Understanding Avascular Necrosis: When Bone Meets a Blood Supply Crisis
Our bodies are intricate, dynamic systems, and at the heart of their function is the circulatory system. We often think of blood as the life force for our organs—the heart, brain, and lungs—but it is just as vital for the living tissue that makes up our skeleton. When this crucial blood supply is cut off from a section of bone, the tissue can no longer sustain itself. This condition, known as avascular necrosis (AVN) or osteonecrosis, is essentially the death of bone tissue, leading to a cascade of problems that can severely impact mobility and quality of life.
In this article, we will delve into the complex world of avascular necrosis. We’ll explore what it is, what causes it, how it’s diagnosed, and the spectrum of treatments available, from conservative measures to advanced surgical interventions.
What is Avascular Necrosis (AVN)?
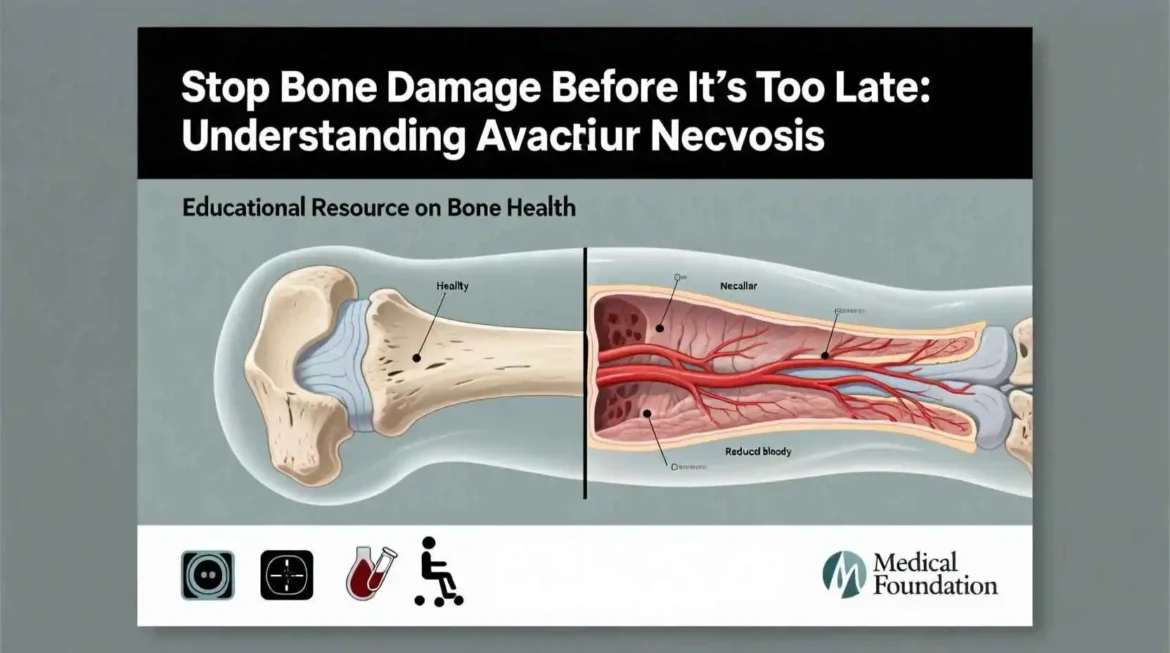
Imagine a thriving, vibrant city that suddenly has all of its supply routes – roads, railways, and ports – cut off. Without food, water, and essential resources, the city would inevitably begin to wither and collapse. Avascular necrosis (AVN), also known as osteonecrosis, works on a similar principle, but at a microscopic, cellular level within our bones.
Bone isn’t the static, lifeless material we often perceive it to be. It’s a living, dynamic, and constantly regenerating tissue. Like any living tissue, it requires a constant and reliable supply of blood. This blood flow delivers vital oxygen and nutrients to the bone cells (osteocytes) and effectively removes waste products generated by their metabolic processes. When this crucial blood supply is disrupted or compromised, the bone cells are deprived of what they need to survive, and they begin to die. This cellular death is what constitutes necrosis.
Initially, avascular necrosis may cause no noticeable symptoms. The early stages can be silent and insidious, developing without any pain or discomfort. However, as the necrosis progresses and a greater number of bone cells die, the structural integrity of the bone gradually weakens. Over time, microscopic fractures or breaks can occur within the affected bone, much like hairline cracks appearing in a building’s foundation. Eventually, this weakening can lead to the collapse of the bone’s surface, resulting in joint damage and significant pain. This collapse is what often triggers the significant pain, stiffness, and disability associated with advanced AVN. It can severely limit range of motion and impact a person’s ability to perform everyday activities.
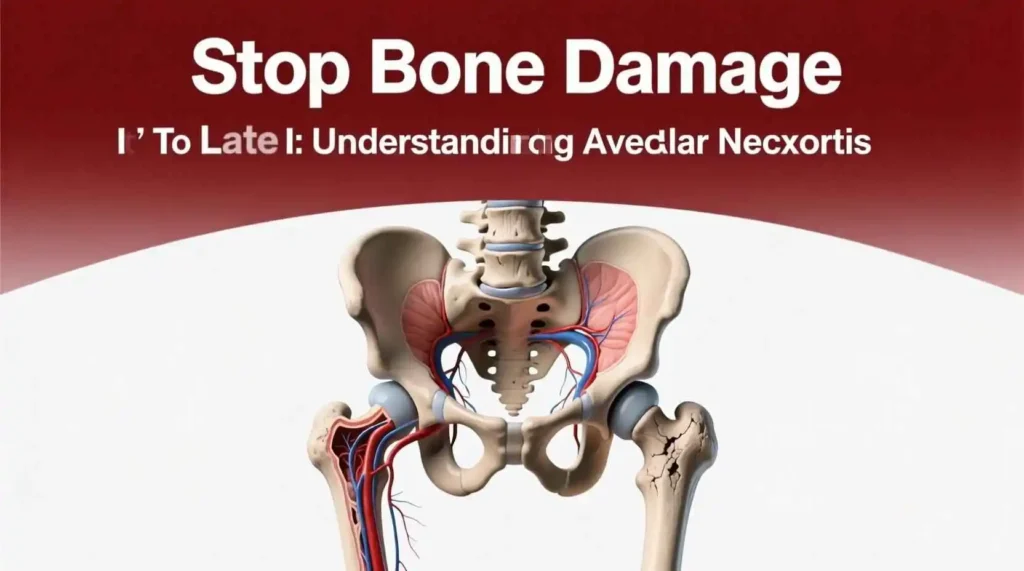
While AVN can theoretically occur in any bone in the body, some areas are more vulnerable due to their unique anatomy and relatively tenuous blood supply. These areas often rely on a limited number of blood vessels, making them more susceptible to disruption. The most commonly affected joints include:
- The Hip: The femoral head (the “ball” of the ball-and-socket hip joint) is the most common site for AVN. The blood supply to the femoral head can be easily disrupted by injury, certain medical conditions, or even some medications.
- The Knee: The femoral condyles (the rounded ends of the femur that articulate with the tibia) or the tibial plateau (the upper surface of the tibia) can be affected. AVN in the knee can lead to pain, stiffness, and difficulty bearing weight.
- The Shoulder: The humeral head (the “ball” of the shoulder joint) is another common location. Similar to the hip, the blood supply to the humeral head can be compromised, leading to AVN and shoulder pain.
- The Ankle: The talus bone in the ankle, which connects the tibia and fibula to the foot, is also susceptible. AVN of the talus can cause chronic ankle pain and instability.
Understanding what AVN is, how it develops, and where it commonly occurs is the first step towards recognizing its potential impact and seeking appropriate diagnosis and treatment. Early detection and intervention are crucial for managing AVN and preserving joint function.
“The good physician treats the disease; the great physician treats the patient who has the disease.” — Sir William Osler
This quote is particularly relevant to AVN, as treatment must be tailored not just to the stage of the disease, but to the individual’s age, activity level, and overall health.
The Culprits: Causes and Risk Factors of Avascular Necrosis (AVN)
The interruption of blood flow that leads to Avascular Necrosis (AVN), also known as osteonecrosis, can happen for two primary reasons: traumatic injury or non-traumatic factors. Understanding these causes and associated risk factors is crucial for diagnosis, prevention, and management of this condition.
1. Traumatic Causes: Direct Impact and Blood Vessel Damage
A severe injury, such as a joint dislocation, bone fracture, or even significant soft tissue damage around a joint, can physically damage blood vessels and disrupt the supply to a section of bone. This disruption deprives the bone tissue of essential oxygen and nutrients, potentially leading to AVN. A displaced hip fracture, where the broken bone fragments shift out of alignment, is a well-known and significant risk factor for developing AVN in the femoral head (the ball-shaped top of the thigh bone that fits into the hip socket). The sharp ends of the bone can sever or compress critical blood vessels that supply the femoral head. Any trauma that compromises the vascular supply to bone puts an individual at increased risk.
2. Non-Traumatic Causes: Internal Factors and Systemic Conditions
More often, AVN develops without a direct, identifiable injury. In these cases, the underlying mechanisms can be complex, multifactorial, and not always fully understood. While the exact pathophysiology remains under investigation, we know that several factors significantly increase a person’s risk of developing AVN in the absence of trauma. These include:
- Long-Term Corticosteroid Use: High-dose or prolonged use of steroid medications (like prednisone, dexamethasone, and methylprednisolone) is one of the most common non-traumatic causes of AVN. While the precise mechanism is not fully elucidated, it is believed that steroids can interfere with the body’s ability to break down fatty substances (lipids). These lipids can accumulate in the blood vessels, causing them to narrow. Steroids may also cause fat cells to enlarge, which may reduce blood flow to the bone. Additionally, steroids can affect blood clotting mechanisms. All of these factors contribute to reduced blood flow to the bone tissue.
- Excessive Alcohol Consumption: Chronic and heavy alcohol use is another significant risk factor. Similar to corticosteroids, excessive alcohol consumption is linked to the development of fatty deposits in the blood vessels, potentially leading to blockages that impede blood flow to the bone. Alcohol can also stimulate the production of cortisol, which, in excess, can have similar effects to corticosteroid use. Furthermore, chronic alcohol abuse is often associated with other underlying health problems that may independently increase the risk of AVN.
- Certain Medical Conditions: A variety of diseases can impact blood flow and increase the risk of AVN. Examples include:
- Sickle Cell Anemia: This genetic blood disorder causes red blood cells to become rigid and sickle-shaped, leading to blockages in small blood vessels and restricting blood flow to various organs, including bone.
- Systemic Lupus Erythematosus (Lupus): This autoimmune disease can cause inflammation and damage to blood vessels, increasing the risk of AVN. Lupus is also often treated with corticosteroids, compounding the risk.
- Gaucher’s Disease: This inherited metabolic disorder leads to the accumulation of fatty substances in various organs, including bone marrow, potentially disrupting blood supply to the bone.
- Pancreatitis: Inflammation of the pancreas can release enzymes into the bloodstream that damage blood vessels.
- Blood Clotting Disorders (Thrombophilias): Conditions that increase the risk of blood clot formation can lead to blockages in the small blood vessels that supply bone.
- HIV/AIDS: Both the HIV virus and some of the medications used to treat it can increase the risk of AVN.
- Medical Treatments: Certain medical treatments can inadvertently contribute to the development of AVN:
- Radiation Therapy: Radiation therapy for cancer can damage blood vessels in the treatment area, potentially impairing blood flow to the bone.
- Organ Transplantation: Organ transplantation, particularly kidney transplants, is associated with a higher incidence of AVN. This is likely due to the high-dose corticosteroids and other immunosuppressant medications used to prevent organ rejection.
- Decompression Sickness (“The Bends”): This condition, which primarily affects deep-sea divers and miners who ascend or decompress too quickly, can cause nitrogen gas bubbles to form in the blood. These bubbles can block blood flow to the bones, leading to AVN, as well as other serious complications.
- Idiopathic AVN: In a significant number of cases, despite thorough investigation, a clear and identifiable cause for AVN cannot be determined. This is referred to as “idiopathic” avascular necrosis. While the underlying mechanism remains unknown in these cases, genetic predisposition, subtle undiagnosed medical conditions, or a combination of unrecognized factors may play a role. Further research is ongoing to uncover the causes of idiopathic AVN.
The Diagnostic Journey: From Silent Damage to Clear Answers
Avascular Necrosis (AVN), also known as osteonecrosis, presents a challenging diagnostic puzzle. Often developing silently, the condition gradually damages bone tissue due to a lack of blood supply. Accurately identifying AVN requires a comprehensive approach, weaving together a detailed medical history, a careful physical examination, and, critically, the insights gleaned from advanced imaging techniques. Recognizing the often subtle and progressive nature of AVN is key to timely intervention and improved outcomes.
The symptoms of AVN typically progress through distinct stages:
- Early Stages: The Whispers of Damage: In the initial phases, AVN may be completely asymptomatic, leaving the individual unaware of the underlying process. This “silent damage” makes early detection particularly difficult. As the condition progresses subtly, a person might begin to experience mild or intermittent pain in the affected joint. This pain is often triggered by activity, weight-bearing exercises, or prolonged standing, and may subside with rest. It’s important to note that this early pain can be easily dismissed as a minor ache or strain.
- Intermediate Stages: Pain Takes Center Stage: As the blood supply continues to diminish and the bone tissue weakens, the pain becomes more constant and pronounced. It transitions from being activity-related to occurring even during periods of rest. For hip AVN, a common manifestation, the pain is frequently felt deep within the groin and may radiate down the thigh towards the knee. This radiating pain can sometimes be mistaken for other conditions, further complicating the diagnostic process.
- Late Stages: Collapse and Impairment: The defining characteristic of late-stage AVN is bone collapse. Once the structural integrity of the bone is compromised, the pain becomes severe and debilitating. The mechanics of the affected joint are significantly disrupted, leading to stiffness, a noticeably limited range of motion, and the eventual development of secondary osteoarthritis. In lower-extremity AVN, such as in the hip or knee, a limp becomes a common compensatory mechanism as the individual attempts to minimize weight-bearing on the affected joint. This limp can further contribute to pain and discomfort in other areas of the body.
Unlocking the Diagnosis: The Power of Imaging
To move from suspicion to certainty and confirm a diagnosis of AVN, physicians rely heavily on the power of imaging studies. These tools allow for a detailed visualization of the bone structure and surrounding tissues, enabling accurate assessment of the extent of the damage.
- X-rays: A Window into Structural Changes: While valuable, X-rays are often normal in the early stages of AVN, as they primarily depict changes in bone density and structure. They become most useful in later stages, where they can reveal more advanced features such as bone collapse, joint space narrowing (indicating cartilage loss), and a characteristic “crescent sign.” This crescent sign, a thin white line just under the bone surface, represents a subchondral fracture, a hallmark of AVN progression.
- MRI (Magnetic Resonance Imaging): The Gold Standard for Early Detection: MRI stands as the gold standard for diagnosing AVN, particularly in its early stages. This non-invasive imaging technique utilizes powerful magnetic fields and radio waves to create detailed cross-sectional images of the body. An MRI is capable of detecting subtle changes in bone marrow and blood supply long before any visible damage to the bone’s structure is apparent on an X-ray. This early detection capability is crucial for initiating timely treatment and potentially preventing further bone damage and collapse.
- CT Scan / Bone Scan: Complementary Tools for Comprehensive Assessment: In certain cases, a CT Scan (Computed Tomography) or a Bone Scan may be employed to provide even more detailed information. CT scans utilize X-rays to create cross-sectional images, offering a more precise visualization of bone structure compared to traditional X-rays. Bone scans, on the other hand, involve injecting a radioactive tracer into the bloodstream. This tracer accumulates in areas of increased bone activity, such as those undergoing repair. Bone scans can be helpful in identifying areas where the body is actively trying to heal the damage caused by AVN. These imaging modalities can be used in conjunction with MRI to gain a more complete understanding of the condition and guide treatment decisions.
A Staged Approach to Treatment of Avascular Necrosis (AVN)