- Microscopic examination: This is often the first line of investigation for superficial fungal infections. Samples such as skin scrapings, nail clippings, or hair follicles are treated with potassium hydroxide (KOH), which dissolves keratin and cellular debris, making it easier to visualize fungal elements like hyphae (thread-like structures) or spores under a microscope. This method provides a rapid, albeit preliminary, indication of a fungal presence.
- Fungal cultures: While microscopic examination provides a quick result, fungal cultures are essential for definitive identification of the specific fungal species. Clinical samples (which can include skin, nail, hair, blood, cerebrospinal fluid, or tissue) are inoculated onto specialized culture media (e.g., Sabouraud Dextrose Agar) that support fungal growth. Although this method provides a precise diagnosis, it can be time-consuming, often taking days to weeks for certain fungi to grow.
- Biopsy: In cases of deeper tissue involvement, chronic infections, or suspected systemic mycoses, a tissue biopsy may be performed. The tissue sample is then processed for histopathological examination, where pathologists look for characteristic fungal structures within the tissue. The biopsy specimen can also be sent for fungal culture and molecular testing for more comprehensive identification.
- Blood tests: For suspected systemic or invasive fungal infections, blood tests play a crucial role. These tests can detect:
- Fungal Antigens: Molecules specific to the fungus (e.g., galactomannan for Aspergillus, cryptococcal antigen for Cryptococcus, beta-D-glucan for various invasive fungi), indicating active infection.
- Antibodies: The body’s immune response to a fungal infection.
- Molecular Tests (PCR): Polymerase Chain Reaction (PCR) tests can detect fungal DNA directly in blood or other body fluids, offering high sensitivity and specificity, especially for hard-to-culture fungi.
- Imaging: Imaging studies are indispensable for assessing the extent of systemic fungal infections and localizing affected organs.
- X-rays: Often used for initial evaluation of lung involvement.
- CT Scans (Computed Tomography): Provide detailed cross-sectional images, excellent for detecting fungal lesions in the lungs, sinuses, and abdomen.
- MRIs (Magnetic Resonance Imaging): Offer superior soft tissue contrast, particularly useful for brain, spinal cord, or deep tissue involvement. These scans help identify characteristic patterns of infection, monitor disease progression, and guide therapeutic interventions.
Prevention Strategies for Fungal Infections:
Preventative measures are crucial in reducing the incidence and spread of fungal infections, ranging from simple hygiene practices to more targeted interventions:
- Good hygiene: Maintaining scrupulous personal hygiene is fundamental. This includes regular washing with soap and water, followed by thorough drying of the entire body, paying particular attention to skin folds (groin, armpits, under breasts, between toes) where moisture can accumulate and create a conducive environment for fungal growth. Promptly changing out of wet clothing or swimsuits is also advised.
- Appropriate footwear: To prevent common conditions like athlete’s foot (tinea pedis) and nail infections, wear shoes made of breathable materials (e.g., leather, canvas) to allow air circulation. Change socks daily, opting for moisture-wicking materials (cotton blend, synthetic fibers). Avoid walking barefoot in public areas like locker rooms, communal showers, and swimming pool decks.
- Avoiding sharing: Fungi can easily spread through direct contact with contaminated items. Therefore, it is crucial to avoid sharing personal belongings such as towels, shoes, socks, hats, hairbrushes, and clothing. This simple measure significantly reduces the risk of transmission.
- Protective gear: When engaging in activities that involve contact with soil, especially in regions where certain fungi are endemic (e.g., Histoplasma, Coccidioides, Sporothrix), wearing protective gear is vital. This includes gloves for gardening or landscaping, and potentially N95 masks when disturbing soil or dust in high-risk environments, to prevent inhalation of fungal spores.
- Immune system support: Individuals with weakened immune systems (e.g., due to HIV/AIDS, cancer chemotherapy, organ transplantation, diabetes, or long-term corticosteroid use) are at a significantly higher risk for severe and invasive fungal infections. For this vulnerable population, adherence to medical advice regarding underlying conditions, nutritional support, and as prescribed by a physician, prophylactic antifungal medications are critical to prevent opportunistic fungal infections.
A comprehensive understanding of fungal infections – from their diverse causes and symptoms to their specific risk factors – forms the cornerstone of effective management. The combined approach of advanced diagnostic techniques and diligent preventative strategies is essential not only for successful treatment but also for mitigating the burden of these infections, improving patient outcomes, and promoting overall public health.
What Are the Primary Causes and Risk Factors?
Recognizing the Symptoms and Seeking Diagnosis
Fungal infections, also known as mycoses, are not random occurrences. They arise from a confluence of factors, primarily involving exposure to fungal spores or organisms coupled with environmental and physiological conditions that facilitate their proliferation within the host. These opportunistic pathogens are ubiquitous in our environment, but an infection only takes hold when the right circumstances align. Understanding these primary causes and risk factors is crucial for prevention and effective management.
Here are the primary factors that can lead to a fungal infection:
- Weakened Immune System: A compromised or weakened immune system stands as the single most critical risk factor, dramatically increasing susceptibility to both superficial and deeply invasive fungal infections. The immune system acts as the body’s primary defense, identifying and eliminating foreign invaders like fungi. When this defense is impaired, fungi can establish themselves and spread more easily. Beyond the mentioned groups—individuals with HIV/AIDS, cancer patients undergoing chemotherapy, and organ transplant recipients on immunosuppressants—other vulnerable populations include those with uncontrolled diabetes, the very young, the elderly, and people with certain genetic immunodeficiencies. For these individuals, what might be a minor skin rash in a healthy person could escalate into a life-threatening systemic infection.
- Antibiotic Use: While invaluable for combating bacterial illnesses, broad-spectrum antibiotics can inadvertently disrupt the body’s delicate microbial balance, particularly in the gut and on mucous membranes. These medications not only target harmful bacteria but also indiscriminately eliminate beneficial bacteria (part of our natural microbiome) that normally compete with fungi for resources and space. Without the regulatory presence of these ‘good’ bacteria, opportunistic fungi, most notably Candida albicans, can proliferate unchecked. This imbalance often leads to common issues like oral thrush, vaginal yeast infections, or even skin folds infections, as the fungal population experiences an uncontrolled overgrowth.
- Poor Hygiene or Excessive Moisture: Fungi thrive in warm, dark, and especially moist environments. Persistent dampness provides the ideal conditions for fungal spores to germinate and grow, transforming the skin’s surface into a fertile breeding ground. Habits such as not thoroughly drying the feet after showering, wearing damp or sweaty clothing for extended periods (e.g., after exercise), or neglecting general personal hygiene significantly contribute to this problem. Areas prone to moisture accumulation, like between the toes, in skin folds (e.g., groin, armpits, under breasts), and under tight clothing, are particularly susceptible to infections such as athlete’s foot (tinea pedis), jock itch (tinea cruris), and ringworm.
- Direct Contact: Many common fungal infections are highly contagious and can be readily transmitted through direct physical contact. This includes skin-to-skin contact with an infected individual, such as through close personal interaction or participating in contact sports. Additionally, fungi can spread from infected animals (like pets such as cats or dogs, or livestock) to humans, leading to conditions like ringworm (tinea corporis). This direct transfer allows fungal spores to establish themselves on new hosts, particularly when there are minor skin breaks or a moist environment present.
- Indirect Contact: Beyond direct person-to-person or animal-to-person spread, fungal spores are remarkably resilient and can survive for extended periods on various inanimate objects and surfaces, known as fomites. Indirect contact occurs when an individual touches a contaminated item and then touches their own skin, allowing the spores to transfer. Common culprits include shared towels, bedding, combs, brushes, clothing, and footwear. Public environments like locker room floors, communal showers, swimming pool decks, and gym equipment are notorious for harboring fungal spores, making it easy to pick up infections if proper precautions (like wearing flip-flops) are not taken.
- Environmental Exposure: Certain types of fungi are naturally abundant in specific environmental reservoirs, and exposure often occurs through the inhalation of microscopic spores. These fungi commonly reside in soil, decaying organic matter (like leaf litter), and animal droppings (especially from birds or bats). Examples include Histoplasma capsulatum (found in the Ohio and Mississippi River valleys), Coccidioides immitis (in the arid southwestern United States), and Blastomyces dermatitidis (in the southeastern and midwestern US). Activities that disturb soil or contaminated areas, such as gardening, farming, construction, excavation, or exploring caves, can aerosolize these spores. Once inhaled, these spores can lead to respiratory infections, which, while often asymptomatic or flu-like in healthy individuals, can disseminate and cause severe, systemic disease in those with compromised immune systems.
Symptoms vary widely depending on the type and location of the infection. However, there are common signs to watch for:
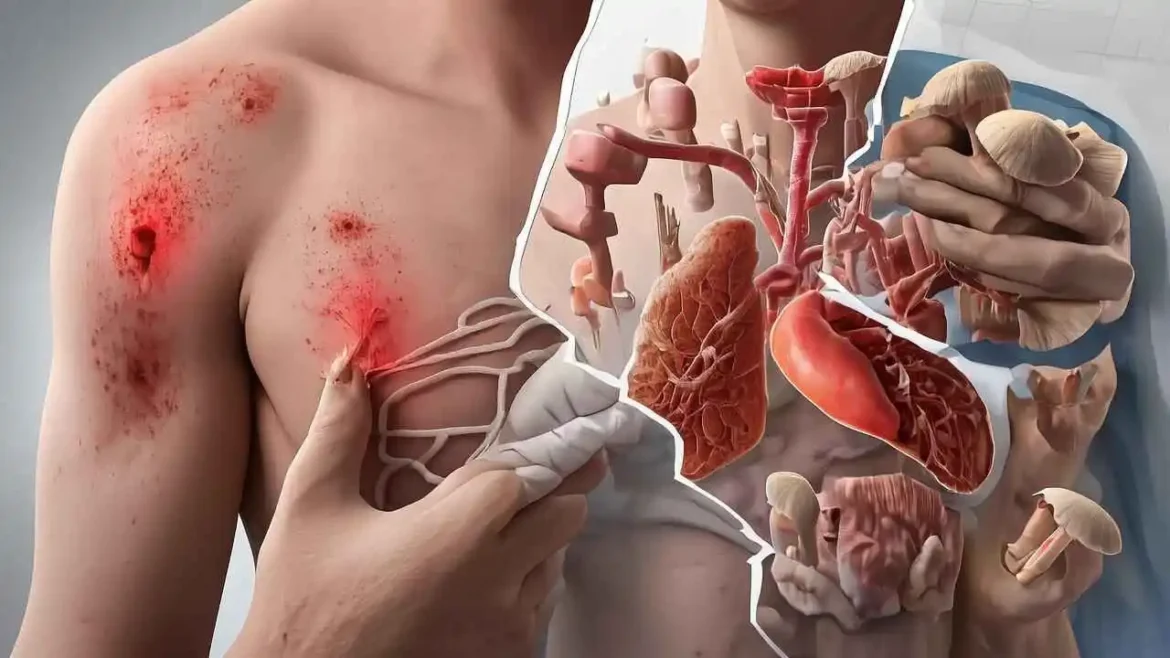
Fungal infections, while common, can manifest with a wide range of symptoms, profoundly influenced by the specific type of fungus involved and its location on or within the body. From superficial skin conditions to more serious systemic diseases, recognizing the key indicators is crucial for timely diagnosis and effective treatment. While the exact presentation can differ, several common signs serve as important alerts that warrant attention:
For Superficial Fungal Infections (Skin, Nail, and Hair):
These infections, often referred to as dermatophytoses (like ringworm, athlete’s foot, or jock itch) or onychomycosis (nail fungus), primarily involve localized irritation and visible changes:
- Persistent itching, stinging, or burning: This is a hallmark symptom, often intense and relentless, caused by the fungal organisms irritating nerve endings in the skin.
- Redness and inflammation: The affected area often becomes noticeably red and swollen, indicating the body’s immune response to the infection.
- Scaling, peeling, or cracking skin: The skin may appear dry, flaky, or scaly, and in severe cases, it can crack, leading to pain and potential entry points for bacterial infections.
- A rash, especially one that is circular or has defined borders: Common in ringworm (tinea corporis), these rashes often present as a red, itchy, scaly patch with raised borders and a clearer center, resembling a ring.
- Thick, discolored, or brittle nails: Nails, particularly toenails, may become thickened, crumbly, and discolored (yellow, brown, white, or opaque). They might also separate from the nail bed. This condition is known as onychomycosis.
- Hair loss in patches: When the scalp is affected (tinea capitis), the fungus can cause hair to become brittle and break off, leading to distinct patches of hair loss, sometimes with visible scaling or black dots (broken hairs).
For Mucosal or Systemic Fungal Infections:
More serious fungal infections can affect mucous membranes (like the mouth or vagina) or spread systemically throughout the body, particularly in individuals with weakened immune systems or those on certain medications. These infections often present with different, and sometimes more generalized, symptoms:
- White patches inside the mouth (thrush): Caused by an overgrowth of Candida albicans, these creamy white, cottage cheese-like lesions can appear on the tongue, inner cheeks, roof of the mouth, or throat. They may be painful and bleed slightly when scraped.
- Vaginal itching, burning, and discharge (yeast infection): Another common Candida infection, symptoms include intense vaginal itching and burning, soreness, redness, and a thick, white, cottage cheese-like discharge. Pain during urination or intercourse may also occur.
- Fever and chills: These are systemic signs indicating that the body is fighting a more widespread infection, common in many types of systemic fungal diseases.
- Headache and muscle aches: Generalized body aches and headaches can accompany systemic fungal infections, similar to symptoms of the flu.
- Cough or shortness of breath: If the fungal infection affects the lungs (e.g., fungal pneumonia), symptoms can include a persistent cough, shortness of breath, chest pain, and fatigue.
When to Consult a Healthcare Provider and How Diagnosis is Made:
Given the varied presentation of fungal infections and the importance of accurate diagnosis, it is highly recommended to consult a healthcare provider promptly if you suspect you might have one. Early intervention can prevent the spread of the infection, alleviate discomfort, and prevent potential complications.
A general practitioner, dermatologist, or other specialist can typically diagnose superficial infections through a thorough physical examination, observing the characteristic appearance of the affected area. For definitive confirmation, especially in cases where symptoms are atypical, or for more severe or persistent infections, your doctor may perform diagnostic tests. These often include taking a small skin scraping, nail clipping, or a swab of the affected area. This sample can then be:
- Examined under a microscope (e.g., KOH prep): This rapid method involves treating the sample with potassium hydroxide to dissolve skin cells, allowing for clearer and direct visualization of fungal elements (hyphae, spores) under the microscope.
- Sent for a lab culture: This involves growing the fungus in a specialized medium over several days or weeks. A lab culture is more definitive as it helps in identifying the specific species of fungus, which is crucial for guiding the most effective antifungal treatment.
For suspected systemic fungal infections, additional diagnostic tests such as blood tests, imaging (like X-rays or CT scans), or biopsies may be necessary. Accurate diagnosis ensures you receive the appropriate antifungal medication and prevents unnecessary use of other treatments, leading to better outcomes and faster recovery.
Effective Treatment and Prevention Strategies for Fungal Infections
Fungal infections, while often annoying and persistent, are fortunately treatable in the vast majority of cases. The specific course of action required depends significantly on several factors, including the type of fungus involved, the location of the infection, its severity, and the overall health of the affected individual. Early diagnosis and intervention are key to preventing more widespread or complicated issues.
Comprehensive Treatment Approaches:
Various therapeutic options are available, ranging from topical applications for superficial issues to systemic medications for more entrenched or severe conditions.
- Topical Antifungals: The First Line of Defense For most localized and superficial skin infections, such as common conditions like athlete’s foot (tinea pedis), ringworm (tinea corporis), jock itch (tinea cruris), and certain types of yeast infections (like candidiasis affecting skin folds), topical antifungals are the primary treatment. These come in various forms, including:
- Creams and Ointments: Provide direct contact and often have moisturizing properties.
- Gels: Can be less greasy and dry more quickly.
- Powders: Help to keep areas dry, inhibiting fungal growth, especially in skin folds.
- Medicated Shampoos: Used for scalp conditions like tinea capitis (though often requiring oral antifungals for full eradication).
- Sprays: Convenient for larger areas or hard-to-reach spots.
These products contain antifungal agents like miconazole, clotrimazole, terbinafine, or ketoconazole, which work by disrupting the fungal cell wall or inhibiting fungal growth. They are applied directly to the affected area, usually once or twice daily, for a period that often extends beyond the disappearance of symptoms to ensure complete eradication (typically 2-4 weeks). Adherence to the full treatment course is crucial to prevent recurrence.
- Oral Antifungals: For Deeper or Widespread Infections When topical treatments prove insufficient, or for infections that are more widespread, deeper, or located in areas where topicals cannot penetrate effectively (such as nails or hair follicles), a healthcare professional may prescribe oral antifungal medications. These pills work systemically, meaning they are absorbed into the bloodstream and travel throughout the body to eliminate the fungus from the inside out. Common conditions requiring oral antifungals include:
- Onychomycosis (Nail Fungus): Fungi within the nail bed are particularly difficult to reach with topical agents.
- Tinea Capitis (Scalp Ringworm): The fungus infects hair follicles, necessitating systemic treatment.
- Extensive Skin Infections: When large areas of the body are affected or the infection is recurrent.
- Internal Candidiasis: For yeast infections affecting the mouth (thrush), esophagus, or vagina that are stubborn or recurrent.
Examples of oral antifungals include fluconazole, itraconazole, terbinafine, and griseofulvin. Treatment durations can vary significantly, from a single dose for some yeast infections to several months for nail fungus. Due to potential side effects like liver enzyme elevation or drug interactions, oral antifungals require a doctor’s prescription and may necessitate monitoring through blood tests.
- Intravenous (IV) Antifungals: Critical Care for Systemic Infections In rare but severe cases, especially in individuals with compromised immune systems (e.g., HIV/AIDS patients, transplant recipients, chemotherapy patients), fungal infections can become systemic. This means the fungus spreads throughout the body, affecting internal organs and potentially leading to life-threatening conditions like candidemia (fungus in the bloodstream), aspergillosis, or cryptococcosis. For these critical situations, potent antifungal drugs are administered directly into the bloodstream via an intravenous (IV) drip in a hospital setting. These medications, such as amphotericin B (often referred to as “ampho-terrible” due to its potential side effects but highly effective), echinocandins (e.g., micafungin, caspofungin), and certain high-dose azoles, are powerful and fast-acting, aimed at rapidly controlling and eliminating the widespread infection to save the patient’s life. This level of treatment is intensive and requires close medical supervision.
Prevention: The Best Medicine
While effective treatments exist, preventing fungal infections is undeniably the most effective and often overlooked strategy. By adopting a few simple yet crucial habits, individuals can significantly reduce their risk of developing these common and sometimes persistent ailments:
- Practice Good Hygiene: Regular bathing or showering with mild soap helps remove fungal spores, sweat, and oils that contribute to fungal growth. Pay particular attention to cleaning skin folds, the groin area, under the breasts, and between the toes. Thorough handwashing is also essential to prevent the spread of fungal spores.
- Keep Your Skin Dry: Fungi thrive in warm, moist environments. After bathing, showering, or swimming, thoroughly pat your skin dry with a clean towel, especially in skin folds, the groin area, under the arms, and between your toes. Consider using absorbent powders (like cornstarch or talcum powder) in areas prone to excessive moisture.
- Wear Breathable Fabrics: Opt for natural, breathable materials like cotton for underwear, socks, and clothing. These materials allow air to circulate, reducing moisture buildup and creating a less hospitable environment for fungal growth. Promptly change out of damp or sweaty clothes (e.g., after exercise) as moisture creates an ideal breeding ground.
- Protect Your Feet: Public spaces like showers, locker rooms, gym floors, and pool areas are prime breeding grounds for fungal spores. Always wear waterproof footwear, such as flip-flops or shower sandals, in these environments to prevent direct contact with contaminated surfaces. Change your socks daily, and consider moisture-wicking synthetic socks if your feet sweat excessively. Rotate your shoes to allow them to fully dry out between uses.
- Don’t Share Personal Items: Fungal spores can easily transfer through direct contact with infected skin cells or contaminated items. Avoid sharing towels, combs, brushes, hats, clothing, shoes, or razors with others, as these can harbor and transmit fungal elements.
- Support Your Immune System: A robust immune system is your body’s frontline defense against opportunistic infections, including fungi. Maintain a healthy lifestyle through a balanced diet rich in fruits, vegetables, and lean proteins, engage in regular physical activity, and ensure you get adequate, quality sleep. Managing stress also plays a vital role in supporting immune function. Individuals with weakened immune systems due to underlying health conditions (e.g., diabetes, HIV) or medications (e.g., corticosteroids, immunosuppressants) should be particularly vigilant with preventive measures.
By understanding both the available treatment options and, crucially, by diligently practicing preventive habits, individuals can effectively manage and significantly reduce the impact of fungal infections on their health and well-being. If you suspect a fungal infection, always consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
In conclusion, while the thought of a fungal infection can be unpleasant, it’s a common part of human health that we can effectively navigate. By understanding their causes, recognizing their symptoms, and embracing preventative hygiene, we empower ourselves to keep these microscopic invaders at bay. If an infection does occur, rest assured that a wide range of effective treatments is available to restore our skin and bodies to a healthy state.
FAQs on Preventing Fungal Infections by Natural Remedies and Lifestyle Changes
- What are fungal infections?
- Fungal infections are caused by fungi that can affect the skin, nails, and internal organs. Common types include athlete’s foot, ringworm, and thrush.
- How can I prevent fungal infections naturally?
- Focus on maintaining good hygiene, keeping skin dry, and using natural antifungal remedies such as tea tree oil and garlic.
- What lifestyle changes can help prevent fungal infections?
- Regularly showering, wearing breathable clothing, and avoiding tight footwear can reduce moisture and prevent infection.
- Is garlic effective against fungal infections?
- Yes, garlic has antifungal properties and can be consumed or applied topically to affected areas.
- Which natural remedies are most effective against fungal infections?
- Tea tree oil, apple cider vinegar, and coconut oil are commonly recommended antifungal remedies.
- Can diet play a role in preventing fungal infections?
- Yes, a diet low in sugar and refined carbohydrates can help prevent fungal growth.
- What types of foods should I include in my diet?
- Include foods rich in probiotics, such as yogurt and sauerkraut, to support gut health and boost immunity.
- How does sugar consumption affect fungal infections?
- Sugar can promote fungal growth; reducing sugar intake can help lower the risk of infection.
- Are there specific conditions that make people more susceptible to fungal infections?
- Yes, individuals with weakened immune systems, diabetes, or skin conditions are at higher risk.
- Is it important to dry my skin thoroughly after showering?
- Yes, keeping skin dry prevents the growth of fungi that thrive in moist environments.
- Can I use essential oils to prevent fungal infections?
- Yes, essential oils like eucalyptus, lavender, and oregano oil can be used for their antifungal properties.
- What precautionary measures should I take in communal places?
- Wear flip-flops in communal showers or pools and avoid sharing towels to minimize risk.
- How often should I change my socks and underwear?
- Change them daily or more frequently if they become sweaty to keep your skin dry.
- Is sweating a concern for fungal infections?
- Yes, excessive sweating can create a hospitable environment for fungi, so use breathable fabrics.
- Should I avoid certain types of clothing?
- Tight-fitting and non-breathable fabrics can trap moisture and promote fungal infections; opt for cotton or moisture-wicking materials.
- Can I use aloe vera for fungal infections?
- Yes, aloe vera has soothing and antifungal properties and can be applied topically.
- Is it safe to use over-the-counter antifungal creams?
- Yes, but it’s recommended to consult with a healthcare provider before using any medication.
- How can I manage stress to prevent fungal infections?
- Regular exercise, meditation, and other stress-relief techniques can strengthen the immune system.
- Is hydration important in preventing fungal infections?
- Yes, proper hydration supports overall health and can help your body fight infections.
- Can pets contribute to fungal infections?
- Yes, some fungi can be transmitted from pets to humans, so maintaining pet hygiene is important.
- Are there home remedies for treating toenail fungus?
- Soaking the affected foot in apple cider vinegar may help, along with regular application of tea tree oil.
- Should I consult a doctor if I suspect a fungal infection?
- Yes, a healthcare provider can offer the best course of treatment and advice tailored to your situation.
- How important is foot care in preventing fungal infections?
- Very important; keeping feet clean and dry is crucial for prevention, especially for those prone to infections.
- Can probiotics help in preventing fungal infections?
- Yes, probiotics can help maintain gut flora and support immune function, reducing infection risk.
- What role does clothing material play in fungal infection prevention?
- Breathable materials reduce sweating and moisture buildup, making it harder for fungi to thrive.
- Why is it advisable to avoid sharing personal items?
- Sharing items like shoes, towels, or razors can spread fungal infections easily.
- Are there specific hygiene practices I should follow in hot climates?
- Shower frequently, apply antifungal powders, and wear light, loose clothing to manage sweat.
- Can I trust DIY remedies for fungal infections?
- While many DIY remedies can be effective, always consult a healthcare professional if symptoms persist.
- Is it true that some fungi are more difficult to treat?
- Yes, some strains can be resistant to treatment, so early intervention is key.
- How can mindfulness practices help in preventing fungal infections?
- Mindfulness can reduce stress and improve overall health, supporting a strong immune system against infections.
Medical Disclaimer:
The information provided on this website is for general educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.