incorporating it into your daily routine, such as brushing your teeth. Set reminders on your phone or use a pill organizer. Keep your inhaler in a visible place as a reminder, and track your use on a calendar or app.
Conclusion
Asthma inhalers are essential tools in the management of asthma, providing both quick relief of symptoms and long-term control of inflammation. Understanding the different types of inhalers, their proper use, potential side effects, and when to seek medical help is crucial for effective asthma management.
Proper inhaler technique is fundamental to ensuring that medication reaches the lungs where it’s needed most. Regular review of technique with healthcare providers, use of spacers or valved holding chambers when appropriate, and following manufacturer instructions for cleaning and maintenance can significantly improve treatment outcomes.
While side effects from asthma inhalers are generally mild and manageable, it’s important to be aware of potential adverse effects and know when to seek medical attention. The benefits of well-controlled asthma typically far outweigh the risks of medication side effects when inhalers are used as prescribed.
Recognizing the signs of worsening asthma and knowing when to seek medical help can prevent severe asthma attacks and hospitalizations. Having a personalized asthma action plan developed with your healthcare provider is an important step in managing your condition effectively.
By staying informed about your asthma and its treatment, using your inhalers correctly, and maintaining regular communication with your healthcare provider, you can achieve good asthma control and enjoy a full, active life. Remember that asthma is a chronic condition that requires ongoing management, but with the right approach and proper use of inhalers, most people with asthma can lead normal, unrestricted lives.
Natural Alternatives to Asthma Inhalers: What Works?