Eczema Symptoms You Should Never Ignore – From Redness to Thickened Skin
For millions of us around the world, the experience of skin that is persistently itchy, red, and inflamed is an unwelcome daily reality. This condition, known broadly as eczema, can feel like a constant battle against our own bodies. It affects our comfort, our confidence, and sometimes even our sleep. But what is truly happening beneath the surface? Why does it occur, and what can we do about it? In this guide, we will journey together to demystify eczema, exploring its complex causes, identifying its varied symptoms, and outlining the modern approaches to diagnosis and treatment that offer hope and relief.
What Exactly Is Eczema? A Deeper Dive
At its core, eczema is not merely a single skin condition, but rather an umbrella term for a group of inflammatory skin conditions that cause the skin to become intensely itchy, red, dry, and irritated. The hallmark symptoms often include persistent itching, which can be relentless and debilitating, along with visible signs like redness, dryness, scaling, weeping, crusting, and thickening of the skin over time.
The most common and widely recognized form, which people often refer to simply as “eczema,” is atopic dermatitis. Understanding the terminology sheds light on its nature:
- The word “atopic” is highly significant. It refers to a genetic predisposition or an inherited tendency to develop other allergic conditions. This means individuals with atopic dermatitis frequently have a personal or family history of related “atopic” diseases, such as allergic asthma (a chronic respiratory condition characterized by airway inflammation) and hay fever (allergic rhinitis, involving nasal inflammation triggered by environmental allergens like pollen or dust mites). This interconnectedness of allergic conditions is sometimes referred to as the “atopic march.”
- “Dermatitis” simply means inflammation of the skin. When combined, “atopic dermatitis” describes an inherited condition causing skin inflammation, often linked to an overactive immune response.
It’s absolutely crucial to understand, and worth reiterating, that eczema is not contagious. You cannot catch it from someone else through touch, shared objects, or airborne particles. This is a vital point to dispel common misconceptions and reduce any social stigma associated with the condition.
Eczema is a chronic condition, meaning it can persist over a long period, often throughout a person’s life, rather than being a temporary ailment. Its course is typically characterized by fluctuating periods:
- Flare-ups: These are times when symptoms worsen dramatically, becoming more intense, widespread, and uncomfortable. Flares can be triggered by a variety of factors including environmental irritants (like certain soaps, detergents, or fabrics), allergens (such as dust mites, pet dander, or pollens), stress, changes in temperature or humidity, or even certain foods.
- Remission: These are periods when symptoms improve significantly, lessen in severity, or may even disappear entirely, leaving the skin largely clear and calm. Managing triggers and adhering to treatment plans often helps prolong periods of remission.
For many, eczema begins in infancy or early childhood, sometimes improving or even resolving by adulthood. However, it’s important to note that it can also develop for the first time at any age, affecting adolescents, adults, and even seniors.
Our goal in exploring this condition is to move beyond simply managing symptoms. We aim to delve deeper into understanding the complex mechanisms behind eczema, which involve a combination of genetic factors, a compromised skin barrier (allowing irritants and allergens to penetrate more easily), immune system dysregulation (leading to an exaggerated inflammatory response), and environmental triggers. A comprehensive understanding of these underlying processes is key to developing more effective, personalized management strategies, improving the quality of life for those affected, and fostering a better relationship with their skin.
Unraveling the Complex Causes: A Deep Dive into Eczema’s Origins
One of the most profoundly challenging and often frustrating aspects of managing eczema is the perplexing and often elusive nature of its exact cause. Unlike some conditions with a single, identifiable root, eczema is a sophisticated and highly individualized disorder. We now understand that it doesn’t stem from one culprit, but rather emerges from a complex and dynamic interplay between an individual’s unique genetic predispositions and a myriad of environmental factors. Picture it like this: your body’s inherited genetic blueprint might create a foundational vulnerability in your skin, making it inherently more susceptible to irritation and inflammation. Then, various external triggers act as the catalysts, activating and intensifying the noticeable symptoms of eczema.
• The Genetic Link: Inherited Vulnerability
Research has unequivocally identified a robust hereditary component to eczema. It’s common to observe a strong family history of not just eczema itself, but also related allergic conditions such as asthma or hay fever – a trio often referred to by medical professionals as the “atopic triad.” This familial connection strongly suggests that genes play a significant role in determining who develops the condition.
A pivotal discovery in unraveling this genetic puzzle involves a specific gene that is instrumental in the creation of a crucial protein called filaggrin (filament aggregating protein). Filaggrin is far more than just a protein; it’s a foundational component for building a healthy, robust, and protective skin barrier. In individuals with properly functioning filaggrin, this protein helps to bind skin cells together, creating a strong, resilient outermost layer that effectively seals in moisture and keeps harmful substances out.
However, when this filaggrin gene is mutated or deficient – a common finding in many eczema sufferers – the consequences for the skin barrier are profound. It becomes inherently “leaky” or compromised. This compromised barrier functions inefficiently, allowing precious moisture to escape far too easily (leading to characteristic dryness, flakiness, and tightness) while simultaneously providing an open gateway for irritants, allergens, and even microbes to penetrate the deeper layers of the skin more readily. Once these foreign invaders breach the weakened barrier, the immune system, sensing a threat, mounts an exaggerated inflammatory response, leading to the redness, itching, and swelling typical of an eczema flare.
• Environmental Triggers: The Catalysts for Flare-Ups
While our genes might load the metaphorical gun by predisposing us to eczema, it is often the direct interaction with our environment that pulls the trigger, initiating or exacerbating symptoms. Consequently, a cornerstone of effective eczema management involves meticulously identifying and diligently managing these environmental triggers, as their avoidance can significantly reduce the frequency and severity of flare-ups. Common culprits include:
- Irritants: These are everyday substances that, when they come into contact with sensitive, eczema-prone skin, can strip away its natural protective oils and disrupt its delicate pH balance. This chemical assault further compromises an already vulnerable skin barrier. Common examples include harsh soaps (especially those with high pH, fragrances, or dyes), strong detergents and laundry products, specific shampoos and conditioners, disinfectants, cleaning agents, and even certain fabrics like rough wool or synthetic materials that can cause friction and overheating.
- Expanded Insight: Even seemingly innocuous products can contain hidden irritants. Opting for “fragrance-free,” “dye-free,” and “hypoallergenic” products is often recommended.
- Allergens: Substances that provoke an allergic reaction in the immune system can trigger or intensify an eczema flare, particularly in individuals with the genetic predisposition for atopy. These allergens can be broadly categorized:
- Airborne Allergens: Microscopic dust mites (and their droppings), pet dander (from cats, dogs, etc.), pollen from trees, grasses, and weeds are ubiquitous in our environment and can settle on the skin, or be inhaled, initiating an immune response that manifests as skin inflammation.
- Food-Related Allergens: While less common as a direct cause of all eczema, certain foods can be significant triggers for some individuals, especially children. Common food culprits include dairy products, eggs, peanuts and tree nuts, soy, and wheat. Identifying food triggers often requires careful observation and, importantly, medical supervision, as unnecessary elimination diets can lead to nutritional deficiencies.
- Climate and Temperature: Extreme weather conditions can be particularly harsh on sensitive and already compromised skin. Dry, cold winter air, often exacerbated by indoor heating systems that strip moisture from the environment, can lead to significant skin dehydration and cracking, making it more prone to irritation. Conversely, hot and humid weather, while seemingly moisturizing, can lead to excessive sweating. Sweat, with its salt and urea content, can be highly irritating to eczema-prone skin, leading to intense itching and inflammation, especially in skin folds.
- Expanded Insight: Sudden changes in temperature, such as moving from a warm indoor environment to cold outdoor air, can also stress the skin and trigger flares.
- Hormonal Fluctuations: For many women, there’s a clear link between hormonal changes and their eczema symptoms. Fluctuations during the menstrual cycle (often pre-menstrual or during ovulation), pregnancy, or the perimenopausal and menopausal stages can lead to intensified flare-ups. The exact mechanism isn’t fully understood but is thought to involve the influence of hormones on immune system modulation and skin barrier function.
- Expanded Insight: Tracking symptoms in relation to hormonal cycles can help individuals anticipate and prepare for potential flares.
- Stress: While emotional or psychological stress does not directly cause eczema, the powerful mind-skin connection is undeniable. Stress is a well-documented exacerbating factor that can significantly worsen existing eczema symptoms. It can trigger a cascade of internal responses, including the release of stress hormones, which can affect the immune system and the skin’s barrier function. Most notably, stress can intensify the “itch-scratch cycle” – the more stressed a person feels, the more intensely they may perceive itch, leading to more scratching, which further damages the skin barrier, perpetuating inflammation and creating a vicious cycle that is incredibly difficult to break.
- Expanded Insight: Incorporating stress-management techniques such as mindfulness, meditation, regular exercise, adequate sleep, and seeking psychological support can be invaluable in managing eczema severity.
Understanding eczema means appreciating its multifaceted nature. It’s a condition where an individual’s inherent genetic blueprint creates a susceptible skin environment, which is then perpetually challenged and expressed through interactions with various elements in their daily environment. Effective management, therefore, demands a holistic and personalized approach, addressing both the underlying predispositions and the tangible triggers.
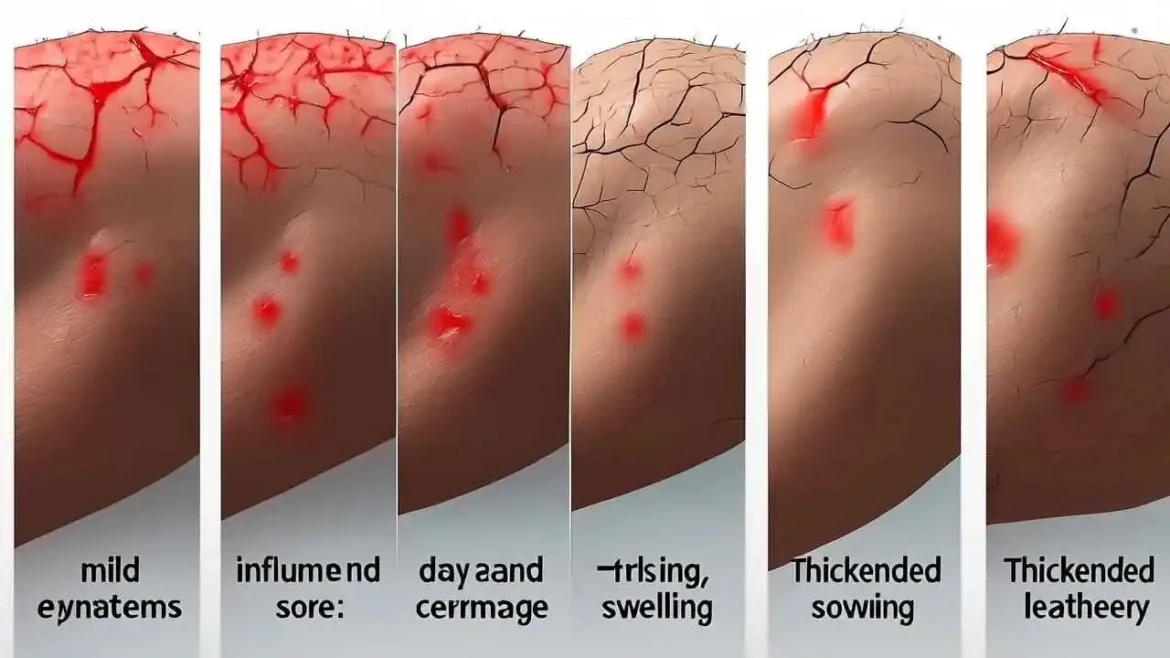
Recognizing the Signs: A Spectrum of Symptoms
While “itchy, red rash” is the classic description, the symptoms of eczema can vary significantly from person to person and by age. Together, these signs paint a clearer picture of the condition we’re facing.
- Intense Itching (Pruritus): This is the hallmark symptom. The itch can be unrelenting and is often worse at night.
- Dry, Sensitive Skin: The compromised skin barrier leads to chronic dryness.
- Inflamed, Discolored Patches: Skin may appear red on lighter skin tones, or brown, purple, or ashen grey on darker skin tones.
- Rough, Leathery, or Scaly Patches: Chronic scratching can cause the skin to thicken over time in a process called lichenification.
- Oozing or Crusting: In severe flares, small, fluid-filled blisters (vesicles) may form, which can weep clear fluid and then crust over.
- Swelling: The affected areas may become swollen, particularly after prolonged scratching.
The Many Faces of Eczema
While atopic dermatitis is the most prevalent, it’s important for us to recognize that “eczema” is an umbrella term for several distinct types of skin inflammation. Understanding the specific type can help tailor the most effective treatment.
| Type of Eczema | Key Characteristics | Common Locations |
| Atopic Dermatitis | The classic, chronic, itchy, and inflammatory form linked to the atopic triad. | Creases of elbows/knees, neck, wrists, ankles. |
| Contact Dermatitis | A rash caused by direct contact with an irritant or allergen (e.g., poison ivy, nickel). | Anywhere the skin had contact with the trigger. |
| Dyshidrotic Eczema | Characterized by small, intensely itchy blisters. | Palms of hands, soles of feet, sides of fingers. |
| Nummular Eczema | Presents as coin-shaped, scaly, and itchy patches on the skin. | Arms, legs, torso, and hands. |
| Seborrheic Dermatitis | Causes flaky, yellowish scales on oily areas; known as “cradle cap” in infants. | Scalp, face (eyebrows, sides of nose), chest. |
Seeking a Diagnosis and Crafting a Treatment Plan