This remains the most significant and well-documented risk factor for all neural tube defects, including encephalocele.
- Why it Matters: Folic acid, the synthetic form of the B vitamin folate, is a cornerstone of healthy cellular development. Its primary role is in synthesizing and repairing DNA and producing red blood cells. During the first 28 days of pregnancy—often before a woman is even aware she is pregnant—the embryo’s neural tube is forming and closing to become the brain and spinal cord. Adequate folate levels are absolutely critical for the rapid cell division and differentiation required for this process to occur correctly. A deficiency can disrupt this intricate sequence, leading to an incomplete closure of the tube.
- Recommendation: Because of this critical early window, health organizations worldwide recommend that all women of childbearing age consume 400 micrograms (mcg) of folic acid daily, even if they are not actively trying to conceive. This ensures that a protective level is already present should a pregnancy occur.
2. Genetic Predisposition
While the vast majority of encephalocele cases are sporadic (meaning they occur without any known family history), genetics can play a role.
- Family History: A woman who has previously had a child with a neural tube defect (like encephalocele, spina bifida, or anencephaly), or who has an NTD herself, has a slightly elevated risk in subsequent pregnancies. The same applies if the father or a close relative has a history of NTDs. This suggests that certain inherited genes may make an embryo more susceptible to environmental triggers.
- Specific Genetic Syndromes: In rarer cases, an encephalocele can be a known feature of a specific genetic disorder. For example, Meckel-Gruber syndrome is a severe inherited condition characterized by a trio of symptoms, including encephalocele, polycystic kidneys, and extra fingers or toes (polydactyly).
3. Maternal Health Conditions and Environmental Factors
The uterine environment plays a vital role in fetal development. Certain health conditions or exposures can increase the risk of NTDs.
- Poorly Controlled Diabetes: Women with pre-existing diabetes who have high blood glucose levels (hyperglycemia) during the early stages of pregnancy face a significantly higher risk. These elevated sugar levels are considered teratogenic, meaning they can be toxic to the developing embryo and interfere with key developmental pathways, including neural tube closure.
- Maternal Obesity: Research has consistently shown a link between a high maternal body mass index (BMI) and an increased risk of NTDs. While the exact mechanism is not fully understood, it may be related to underlying metabolic issues like insulin resistance, altered glucose metabolism, or chronic inflammation.
- Hyperthermia (Elevated Body Temperature): A significant increase in the mother’s core body temperature during the first trimester can disrupt protein synthesis and cell division. This can be caused by a high-grade fever from an infection (like the flu) or prolonged exposure to high heat from external sources, such as frequent use of hot tubs or saunas.
4. Exposure to Certain Medications
Some medications can interfere with the body’s metabolic processes, particularly the way it absorbs and uses folate. These are sometimes referred to as “folate antagonists.”
- Anti-Seizure Medications: The most well-known example is valproic acid (Depakote), a medication used to treat epilepsy, bipolar disorder, and migraines. It has been definitively linked to a higher risk of neural tube defects because it inhibits folate metabolism. Other anti-seizure drugs may also carry a similar, though often lower, risk.
- Important Note: It is crucial for women taking these medications to not stop them abruptly. Instead, they should consult with their doctor before planning a pregnancy. A physician can explore options such as switching to a safer alternative, adjusting the dosage, or prescribing a higher-dose folic acid supplement to mitigate the risk while effectively managing the underlying health condition.
“All women of reproductive age should get 400 micrograms (mcg) of folic acid every day to get enough folic acid to help prevent some birth defects because about half of all pregnancies in the United States are unplanned.” — The Centers for Disease Control and Prevention (CDC)
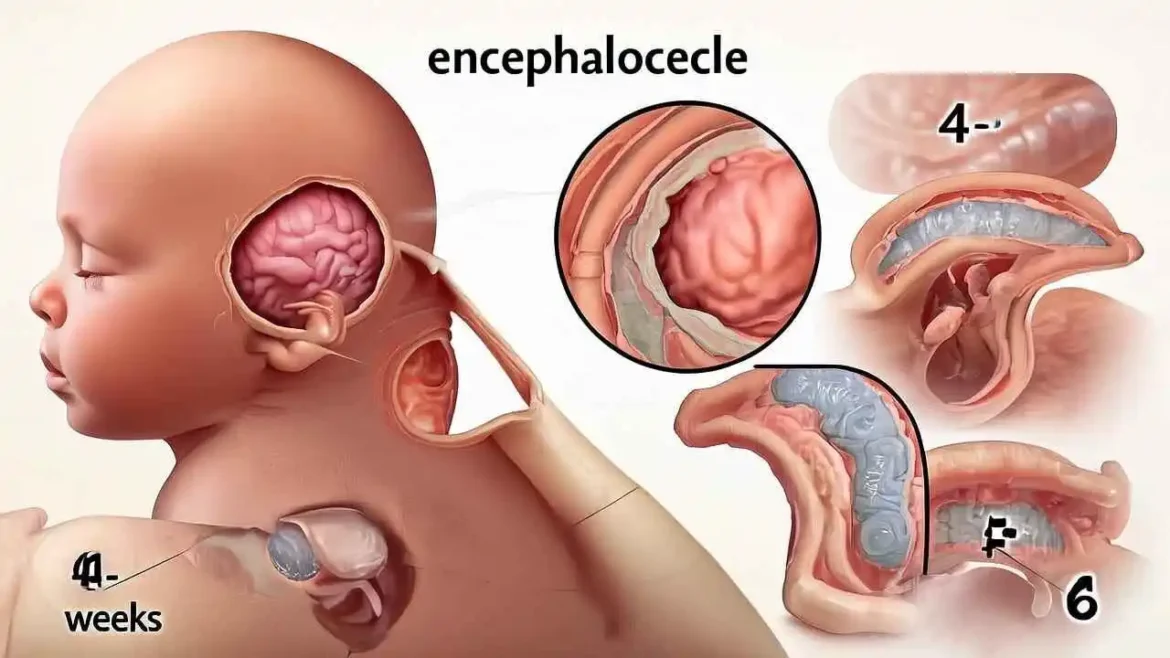
The Diagnostic Journey: From Prenatal Screening to Postnatal Imaging
The diagnosis of an encephalocele, a rare type of neural tube defect, is a step-by-step process that can begin long before a child is born. This diagnostic journey involves a multidisciplinary team of specialists and a sequence of increasingly detailed investigations designed to understand the exact nature of the condition. For parents, this path is often filled with uncertainty, but each step provides crucial information for medical planning and decision-making. The process typically follows a clear path, from initial suspicion to a definitive surgical plan.
1. Prenatal Screening: The First Indication
The first clue that a neural tube defect may be present often comes from a routine maternal blood test performed during the second trimester of pregnancy. This test, often part of a “quad screen,” measures the level of alpha-fetoprotein (AFP). AFP is a protein produced by the fetal liver that circulates in the fetal bloodstream and, in smaller amounts, crosses the placenta into the mother’s blood. If there is an opening in the fetus’s skin, such as with an open neural tube defect like an encephalocele or spina bifida, an excess amount of AFP can leak into the amniotic fluid and subsequently into the maternal bloodstream.
An elevated AFP level is not a diagnosis in itself but a significant screening marker. It acts as a red flag that indicates an increased risk and signals the need for more definitive testing to determine the cause.
2. Prenatal Ultrasound: Visualizing the Abnormality
Following an abnormal AFP screen, or as part of a routine anatomy scan (typically around 18-22 weeks of gestation), a detailed prenatal ultrasound is the primary tool for diagnosing an encephalocele. A skilled sonographer will meticulously examine the fetal anatomy. They look for a characteristic defect or gap in the skull bone (calvarium) through which a sac-like protrusion emerges. This sac may contain only cerebrospinal fluid and the brain’s protective membranes (a meningocele) or, more critically, portions of brain tissue itself (an encephalocele). The location of the encephalocele—most commonly at the back of the skull (occipital)—can also be identified.
3. Fetal MRI: A Deeper Look for Prognosis and Planning
If an ultrasound confirms the presence of a probable encephalocele, a fetal Magnetic Resonance Imaging (MRI) scan is often recommended. This advanced, non-invasive imaging technique uses a powerful magnetic field instead of radiation to create highly detailed, cross-sectional images of the fetus.
A fetal MRI provides invaluable information that an ultrasound cannot:
- Contents of the Sac: It can clearly differentiate between fluid and brain tissue within the sac and, most importantly, help identify which parts of the brain have herniated. This distinction is critical for prognosis, as the involvement of vital brain structures (like the brainstem or visual cortex) significantly impacts the child’s future neurological function.
- Associated Brain Abnormalities: Encephaloceles are often accompanied by other structural brain issues. The MRI can detect conditions like hydrocephalus (an accumulation of excess cerebrospinal fluid in the brain’s ventricles), agenesis of the corpus callosum (the absence of the structure connecting the brain’s two hemispheres), and Chiari malformations.
- Surgical Planning: This detailed anatomical map helps the pediatric neurosurgery team begin preliminary planning for postnatal repair even before the baby is born.
The information gathered from the fetal MRI allows the medical team to provide parents with more accurate counseling about the potential outcomes and to prepare a comprehensive plan for delivery and immediate postnatal care.
4. Postnatal Diagnosis and Surgical Preparation
In cases where the encephalocele was not detected prenatally, it is typically diagnosed immediately at birth due to the obvious physical presence of the sac protruding from the infant’s head. The immediate priorities are to protect the delicate sac from rupture or infection and to stabilize the newborn.
Once the baby is stable, definitive imaging is performed to create a precise roadmap for surgical intervention.
- Computed Tomography (CT) Scan: A CT scan is particularly effective at creating detailed, three-dimensional images of the bony structures, providing the surgeon with a clear view of the size and shape of the defect in the skull.
- Magnetic Resonance Imaging (MRI): An MRI is considered the gold standard for evaluating the soft tissues. It gives the neurosurgeon an unparalleled view of the brain’s anatomy, the exact amount and type of neural tissue within the sac, and the surrounding blood vessels.
Together, these postnatal imaging studies provide the surgical team with all the necessary information to plan a complex procedure aimed at gently placing the herniated brain tissue back into the skull, repairing the protective membranes, and closing the defect in the skull and scalp. This meticulous diagnostic journey, from the first blood test to the final MRI, ensures that every decision is informed, allowing the medical team to provide the best possible care for the child.
Treatment and Long-Term Management: A Comprehensive Team Approach
The journey of managing an encephalocele begins with intensive treatment but extends into a lifetime of coordinated care, underscoring the necessity of a dedicated, multidisciplinary team.
The Initial Surgical Intervention
The primary and most urgent treatment for an encephalocele is surgery, which is typically performed shortly after birth or within the first few months of life, once the infant is stable. The timing depends on the size and location of the encephalocele, the presence of skin covering the sac (which reduces the immediate risk of infection), and the baby’s overall health.
The goals of this complex surgery are multifaceted:
- Preservation and Repositioning: To gently place the protruding brain tissue and meninges (the protective membranes surrounding the brain) back inside the skull. The neurosurgeon carefully assesses the herniated tissue to preserve as much functional brain matter as possible.
- Sac Removal and Closure: To remove the external sac and meticulously close the dura mater (the outermost meninx) to create a watertight seal, preventing leakage of cerebrospinal fluid (CSF).
- Cranial Reconstruction: To repair the opening in the skull. This is a critical step to protect the brain from injury and allow for normal growth. The repair may involve simply bringing the bone edges together, but for larger defects, it often requires the use of bone grafts (taken from the ribs or other parts of the skull) or synthetic plates to ensure a durable and stable closure.
This delicate procedure requires an expert surgical team, led by a pediatric neurosurgeon. For encephaloceles affecting the face or forehead (frontoethmoidal), a craniofacial or plastic surgeon is essential. Their collaboration ensures not only the protection of the brain but also the best possible long-term functional and cosmetic outcome, minimizing facial deformities.
Post-Operative Care and Immediate Recovery
Following surgery, the infant will be monitored in a Neonatal Intensive Care Unit (NICU). Immediate post-operative care focuses on preventing complications such as infection, managing pain, monitoring for seizures, and ensuring proper healing.
Long-Term Management: A Lifelong Journey
Surgery is the first critical step, but it is not the end of treatment. The long-term prognosis for a child with an encephalocele varies widely and depends on the amount and location of brain tissue involved. Many children require ongoing support to address associated neurological and developmental challenges.
A key component of long-term management is monitoring for and treating potential complications, including:
- Hydrocephalus: A common associated condition where excess cerebrospinal fluid builds up in the brain’s ventricles, increasing pressure. This often requires a second surgery to place a shunt, a thin tube that drains the excess fluid to another part of the body, like the abdomen.
- Seizure Disorders (Epilepsy): Brain tissue that has been affected by the encephalocele can be a source of abnormal electrical activity, leading to seizures that require management with medication.
- Developmental Delays: Depending on the area of the brain affected, children may experience delays in reaching motor, cognitive, and social milestones.
- Physical and Motor Impairments: This can include muscle weakness or stiffness (spasticity), problems with coordination, and difficulty with balance.
- Vision and Hearing Problems: If the encephalocele or associated brain abnormalities affect the optic or auditory pathways.
The Multidisciplinary Care Team
Successfully navigating these challenges requires a comprehensive and collaborative team of specialists who work with the child and family throughout their development:
- Pediatrician: The central coordinator of the child’s overall health and care.
- Pediatric Neurologist: Manages conditions like hydrocephalus and epilepsy, and monitors overall neurological development.
- Physical Therapist (PT): Helps with gross motor skills like sitting, standing, and walking.
- Occupational Therapist (OT): Focuses on fine motor skills, sensory processing, and activities of daily living, such as feeding and dressing.
- Speech-Language Pathologist (SLP): Addresses issues with speech, language comprehension, and potential feeding or swallowing difficulties.
- Developmental Pediatrician: Assesses the child’s overall developmental progress and helps create a comprehensive therapy plan.
- Social Worker or Case Manager: Provides invaluable support to the family, helping them navigate the healthcare system, access community resources, and cope with the emotional and financial challenges.
This team approach ensures that care is not fragmented. Instead, it is a holistic strategy aimed at early intervention, continuous monitoring, and adaptive support, with the ultimate goal of maximizing the child’s functional independence and quality of life.
However, surgery is just the first step. Long-term management is crucial, as children with an encephalocele often face associated challenges. The prognosis varies widely and depends heavily on whether viable brain tissue was involved. A multidisciplinary team is essential for providing comprehensive care.
The Multidisciplinary Care Team
| Specialist | Role in Care |
| Pediatric Neurosurgeon | Performs the primary surgical repair and manages related neurological issues like hydrocephalus, which may require a shunt. |
| Pediatrician | Oversees the child’s overall health, growth, and development, coordinating care among specialists. |
| Neurologist | Manages seizure disorders, monitors neurological development, and addresses other brain-related complications. |
| Physical Therapist (PT) | Helps with motor skills, balance, strength, and mobility. |
| Occupational Therapist (OT) | Assists with fine motor skills, daily living activities (e.g., feeding, dressing), and sensory processing issues. |
| Ophthalmologist | Manages vision problems, which are common with occipital encephaloceles due to the proximity to the brain’s visual cortex. |
| Endocrinologist | Monitors and treats pituitary or hormonal issues that can arise from defects at the base of the skull. |
Conclusion: A Journey of Resilience
Encephalocele is a serious and complex congenital condition that presents significant challenges for children and their families. However, through advancements in prenatal diagnosis, neurosurgical techniques, and comprehensive, team-based rehabilitative care, we have made enormous strides. While the road ahead can be long, the prognosis for many children is more hopeful than ever before. Our continued understanding of its causes, especially the vital role of folic acid in prevention, and our commitment to multidisciplinary support, empowers us to provide the best possible care and quality of life for these resilient individuals.
FAQs on preventing Encephalocele by natural remedies and lifestyle changes:
- Q: What is Encephalocele and how can it be prevented?
A: Encephalocele is a birth defect where a portion of the brain protrudes through an opening in the skull. It can be prevented by ensuring adequate folic acid intake, maintaining a healthy diet, and avoiding certain environmental toxins.
- Q: How can I reduce the risk of Encephalocele during pregnancy?
A: You can reduce the risk by taking folic acid supplements, eating a balanced diet rich in fruits and vegetables, and avoiding exposure to pesticides and heavy metals.
- Q: What are some natural remedies that can help prevent Encephalocele?
A: Some natural remedies that may help include consuming foods rich in omega-3 fatty acids, vitamin B12, and antioxidants, as well as practicing stress-reducing techniques like meditation and yoga.
- Q: Can a healthy diet help prevent Encephalocele?
A: Yes, a diet rich in essential nutrients, including folic acid, iron, and calcium, can help reduce the risk of Encephalocele.
- Q: How does folic acid help prevent Encephalocele? A: Folic acid is crucial for fetal development, and adequate intake can help prevent neural tube defects, including Encephalocele.
- Q: Can lifestyle changes help prevent Encephalocele?
A: Yes, maintaining a healthy weight, not smoking, and limiting exposure to environmental toxins can all contribute to a reduced risk of Encephalocele.
- Q: Are there any specific foods that can help prevent Encephalocele?
A: Foods rich in folate, such as leafy greens, citrus fruits, and legumes, can help prevent Encephalocele.
- Q: How can I ensure I’m getting enough folic acid during pregnancy?
A: You can ensure adequate folic acid intake by taking prenatal vitamins, eating folate-rich foods, and consulting with your healthcare provider.
- Q: Can stress contribute to the risk of Encephalocele?
A: High stress levels may contribute to an increased risk of Encephalocele, making stress-reducing techniques like meditation and yoga beneficial.
- Q: Are there any environmental toxins that can increase the risk of Encephalocele?
A: Exposure to pesticides, heavy metals, and certain chemicals has been linked to an increased risk of Encephalocele.
- Q: Can exercise help prevent Encephalocele?
A: Regular exercise can contribute to overall health and well-being, potentially reducing the risk of Encephalocele.
- Q: How does vitamin B12 help prevent Encephalocele?
A: Vitamin B12 plays a role in fetal development, and adequate intake may help reduce the risk of Encephalocele.
- Q: Can omega-3 fatty acids help prevent Encephalocele?
A: Omega-3 fatty acids are essential for fetal brain development, and adequate intake may help reduce the risk of Encephalocele.
- Q: Are there any herbal supplements that can help prevent Encephalocele?
A: Certain herbal supplements, such as those rich in antioxidants, may be beneficial, but always consult with a healthcare provider before taking any supplements during pregnancy.
- Q: How can I minimize exposure to environmental toxins during pregnancy?
A: You can minimize exposure by avoiding pesticides, using non-toxic household cleaners, and limiting contact with heavy metals.
- Q: Can a healthy weight help prevent Encephalocele?
A: Maintaining a healthy weight before and during pregnancy can help reduce the risk of Encephalocele.
- Q: How does smoking affect the risk of Encephalocele?
A: Smoking during pregnancy can increase the risk of Encephalocele, making quitting essential for a healthy pregnancy.
- Q: Can a family history of Encephalocele increase the risk?
A: A family history of Encephalocele or other neural tube defects may increase the risk, making it essential to consult with a healthcare provider.
- Q: Are there any genetic factors that contribute to Encephalocele?
A: Genetic factors can play a role in the development of Encephalocele, making genetic counseling beneficial for high-risk families.
- Q: Can Encephalocele be prevented entirely through natural remedies and lifestyle changes?
A: While natural remedies and lifestyle changes can reduce the risk, Encephalocele cannot be entirely prevented in all cases.
- Q: How can I manage stress during pregnancy to reduce the risk of Encephalocele?
A: Practicing stress-reducing techniques like meditation, yoga, and deep breathing can help manage stress during pregnancy.
- Q: Are there any specific nutrients that are crucial for fetal brain development?
A: Nutrients like folic acid, omega-3 fatty acids, and vitamin B12 are essential for fetal brain development.
- Q: Can a prenatal vitamin help prevent Encephalocele?
A: Taking a prenatal vitamin that contains folic acid and other essential nutrients can help reduce the risk of Encephalocele.
- Q: How can I ensure I’m getting enough omega-3 fatty acids during pregnancy?
A: You can ensure adequate omega-3 intake by consuming fatty fish, taking omega-3 supplements, and eating foods fortified with omega-3s.
- Q: Are there any specific antioxidants that can help prevent Encephalocele?
A: Antioxidants like vitamin C, vitamin E, and beta-carotene may help reduce the risk of Encephalocele.
- Q: Can a healthy lifestyle help prevent other birth defects besides Encephalocele?
A: Yes, a healthy lifestyle can help reduce the risk of various birth defects, including neural tube defects and heart defects.
- Q: How can I reduce my exposure to heavy metals during pregnancy?
A: You can minimize exposure by avoiding contaminated fish, limiting contact with lead-based products, and using non-toxic household cleaners.
- Q: Can Encephalocele be detected during pregnancy?
A: Encephalocele can often be detected during prenatal ultrasounds, allowing for early intervention and planning.
- Q: Are there any specific medical conditions that increase the risk of Encephalocele?
A: Certain medical conditions, such as diabetes and obesity, may increase the risk of Encephalocele.
- Q: Can a healthcare provider recommend personalized advice for preventing Encephalocele?
A: Yes, a healthcare provider can offer personalized guidance on reducing the risk of Encephalocele based on individual circumstances and medical history.
Medical Disclaimer:
The information provided on this website is for general educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.