Navigating the World of Fungal Infections: A Comprehensive Guide
In our daily lives, we are constantly surrounded by a microscopic world teeming with life. Among these organisms are fungi—a vast kingdom that includes everything from the yeast that makes our bread rise to the mushrooms in a forest. While the vast majority of fungi are harmless or even beneficial, a small fraction can cause infections when they find a suitable environment to grow on or inside our bodies. These conditions, known as fungal infections or mycoses, are incredibly common, affecting millions of people worldwide every year.
In this article, we will embark on an informational journey to understand what fungal infections are, explore their various types, uncover their root causes, and learn to recognize their symptoms. Most importantly, we will discuss the effective treatments and preventative measures available to help us manage and avoid these persistent ailments.
What Exactly Is a Fungal Infection?
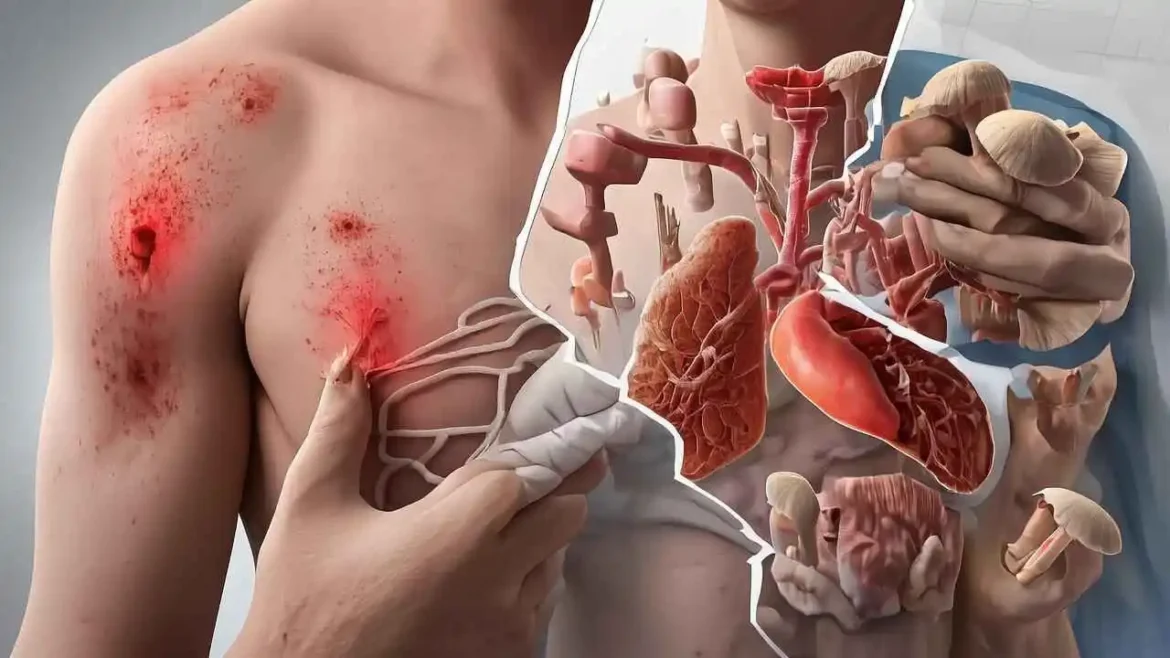
A fungal infection, also known as mycosis, is a disease caused by the overgrowth of a fungus in or on the body. These infections can range from superficial, affecting only the skin, hair, and nails, to deep and systemic, affecting internal organs like the lungs and entering the bloodstream.
Fungi thrive in warm, moist environments, which is why areas of the body like the feet, groin, and skin folds are common sites for infection. They reproduce by releasing spores, which can be picked up through direct contact, inhaled, or land on the skin. For most people with healthy immune systems, an encounter with a pathogenic fungus might not lead to any issues. However, if the skin is broken, the immune system is compromised, or the conditions are just right for fungal growth, an infection can take hold.
There are various types of fungal infections, such as athlete’s foot, ringworm, and yeast infections. Some are more severe and can lead to life-threatening complications, particularly in people with weakened immune systems. Treatment for fungal infections depends on the type and severity of the infection, but may include antifungal medications, creams, or ointments.
Preventing fungal infections involves maintaining good hygiene, keeping skin clean and dry, avoiding contact with infected individuals or contaminated surfaces, and wearing breathable clothing and footwear. Additionally, it is essential to manage any underlying medical conditions that may weaken the immune system, such as diabetes or HIV/AIDS.
Fungal infections are a diverse group of diseases that can affect various parts of the body. While some are relatively harmless, others can lead to severe complications. Prevention and early detection are crucial in managing these infections and maintaining overall health.
The Diverse and Pervasive World of Fungal Infections (Mycoses)
Fungal infections, medically known as mycoses, represent a broad category of diseases caused by various species of fungi. Unlike bacteria or viruses, fungi are eukaryotic organisms, meaning their cells have a nucleus and other membrane-bound organelles, placing them in a kingdom distinct from plants and animals. They thrive in warm, moist environments and can be found in soil, plants, air, and even on our skin.
While several hundred types of fungi can cause infections in humans, they are fundamentally categorized based on the depth of tissue invasion and the part of the body they affect. This classification helps in understanding their clinical presentation, severity, and treatment approaches. The most frequently encountered infections are localized and superficial, often causing discomfort but rarely life-threatening. However, it’s crucial to be aware of the more serious, systemic forms that can pose significant health risks, especially to vulnerable populations.
Fungi can gain entry to the body through various means: direct contact with an infected person or animal, contact with contaminated surfaces (e.g., locker room floors), inhalation of fungal spores from the environment, or even through a break in the skin. Risk factors for developing fungal infections can include a weakened immune system, prolonged use of antibiotics or corticosteroids, diabetes, obesity, excessive sweating, and poor hygiene.
Types
I. Superficial and Cutaneous Fungal Infections
These are the most common types of fungal infections, primarily affecting the outermost layers of the skin (epidermis), hair, nails, and mucous membranes. They are generally not invasive and rarely spread internally. Many of these are caused by a group of fungi called dermatophytes, which specifically feed on keratin, the protein found in skin, hair, and nails. Other common culprits include various species of yeast, such as Candida and Malassezia.
| Infection Name (Medical Term) | Common Name | Causative Agent(s) | Affected Area(s) | Typical Symptoms |
| Tinea Pedis | Athlete’s Foot | Trichophyton rubrum, T. mentagrophytes, Epidermophyton floccosum | Feet, especially between the toes, soles, sides of feet | Intense itching, stinging, burning sensation, cracked or peeling skin, redness, blistering, scaling. Can be chronic and recurrent. |
| Tinea Corporis | Ringworm of the Body | Trichophyton, Microsporum, Epidermophyton species | Torso, arms, legs, face (non-hairy areas) | A characteristic circular, red, scaly rash with a raised, often blistering border and a clearer center, giving it a “ring-like” appearance (hence “ringworm,” though no worm is involved). Itching is common. |
| Tinea Cruris | Jock Itch | Trichophyton rubrum, T. mentagrophytes, Epidermophyton floccosum | Groin, inner thighs, buttocks | A red, intensely itchy rash, often ring-shaped or crescent-shaped, with raised borders. Can cause chafing, burning sensation, and discoloration of the skin. Exacerbated by warmth, moisture, and tight clothing. |
| Tinea Unguium (Onychomycosis) | Nail Fungus | Trichophyton rubrum (most common), T. mentagrophytes, Candida species | Fingernails or toenails (more common in toenails) | Nails become thickened, brittle, crumbly, and discolored (yellow, brown, white, or black). The nail may separate from the nail bed (onycholysis) and develop an irregular, distorted shape. Can be painful. |
| Candidiasis (Cutaneous) | Skin Yeast Infection | Candida albicans (most common), other Candida species | Skin folds (armpits, under breasts, groin, buttocks, between fingers/toes), navel, under fingernails | A red, itchy, often moist rash, sometimes with small, satellite pustules or pimple-like bumps at the edges. Common in warm, moist, and macerated areas. Often associated with diabetes, obesity, and antibiotic use. |
| Candidiasis (Oral) | Oral Thrush | Candida albicans | Mouth, tongue, inner cheeks, throat, gums, tonsils | Creamy white lesions or patches on the tongue or inner cheeks that can be scraped off to reveal underlying redness. May cause soreness, redness, burning sensation, difficulty swallowing, or a cottony feeling in the mouth. Common in infants, denture wearers, immunocompromised individuals, and those on antibiotics or corticosteroids. |
| Tinea Versicolor (Pityriasis Versicolor) | Sun Fungus | Malassezia globosa, Malassezia furfur (yeast-like fungi) | Back, chest, neck, upper arms, abdomen | Characterized by small, discolored patches on the skin that can be lighter (hypopigmented) or darker (hyperpigmented) than the surrounding skin. The patches may or may not itch and often become more noticeable after sun exposure as they do not tan. |
General Treatment for Superficial/Cutaneous Infections: Treatment typically involves topical antifungal creams, sprays, powders, or shampoos. Oral antifungal medications may be prescribed for more extensive or stubborn infections (like nail fungus or severe ringworm) due to their systemic action. Good hygiene, keeping affected areas dry, and wearing breathable materials are crucial for prevention and recovery.
II. Subcutaneous Fungal Infections
These infections are less common than superficial ones and occur when fungi penetrate the skin, usually through trauma (e.g., a thorn prick), and infect the deeper layers of the skin, subcutaneous tissue, and sometimes bone. They are generally localized but can be chronic and require more aggressive treatment. Examples include Sporotrichosis (Rose Gardener’s Disease), Chromoblastomycosis, and Mycetoma.
III. Systemic Fungal Infections
Systemic fungal infections are the most serious forms, as they affect internal organs, often starting in the lungs after inhaling fungal spores from the environment, and then spreading throughout the body via the bloodstream. These infections can be life-threatening and primarily pose a significant threat to individuals with weakened immune systems, though some can cause severe disease in otherwise healthy people.
- Aspergillosis: Caused by species of Aspergillus (e.g., Aspergillus fumigatus), which are common molds found indoors and outdoors.
- Affected Areas: Primarily lungs, but can affect sinuses, brain, kidneys, and skin.
- Forms: Can manifest as allergic reactions (allergic bronchopulmonary aspergillosis), localized fungal balls in lung cavities (aspergilloma), or invasive aspergillosis (a severe, rapidly progressing infection in immunocompromised individuals).
- Risk Factors: Immunosuppression (e.g., organ transplant recipients, chemotherapy patients), chronic lung diseases (e.g., COPD, tuberculosis).
- Histoplasmosis: Caused by Histoplasma capsulatum, a fungus found in soil, especially those enriched with bird or bat droppings.
- Affected Areas: Lungs (primary site of infection), but can disseminate to the brain, liver, spleen, lymph nodes, and bone marrow.
- Symptoms: Often asymptomatic or flu-like (fever, cough, fatigue). In severe cases, it can cause chronic lung disease or widespread systemic infection, particularly in those with compromised immunity.
- Geographic Relevance: Endemic in certain regions, notably the Ohio and Mississippi River valleys in the United States.
- Cryptococcosis: Caused by Cryptococcus neoformans (associated with bird droppings, especially pigeons) and Cryptococcus gattii (found in trees).
- Affected Areas: Primarily lungs and central nervous system (brain and spinal cord), causing meningitis (inflammation of the membranes surrounding the brain and spinal cord). Can also affect skin, bones, and other organs.
- Symptoms: In the lungs, can cause cough, shortness of breath. In the CNS, symptoms include headache, fever, neck stiffness, confusion, and vision changes.
- Risk Factors: Most common in individuals with severely weakened immune systems (e.g., HIV/AIDS patients, organ transplant recipients).
General Treatment for Systemic Infections: Treatment for systemic fungal infections is complex and typically involves powerful oral or intravenous antifungal medications (e.g., amphotericin B, azoles like fluconazole, voriconazole). Treatment courses can be prolonged (weeks to months or even years) and often require careful monitoring for side effects.
Accurate and timely diagnosis of fungal infections is paramount for effective treatment and preventing the spread or progression of the disease. Given the diverse nature of fungi and their varied manifestations, diagnosis often necessitates a comprehensive approach, combining various laboratory and imaging techniques:
Diagnosis of Fungal Infections: