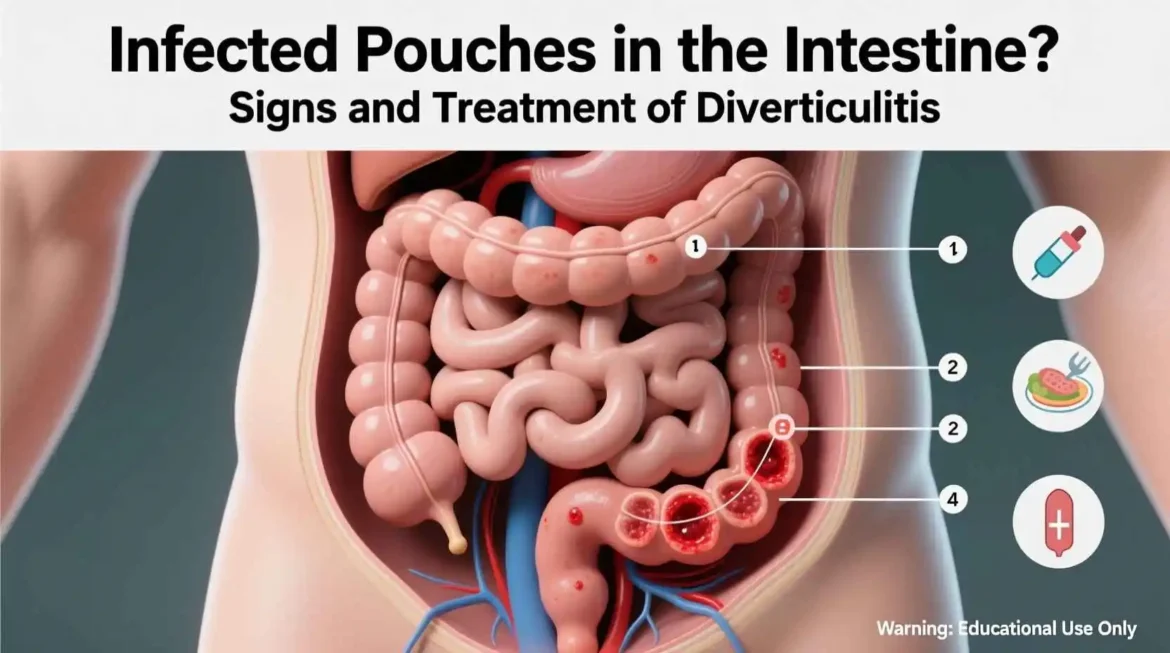
Diverticulitis occurs when small pouches (diverticula) that can form in the lining of the digestive system, most commonly in the colon, become inflamed or infected. While diverticulitis can sometimes lead to severe complications, the majority of cases are classified as uncomplicated diverticulitis. This means there is inflammation without an abscess, perforation, fistula, or obstruction, making it amenable to out-patient, home-based management for most individuals.
Our typical recommendations for managing uncomplicated diverticulitis focus on allowing the colon to rest, reducing inflammation, and preventing potential complications:
- Rest and Activity Modification:
- Prioritize Physical Rest: Your body’s natural healing processes are enhanced when you are well-rested. Limiting strenuous activities and allowing your digestive system to calm down can significantly aid recovery. Avoid heavy lifting and intense exercise during the acute phase.
- Reduce Stress: Emotional stress can sometimes exacerbate digestive symptoms. Practicing relaxation techniques might also be beneficial.
- Carefully Managed Dietary Modifications: The cornerstone of uncomplicated diverticulitis management is often a phased dietary approach designed to reduce irritation of the inflamed colon and gradually reintroduce nutrients as healing progresses. Hydration is also paramount throughout this process.
- Initial Acute Phase (Bowels Rest): For the first few days, the primary goal is to minimize the work of the digestive system. We usually recommend a clear liquid diet. This allows the bowel to rest and inflammation to subside.
- Examples: Clear broths (chicken, vegetable), clear juices (apple, cranberry without pulp), water, plain gelatin, clear sports drinks (without added colors or pulp), clear sodas (ginger ale, Sprite – flat is often preferred), popsicles (without fruit pieces or cream).
- Important: Avoid any solid foods, dairy products, or beverages with pulp or dark colors (like grape juice). Focus on staying well-hydrated.
- Transition Phase (Gradual Reintroduction): As symptoms begin to improve – typically after 2-3 days on a clear liquid diet – you can gradually start to introduce low-fiber, soft, and bland foods. This phase aims to slowly reactivate the digestive system without undue strain.
- Examples: White bread, plain white rice, well-cooked pasta (without heavy sauces), crackers, boiled or baked potatoes (without skin), eggs, poultry without skin (baked or boiled), fish, canned fruits (without skin or seeds), well-cooked, peeled vegetables (e.g., carrots, green beans).
- Guidance: Eat small, frequent meals. Chew your food thoroughly. Continue to avoid anything high in fiber, spicy foods, and foods that are difficult to digest.
- Recovery and Maintenance Phase (Long-Term Health): Once symptoms have fully resolved and you are tolerating a varied diet without discomfort, the focus shifts to gradually increasing dietary fiber. This is crucial for promoting regular bowel movements and can help prevent future episodes of diverticulitis.
- Examples: Whole grains (whole wheat bread, brown rice, oats), fresh fruits (with skin and seeds, as tolerated), a wide variety of vegetables, legumes (beans, lentils), nuts, and seeds.
- Guidance: Increase fiber intake slowly over several weeks to avoid gas, bloating, or discomfort. Ensure adequate fluid intake (at least 8 glasses of water daily) to help fiber move smoothly through the digestive system. A high-fiber diet, along with sufficient hydration, is key to long-term bowel health and reducing the risk of recurrence.
- Initial Acute Phase (Bowels Rest): For the first few days, the primary goal is to minimize the work of the digestive system. We usually recommend a clear liquid diet. This allows the bowel to rest and inflammation to subside.
- Antibiotic Therapy:
- Consideration and Rationale: We sometimes prescribe oral antibiotics to target potential bacterial infection that may be contributing to the inflammation.
- Evolving Research: However, it’s important to note that recent research has suggested that antibiotics may not be necessary for all cases of uncomplicated diverticulitis, especially if the individual is otherwise healthy, has stable vital signs, and shows no signs of systemic infection or severe inflammation.
- Individualized Decision: The decision to prescribe antibiotics is made on a case-by-case basis after a thorough clinical evaluation, weighing the potential benefits against risks such as antibiotic resistance and side effects.
- Pain Management:
- Over-the-Counter Options: Mild to moderate abdominal pain can often be effectively managed with over-the-counter pain relievers such as acetaminophen (paracetamol).
- Caution with NSAIDs: We generally advise against the use of non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen, or aspirin during an acute episode of diverticulitis. NSAIDs can potentially increase the risk of complications such as bleeding, perforation, or aggravation of the inflammatory process.
- Monitoring Pain: If pain worsens, becomes severe, or is not relieved by recommended pain medications, it is crucial to seek immediate medical attention.
Important Considerations and When to Seek Medical Attention:
While most cases of uncomplicated diverticulitis can be managed at home, it is vital to monitor your symptoms closely. You should contact your healthcare provider immediately or seek emergency care if you experience any of the following:
- Worsening or severe abdominal pain
- Persistent fever (over 100.4°F or 38°C)
- Persistent nausea, vomiting, or inability to tolerate oral fluids
- Chills or signs of widespread infection
- Abdominal swelling or tenderness
- Rectal bleeding
- No improvement in symptoms after 2-3 days of home management
Remember, these guidelines are general recommendations. Always consult with your healthcare provider for a proper diagnosis and an individualized treatment plan tailored to your specific condition and medical history.
Complicated Diverticulitis: When Immediate and Intensive Care is Required
Diverticulitis, an inflammation or infection of small pouches (diverticula) in the digestive tract, can sometimes progress to more severe conditions, necessitating urgent and intensive medical intervention.
When diverticulitis leads to complications, such as:
- Abscesses: Collections of pus that form near the infected diverticula.
- Perforations: A hole or tear in the wall of the colon, allowing bowel contents to leak into the abdominal cavity.
- Fistulas: Abnormal connections that form between the colon and other organs (like the bladder, skin, or other parts of the intestine).
- Bowel Obstruction: A blockage in the colon, often due to significant inflammation, scarring, or a large abscess.
…hospital admission is almost always required due to the potential for severe infection, sepsis, and life-threatening complications. Our treatment plan for such cases becomes significantly more intensive and closely monitored:
Intensive Treatment Plan for Complicated Diverticulitis:
- Intravenous (IV) Antibiotics: We administer powerful, broad-spectrum antibiotics directly into the bloodstream. This method ensures rapid and high concentrations of the medication reach the site of infection, effectively combating severe bacterial proliferation throughout the body, especially in cases of systemic infection or suspected perforation. The type and duration of antibiotics are carefully chosen based on the severity of the infection and the patient’s specific condition.
- NPO (Nothing by Mouth): Our patients are typically kept NPO, meaning they are not allowed to consume any food or drink by mouth. This critical measure allows the inflamed bowel to rest completely, minimizing irritation, reducing the passage of stool through the affected area, and promoting healing. It’s a foundational step to stabilize the digestive system and prevent further strain on the compromised colon.
- IV Fluids: To prevent dehydration and maintain electrolyte balance, particularly when patients are NPO, we administer intravenous fluids. This ensures the body receives essential hydration and nutrients, supporting overall organ function and helping the patient’s body fight the infection effectively.
- Drainage of Abscesses: If a localized collection of pus (abscess) forms and is of significant size, it needs to be drained to remove the source of infection and alleviate pressure. This is often performed percutaneously – a minimally invasive procedure where a thin needle or catheter is inserted through the skin directly into the abscess. This entire process is precisely guided by real-time imaging, such as CT scans or ultrasound, to ensure accuracy and safety. This approach can often prevent the need for more invasive surgical intervention.
- Surgery: Surgical intervention becomes necessary for the most severe cases or when specific complications cannot be resolved by non-surgical means. The decision for surgery is made carefully, considering the patient’s overall health, the nature of the complication, and the potential risks.
- Colon Resection (Colectomy): This is a procedure where the inflamed, diseased, or damaged section of the colon is surgically removed.
- Emergency Procedure: It is typically performed as an emergency for critical conditions like a frank perforation (a complete hole in the bowel wall leading to widespread infection in the abdomen, known as peritonitis) or uncontrollable bleeding.
- Planned Procedure: It may also be a planned, elective procedure for patients experiencing recurrent severe attacks of diverticulitis, chronic fistulas that haven’t healed, or persistent bowel obstructions caused by inflammation and scarring that have not responded to medical management. The goal is to remove the source of the problem and prevent future complications.
- Ostomy: In some emergency situations, particularly when the colon is severely inflamed or infected, or if a safe connection (anastomosis) cannot be immediately performed after a resection, a temporary or permanent ostomy may be created.
- This involves bringing a healthy section of the intestine (either the colon for a “colostomy” or the small intestine for an “ileostomy”) through an opening, called a stoma, in the abdominal wall. This allows waste to exit the body into an external collection bag, diverting stool away from the healing or diseased colon.
- Our primary goal is typically to reverse temporary ostomies once the colon has fully healed and inflammation has subsided, a process that usually involves a subsequent surgical procedure several months later. However, in some complex cases, a permanent ostomy may be necessary. We provide comprehensive education and support for patients living with an ostomy, ensuring they maintain a good quality of life.
- Colon Resection (Colectomy): This is a procedure where the inflamed, diseased, or damaged section of the colon is surgically removed.
| Type of Diverticulitis | Typical Management | Key Considerations |
| Uncomplicated | Oral antibiotics (selective), clear/low-fiber diet, pain relief, rest. | Often managed at home. Gradual dietary progression. |
| Complicated (Abscess) | Hospitalization, IV antibiotics, NPO, IV fluids, percutaneous drainage if large. | Close monitoring for signs of worsening infection. |
| Complicated (Perforation/Fistula/Obstruction) | Emergency hospitalization, IV antibiotics, NPO, IV fluids, urgent surgical resection (with possible ostomy). | Life-threatening conditions requiring immediate intervention. |
| Recurrent/Chronic | Lifestyle modifications, planned colonoscopy, elective surgical resection (if severe or frequent attacks). | Focus on prevention and long-term management. |
Prevention and Long-Term Management: A Holistic Approach to Diverticular Disease
“The gut is the gateway to health.” This timeless wisdom, often attributed to the “Father of Medicine,” Hippocrates, underscores the profound connection between our digestive system and overall well-being. Nowhere is this truth more evident than in the context of diverticular disease, particularly when addressing the prevention of recurrent diverticulitis episodes and the long-term maintenance of remission. Our comprehensive, long-term strategy is firmly rooted in empowering individuals through crucial, evidence-based lifestyle modifications. These pillars of health not only reduce the risk of future flare-ups but also contribute to overall improved quality of life:
- High-Fiber Diet: The Cornerstone of Gut Health This is paramount and serves as the fundamental dietary intervention. We strongly advocate for a diet generously rich in diverse sources of fiber, including an abundance of fresh fruits (like berries, apples with skin, pears), a wide variety of vegetables (leafy greens, broccoli, carrots), wholesome whole grains (oats, brown rice, quinoa, whole-wheat bread), and nutrient-dense legumes (lentils, beans, chickpeas). Fiber’s crucial role is to add bulk to stool and absorb water, thereby keeping stools soft, well-formed, and facilitating easier passage through the colon. This action significantly reduces the pressure within the colon walls, minimizing the strain that can contribute to diverticula formation and inflammation. Our aim is for individuals to gradually increase their intake to 25-38 grams of fiber per day, starting slowly to allow the digestive system to adjust and prevent bloating or discomfort.
- Adequate Hydration: A Vital Partner to Fiber Drinking plenty of water throughout the day is non-negotiable for effective digestive function. Water is essential for fiber to work efficiently; it helps swell the fiber, creating the soft, bulky stools necessary for smooth bowel movements. Insufficient hydration can lead to harder, more difficult-to-pass stools, increasing colonic pressure and strain. Aim for at least 8 glasses (approximately 2-3 liters) of plain water daily, more if exercising or in a warm climate.
- Regular Exercise: Promoting Bowel Motility Consistent physical activity plays a significant role in maintaining healthy bowel function and is a powerful tool in preventing constipation, a known risk factor for diverticulitis. Engaging in moderate-intensity exercise, such as brisk walking, jogging, swimming, or cycling, for at least 30 minutes most days of the week, helps to stimulate intestinal motility and improve overall circulation, contributing to a more efficient digestive system. Exercise also offers the added benefit of stress reduction, which can indirectly impact gut health.
- Maintain a Healthy Weight: Reducing Systemic Burden Achieving and maintaining a healthy body weight is crucial. Excess weight, particularly around the abdomen, can increase pressure within the abdominal cavity and is often associated with systemic inflammation, both of which can significantly elevate the risk of diverticular disease and its complications. Working towards a healthy Body Mass Index (BMI) through diet and exercise can profoundly lower this risk, benefiting not just your colon but your entire body.
- Avoid Smoking: Eliminating a Major Risk Factor Smoking is a detrimental habit with far-reaching negative health consequences, and its impact on gut health is no exception. It is a known significant risk factor for diverticulitis, thought to compromise blood flow to the intestines and promote systemic inflammation, making the colon more vulnerable to disease. Quitting smoking is one of the most impactful steps an individual can take to improve their overall health and significantly reduce their risk of diverticulitis and countless other chronic conditions.
- Limit NSAID Use: Protecting the Gut Lining Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen, especially when used long-term or at high doses, can irritate the intestinal lining, increase inflammation, and potentially contribute to the development or exacerbation of diverticular issues, including bleeding or perforation. If possible, we strongly advise limiting their use. It is crucial to have an open discussion with your healthcare provider about alternative pain relief options that are gentler on the digestive system, such as acetaminophen or other non-pharmacological approaches.
By diligently embracing these foundational principles – a fiber-rich diet, ample hydration, regular physical activity, healthy weight management, avoiding smoking, and mindful NSAID use – individuals can significantly reduce their risk of diverticulitis recurrences and foster a healthier, more resilient digestive system. This proactive and holistic approach empowers you to take control of your gut health and improve your overall quality of life.
Conclusion
Diverticulitis, while a common and sometimes debilitating condition, is manageable with the right knowledge and timely intervention. From understanding its potential causes rooted in our lifestyle choices to recognizing the subtle and overt symptoms, we have explored the journey of diagnosis and the array of treatments available. Our ability to recover and prevent future episodes often hinges on our commitment to dietary and lifestyle changes, particularly adopting a high-fiber diet and maintaining proper hydration. By empowering ourselves with this information, we can work closely with our healthcare providers to navigate this condition effectively, ensuring our digestive health and overall well-being remain a priority.
FAQs on Preventing Diverticulitis Naturally
General Understanding & Basics
- Q: What are diverticula, and how do they lead to diverticulitis?
- A: Diverticula are small, bulging pouches that can form in the lining of the large intestine (colon). When these pouches become inflamed or infected, it’s called diverticulitis. Preventing this inflammation/infection is the goal.
- Q: What is the primary natural strategy for preventing diverticulitis flare-ups?
- A: The cornerstone of natural prevention is a high-fiber diet, coupled with adequate hydration and a healthy lifestyle.
- Q: Can lifestyle changes truly prevent diverticulitis, or just manage symptoms?
- A: While existing diverticula won’t disappear, consistent lifestyle changes, particularly dietary, are highly effective in preventing new diverticula from forming and, more importantly, preventing the inflammation (diverticulitis) that causes symptoms.
Dietary Strategies: Fiber Focus
- Q: How much dietary fiber should I aim for daily to help prevent diverticulitis?
- A: Most health organizations recommend 25-30 grams of fiber per day for women and 30-38 grams for men. It’s best to achieve this through food sources.
- Q: What types of fiber are most beneficial for preventing diverticulitis?
- A: Both soluble and insoluble fibers are beneficial. Insoluble fiber adds bulk to stool, helping it pass more easily. Soluble fiber forms a gel, softening stool and contributing to gut health.
- Q: What are excellent food sources of insoluble fiber?
- A: Good sources include whole wheat bread, wheat bran, brown rice, whole-grain pasta, corn, nuts, seeds, and the skins of many fruits and vegetables.
- Q: Which foods provide good sources of soluble fiber?
- A: Oats, barley, apples, citrus fruits (oranges, grapefruit), carrots, psyllium, peas, beans, and lentils are rich in soluble fiber.
- Q: How should I gradually increase my fiber intake to avoid discomfort like gas or bloating?
- A: Start slowly, adding just a few grams of fiber each week. Increase water intake simultaneously. Common discomfort usually subsides as your digestive system adjusts.
- Q: Is hydration important for fiber to work effectively? If so, how much water?
- A: Absolutely critical! Fiber absorbs water to soften stools and allow for easy passage. Aim for at least 8 glasses (roughly 2 liters) of water or other non-caffeinated, unsweetened fluids daily.
Dietary Strategies: Other Foods & Supplements
- Q: Do nuts, seeds, and popcorn cause diverticulitis, and should I avoid them?
- A: No, this is a common myth. Current research shows no evidence that nuts, seeds, or popcorn cause diverticulitis flare-ups or significantly increase risk. In fact, they are good sources of fiber and can be beneficial.
- Q: Are there any foods I should limit or avoid to reduce my risk?
- A: While there are no hard “avoid” lists for prevention (unless you’re having a flare-up), some experts suggest limiting red meat and highly processed foods, which are low in fiber and can contribute to inflammation.
- Q: Can fermented foods like yogurt or kefir help in preventing diverticulitis?
- A: Yes, fermented foods are rich in beneficial probiotics, which can help maintain a healthy gut microbiome. A balanced gut can support overall digestive health and potentially reduce inflammation, aiding prevention.
- Q: Should I consider taking a fiber supplement if I struggle to meet my daily target?
- A: Fiber supplements (like psyllium or methylcellulose) can be helpful to reach your fiber goal, but discuss this with your doctor. Always take them with plenty of water.
- Q: What natural anti-inflammatory foods can I include in my diet?
- A: Include foods rich in omega-3 fatty acids (fatty fish, flaxseed, chia seeds), turmeric, ginger, leafy green vegetables, and berries, all known for their anti-inflammatory properties.
- Q: Is it beneficial to avoid refined carbohydrates and processed foods?
- A: Yes, refined carbs (white bread, sugary cereals) and processed foods are often low in fiber and nutrients, and high in unhealthy fats and sugars, which can contribute to inflammation and an unhealthy gut environment. Prioritize whole, unprocessed foods.
Lifestyle & Habits
- Q: Can exercise help prevent diverticulitis flare-ups?
- A: Yes, regular physical activity is strongly linked to a reduced risk. Exercise helps keep bowel movements regular, reduces pressure in the colon, and can decrease inflammation.
- Q: What kind of exercise is recommended, and how often?
- A: Aim for at least 30 minutes of moderate-intensity exercise most days of the week (e.g., brisk walking, jogging, cycling, swimming). Even light activity is better than none.
- Q: How does maintaining a healthy weight contribute to prevention?
- A: Obesity, particularly abdominal obesity, is associated with an increased risk of diverticulitis. Maintaining a healthy weight reduces overall inflammation and pressure on the digestive system.
- Q: Is stress a factor in diverticulitis, and how can it be managed naturally?
- A: While not a direct cause, chronic stress can negatively impact gut health (the “gut-brain axis”) and may exacerbate digestive issues. Natural stress management techniques include yoga, meditation, deep breathing exercises, and spending time in nature.
- Q: How important is establishing regular bowel habits?
- A: Very important. Passing stools regularly and without straining reduces pressure in the colon, which can lessen the chance of diverticula formation and irritation. Don’t ignore the urge to go.
- Q: Can squatting during bowel movements help in prevention?
- A: Some people find that using a squatting stool (like a Squatty Potty) helps align the colon for easier and more complete bowel movements, reducing strain.
Gut Health & Probiotics
- Q: What role do probiotics play in gut health and diverticulitis prevention?
- A: Probiotics introduce beneficial bacteria to your gut, maintaining a healthy bacterial balance. A balanced microbiome supports digestion, immune function, and can help reduce inflammation, which is key in prevention.
- Q: Which probiotic-rich foods can I incorporate into my diet?
- A: Good sources include plain yogurt with live active cultures, kefir, sauerkraut, kimchi, kombucha, and tempeh.
- Q: Should I consider taking probiotic supplements for prevention?
- A: While food sources are ideal, a probiotic supplement may be beneficial, especially if advised by your doctor or dietitian. Look for supplements with diverse strains and a high CFU count.
- Q: How do prebiotics differ from probiotics, and where can I find them?
- A: Prebiotics are non-digestible fibers that act as food for your beneficial gut bacteria. They are found in many high-fiber foods like onions, garlic, bananas, oats, asparagus, and chicory root.
Things to Avoid & Other Factors
- Q: Is it true that certain medications can increase my risk?
- A: Long-term use of certain medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen, and corticosteroids, may increase the risk of diverticulitis or its complications. Discuss alternatives with your doctor.
- Q: How does smoking impact the risk of diverticulitis?
- A: Smoking is associated with an increased risk of diverticulitis and its complications. Quitting smoking is a significant step toward improving overall gut health and reducing inflammation.
- Q: What about alcohol consumption and its effects on diverticulitis prevention?
- A: Moderate alcohol consumption generally doesn’t significantly increase risk, but excessive intake can dehydrate you and irritate the digestive system, potentially worsening symptoms or contributing to gut dysbiosis. Moderation is key.
Monitoring & When to Seek Help
- Q: How long does it take to see benefits from lifestyle changes for diverticulitis prevention?
- A: While some benefits like improved bowel regularity can be noticed within weeks, consistent adherence to a high-fiber, healthy lifestyle over months and years is what truly reduces the long-term risk of diverticulitis flare-ups.
- Q: When should I seek medical advice despite following natural prevention strategies?
- A: Always consult your doctor if you experience new or worsening abdominal pain, fever, nausea, vomiting, significant changes in bowel habits, or rectal bleeding. These could indicate a diverticulitis flare-up or another serious condition requiring medical attention. Natural strategies are preventative, not a substitute for acute medical care.
Medical Disclaimer:
The information provided on this website is for general educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.