The liver is the sole site of albumin synthesis, making it particularly vulnerable to hepatic dysfunction. In acute liver injury, albumin production decreases rapidly, though levels may not fall immediately due to its long half-life. In chronic liver disease, particularly cirrhosis, progressive impairment of synthetic function leads to persistent hypoalbuminemia.
Several mechanisms contribute to hypoalbuminemia in liver disease:
- Reduced Synthesis: Damaged hepatocytes produce less albumin, with synthesis rates dropping to as low as 20-30% of normal in advanced cirrhosis.
- Increased Loss: Portal hypertension in cirrhosis causes increased capillary permeability, allowing albumin to leak into the peritoneal cavity, contributing to ascites formation.
- Altered Distribution: The expanded plasma volume in cirrhosis dilutes circulating albumin, further lowering its concentration.
- Malnutrition: Many patients with advanced liver disease suffer from malnutrition due to reduced intake, malabsorption, and altered metabolism, exacerbating hypoalbuminemia.
Hypoalbuminemia in liver disease contributes to several complications:
- Ascites: Reduced oncotic pressure promotes fluid transudation into the peritoneal cavity.
- Edema: Peripheral and pulmonary edema result from fluid shifts into interstitial spaces.
- Coagulopathy: Albumin binds anticoagulants like heparin; low levels may contribute to bleeding tendencies.
- Drug Toxicity: Altered drug binding due to hypoalbuminemia increases free fractions of highly protein-bound medications, raising toxicity risks.
- Increased Infection Risk: Impaired immune function and reduced binding of bacterial products heighten susceptibility to infections.
Kidney Disease
In kidney disease, albumin plays a dual role as both a victim and contributor to pathology. The glomerular filtration barrier normally prevents albumin from passing into urine, but in conditions like diabetic nephropathy, glomerulonephritis, and hypertensive nephrosclerosis, this barrier becomes damaged, leading to albuminuria.
The mechanisms of albuminuria include:
- Podocyte Injury: Damage to podocytes, specialized cells in the glomerulus, disrupts the filtration barrier.
- Glomerular Basement Membrane Alterations: Changes in the composition and charge of the basement membrane increase permeability to albumin.
- Hemodynamic Factors: Intraglomerular hypertension in conditions like diabetes or hypertension stresses the filtration barrier.
- Tubular Dysfunction: Impaired reabsorption of filtered albumin by proximal tubular cells contributes to albuminuria.
Albuminuria itself contributes to kidney damage through several mechanisms:
- Tubulointerstitial Inflammation: Filtered albumin overload activates pro-inflammatory and pro-fibrotic pathways in tubular cells.
- Direct Tubular Toxicity: Albumin-bound substances like fatty acids and complement factors may damage tubular cells.
- Oxidative Stress: Increased albumin filtration promotes oxidative stress in tubular cells.
Hypoalbuminemia in kidney disease results from urinary losses and sometimes reduced synthesis due to inflammation or malnutrition. This contributes to edema formation and hyperlipidemia, as the liver increases lipoprotein production in response to low oncotic pressure.
Inflammatory Conditions
Acute and chronic inflammation profoundly affects albumin metabolism through multiple mechanisms:
- Increased Catabolism: Inflammatory cytokines like TNF-α and IL-6 accelerate albumin breakdown.
- Reduced Synthesis: The same cytokines suppress albumin gene expression in hepatocytes.
- Altered Distribution: Inflammation increases vascular permeability, allowing albumin to escape into interstitial spaces.
- Increased Loss: In conditions like sepsis or burns, capillary leak syndrome causes significant albumin loss.
This inflammatory hypoalbuminemia contributes to:
- Edema: Reduced oncotic pressure promotes fluid accumulation in tissues.
- Impaired Drug Binding: Altered protein binding affects pharmacokinetics of many medications.
- Antioxidant Deficit: Reduced albumin levels diminish antioxidant capacity, exacerbating oxidative stress.
- Nutritional Depletion: Hypoalbuminemia both reflects and contributes to malnutrition in chronic inflammatory conditions.
Cardiovascular Disease
Albumin influences cardiovascular health through several mechanisms:
- Fluid Balance: Hypoalbuminemia contributes to edema and may worsen heart failure by increasing preload.
- Vascular Function: Albumin supports endothelial health and nitric oxide signaling, affecting vascular tone.
- Lipid Metabolism: Albumin transports fatty acids and influences lipid profiles.
- Thrombosis Risk: Altered binding of anticoagulants and platelet function modulators affects coagulation.
In heart failure, hypoalbuminemia is common due to inflammation, malnutrition, and sometimes hepatic congestion. Low albumin levels correlate with worse outcomes, including increased mortality and hospitalization rates. The relationship is likely bidirectional, with heart failure contributing to hypoalbuminemia and hypoalbuminemia exacerbating cardiac dysfunction.
In atherosclerosis, albumin’s antioxidant properties may protect against LDL oxidation, while its ability to bind and remove oxidized lipids could influence plaque formation. However, the clinical significance of these effects remains under investigation.
Diabetes
Diabetes affects albumin through multiple pathways:
- Diabetic Nephropathy: Hyperglycemia damages glomeruli, leading to albuminuria and eventually hypoalbuminemia.
- Glycation: Chronic hyperglycemia promotes non-enzymatic glycation of albumin, altering its structure and function.
- Oxidative Stress: Increased oxidative stress in diabetes consumes albumin’s antioxidant capacity.
- Inflammation: Low-grade inflammation in diabetes suppresses albumin synthesis and increases catabolism.
Glycated albumin serves as a marker of intermediate-term glycemic control (reflecting the past 2-3 weeks), complementing hemoglobin A1c which reflects longer-term control. In diabetic nephropathy, albuminuria is an early marker of kidney damage and a predictor of disease progression.
Cancer
Cancer profoundly affects albumin metabolism through several mechanisms:
- Systemic Inflammation: Tumors and their microenvironment produce inflammatory cytokines that suppress albumin synthesis.
- Malnutrition: Cancer cachexia involves reduced intake, increased metabolic demands, and altered metabolism, leading to hypoalbuminemia.
- Increased Loss: Some tumors cause protein-losing enteropathy or increase vascular permeability.
- Altered Distribution: Tumor-associated inflammation promotes capillary leak.
Hypoalbuminemia in cancer correlates with:
- Poor Prognosis: Low albumin levels are associated with advanced disease and reduced survival across many cancer types.
- Treatment Toxicity: Hypoalbuminemia increases the risk of chemotherapy toxicity due to altered drug binding and distribution.
- Impaired Wound Healing: Low albumin levels compromise tissue repair after surgery or radiation.
- Reduced Treatment Efficacy: Some studies suggest hypoalbuminemia may diminish response to chemotherapy and targeted therapies.
Critical Illness
In critical illness, albumin metabolism undergoes dramatic changes:
- Capillary Leak: Systemic inflammation increases vascular permeability, causing albumin to shift into interstitial spaces.
- Accelerated Catabolism: Hypermetabolism in critical illness increases protein breakdown, including albumin.
- Reduced Synthesis: Inflammatory cytokines suppress albumin production in the liver.
- Increased Loss: In conditions like burns or pancreatitis, significant protein losses occur through exudates or drainage.
Hypoalbuminemia in critical illness contributes to:
- Edema: Reduced oncotic pressure promotes tissue edema, potentially compromising organ function.
- Hemodynamic Instability: Altered fluid distribution affects cardiac preload and afterload.
- Impaired Oxygen Delivery: Edema may increase diffusion distance for oxygen in tissues.
- Immune Dysfunction: Altered binding of immunomodulatory substances affects immune responses.
- Drug Pharmacokinetics: Changes in protein binding alter drug distribution and elimination.
Albumin as a Biomarker
Albumin’s measurement in clinical practice extends far beyond its role as a simple indicator of nutritional status. Its concentration and characteristics provide valuable information across various medical specialties, serving as a prognostic indicator, disease severity marker, and therapeutic guide.
Standard Measurement Techniques
Albumin is typically measured in serum or plasma using automated clinical chemistry analyzers. The most common methods include:
- Bromocresol Green (BCG) Method: This colorimetric technique relies on the binding of albumin to bromocresol green dye, causing a measurable color change. While widely used due to its simplicity and low cost, the BCG method may overestimate albumin levels in some cases due to binding to other proteins.
- Bromocresol Purple (BCP) Method: Similar to BCG, this method uses bromocresol purple dye, which is more specific for albumin. The BCP method is considered more accurate but may be affected by certain medications and conditions.
- Immunoassays: These techniques use antibodies specific to albumin and include methods like immunoturbidimetry and immunonephelometry. Immunoassays offer high specificity but are more expensive and complex than dye-binding methods.
- Electrophoresis: Serum protein electrophoresis separates proteins based on charge and size, allowing visualization of albumin as a distinct band. This method is particularly useful when abnormal albumin variants or paraproteins are suspected.
The choice of method depends on clinical needs, laboratory capabilities, and cost considerations. Standardization across laboratories remains a challenge, with potential variations between methods and instruments.
Albumin in Prognostic Scoring Systems
Albumin is incorporated into several validated prognostic scoring systems across different medical specialties:
- Child-Pugh Score: Used to assess prognosis in chronic liver disease, this score includes albumin levels along with bilirubin, prothrombin time, ascites, and encephalopathy. Lower albumin scores indicate worse prognosis.
- Model for End-Stage Liver Disease (MELD): Originally developed to predict mortality in patients undergoing transjugular intrahepatic portosystemic shunt (TIPS) procedures, MELD includes bilirubin, creatinine, and international normalized ratio (INR). Some variants incorporate albumin to improve predictive accuracy.
- Glasgow Prognostic Score (GPS): Used in oncology, this score combines C-reactive protein and albumin levels to predict survival in cancer patients. Elevated CRP and low albumin indicate poor prognosis.
- Prognostic Nutritional Index (PNI): Calculated from serum albumin and lymphocyte count, PNI predicts outcomes in surgical patients and those with gastrointestinal malignancies.
- Acute Physiology and Chronic Health Evaluation (APACHE): This ICU scoring system includes albumin as one component in assessing illness severity and predicting mortality.
These scoring systems demonstrate albumin’s value as a prognostic marker across diverse clinical scenarios, reflecting its role in fundamental physiological processes.
Albumin in Disease Monitoring
Serial albumin measurements provide valuable information about disease progression and treatment response:
- Liver Disease: In chronic liver disease, declining albumin levels indicate worsening synthetic function. Improvement following treatment or transplantation suggests recovery.
- Kidney Disease: In nephrotic syndrome, rising albumin levels may indicate response to therapy, while persistent hypoalbuminemia suggests ongoing protein loss.
- Inflammatory Conditions: In autoimmune diseases like rheumatoid arthritis or systemic lupus erythematosus, albumin levels may rise with successful anti-inflammatory treatment.
- Nutritional Support: In malnourished patients, increasing albumin levels over weeks to months indicate response to nutritional interventions.
- Critical Illness: In ICU patients, improving albumin levels may signal recovery from systemic inflammation and capillary leak.
The interpretation of serial measurements must consider albumin’s long half-life, with changes reflecting trends over weeks rather than days. Combining albumin with shorter half-life markers like prealbumin provides a more comprehensive view of nutritional and inflammatory status.
Novel Albumin-Based Biomarkers
Beyond total albumin concentration, researchers are exploring novel albumin-based biomarkers:
- Ischemia-Modified Albumin (IMA): This form of albumin with altered metal-binding capacity serves as a marker of myocardial ischemia. IMA rises rapidly during ischemic events and may help diagnose acute coronary syndromes.
- Glycated Albumin: Reflecting average glycemia over the past 2-3 weeks, glycated albumin complements hemoglobin A1c in diabetes management, particularly in conditions affecting red blood cell turnover.
- Oxidized Albumin: The ratio of oxidized to reduced albumin may serve as a marker of oxidative stress in conditions like diabetes, cardiovascular disease, and chronic kidney disease.
- Albumin-Corrected Calcium: Since albumin binds calcium, total calcium levels are adjusted based on albumin concentration to assess ionized calcium status more accurately.
- Urinary Albumin Excretion: Beyond total albumin concentration, the rate of albumin excretion in urine provides critical information about kidney damage in diabetes and hypertension.
These emerging biomarkers expand the clinical utility of albumin measurements, offering more specific insights into various pathological processes.
Limitations of Albumin as a Biomarker
Despite its widespread use, albumin has limitations as a biomarker that must be recognized:
- Non-Specificity: Hypoalbuminemia occurs in numerous conditions, making it non-specific for any single disease.
- Influence of Non-Nutritional Factors: Inflammation, hydration status, and liver function significantly affect albumin levels, independent of nutritional status.
- Long Half-Life: Albumin’s 20-day half-life means it reflects chronic rather than acute changes, limiting its utility in short-term monitoring.
- Methodological Variability: Different measurement techniques may yield varying results, affecting interpretation.
- Population Variability: Normal ranges may differ based on age, sex, and ethnicity, requiring appropriate reference intervals.
These limitations necessitate careful interpretation of albumin levels in context with other clinical and laboratory findings.
Therapeutic Uses of Albumin
Beyond its role as a diagnostic and prognostic marker, albumin has important therapeutic applications in medicine. The development of albumin preparations for clinical use has evolved significantly since their introduction, with ongoing research refining their indications and administration protocols.
Albumin Preparations
Therapeutic albumin is derived from human plasma through a fractionation process that involves multiple steps to ensure safety and purity:
- Source Plasma: Albumin is extracted from pooled human plasma obtained from volunteer donors.
- Fractionation: The Cohn cold ethanol fractionation process separates albumin from other plasma proteins based on solubility differences.
- Purification: Additional steps, including chromatography and filtration, remove impurities and potential pathogens.
- Stabilization: Albumin solutions are stabilized with sodium caprylate and acetyltryptophanate to prevent denaturation during heat treatment.
- Viral Inactivation/Removal: Multiple methods, including pasteurization (heating at 60°C for 10 hours), solvent-detergent treatment, and nanofiltration, inactivate or remove viruses and other pathogens.
- Formulation: Final products are available in various concentrations (typically 5%, 20%, or 25%) in isotonic saline solutions.
The rigorous manufacturing process ensures that therapeutic albumin has an excellent safety profile, with no documented cases of viral transmission since the implementation of modern viral inactivation methods.
Approved Indications
Albumin is approved for several specific indications based on clinical evidence and regulatory guidelines:
- Hypovolemia: Albumin 5% is indicated for volume expansion in hypovolemia when crystalloids are insufficient. It is particularly useful in patients requiring oncotic support.
- Hypoalbuminemia: Albumin 25% is used to raise serum albumin levels in patients with hypoalbuminemia due to inadequate production, excessive loss, or abnormal distribution.
- Burns: Albumin is indicated for burn shock management, particularly after the first 24 hours when capillary leak stabilizes.
- Liver Disease: Specific indications include spontaneous bacterial peritonitis (with antibiotics), large-volume paracentesis in cirrhotic patients, and hepatorenal syndrome (with vasoconstrictors).
- Cardiopulmonary Bypass: Albumin may be used in priming solutions for cardiopulmonary bypass circuits.
- Acute Respiratory Distress Syndrome (ARDS): In some cases, albumin with furosemide may be used for fluid management in ARDS.
- Plasma Exchange: Albumin serves as a replacement fluid in therapeutic plasma exchange procedures.
These approved indications reflect situations where albumin’s unique properties provide specific benefits beyond simple volume expansion.
Off-Label Uses
Beyond approved indications, albumin is used off-label in several clinical scenarios:
- Sepsis and Septic Shock: Albumin may be used as part of fluid resuscitation in sepsis, particularly in patients requiring large volumes of crystalloids.
- Nephrotic Syndrome: In severe cases with refractory edema, albumin infusions with diuretics may provide temporary relief.
- Pancreatitis: Some clinicians use albumin in severe acute pancreatitis to maintain oncotic pressure and potentially reduce complications.
- Ovarian Hyperstimulation Syndrome: Albumin may help reduce ascites and hematocrit in this complication of fertility treatments.
- Postoperative Care: In major surgery, albumin may be used to maintain hemodynamic stability, particularly in patients with preoperative hypoalbuminemia.
While these uses lack robust evidence from large randomized trials, they may be considered in specific clinical situations based on pathophysiological rationale and clinical experience.
Administration and Dosing
Albumin administration requires careful consideration of several factors:
- Concentration Selection:
- 5% albumin is iso-oncotic and primarily used for volume expansion.
- 25% albumin is hyperoncotic and used to raise oncotic pressure or treat hypoalbuminemia.
- Dosing:
- For hypovolemia, initial doses typically range from 250-500 mL of 5% albumin, with subsequent doses based on response.
- For hypoalbuminemia, dosing is calculated based on the desired increase in serum albumin and the patient’s plasma volume.
- Infusion Rate:
- 5% albumin can be infused rapidly in emergencies.
- 25% albumin should be infused slowly (1-2 mL/minute) to avoid rapid fluid shifts and pulmonary edema.
- Monitoring:
- Vital signs, fluid balance, and serum albumin levels should be monitored during administration.
- In patients with cardiac or renal impairment, more intensive monitoring may be necessary.
- Compatibility:
- Albumin should not be mixed with other medications or blood products.
- It is compatible with standard intravenous administration sets.
Proper administration techniques maximize therapeutic benefits while minimizing potential adverse effects.
Safety and Adverse Effects
Albumin has a favorable safety profile, but potential adverse effects include:
- Volume Overload: Rapid administration or excessive doses can cause pulmonary edema, particularly in patients with cardiac or renal impairment.
- Hypertension: Albumin may increase blood pressure due to volume expansion.
- Allergic Reactions: Rare hypersensitivity reactions, including anaphylaxis, can occur despite purification processes.
- Coagulopathy: Large volumes of albumin may dilute coagulation factors, though this is less common than with crystalloid solutions.
- Electrolyte Imbalances: Albumin preparations contain sodium, which may contribute to hypernatremia in susceptible patients.
- Alkalosis: The citrate in some albumin preparations can cause metabolic alkalosis, particularly with large volumes.
- Renal Effects: In some studies, albumin administration was associated with increased mortality in patients with traumatic brain injury, though this remains controversial.
Contraindications to albumin include severe anemia (without concurrent blood transfusion) and known hypersensitivity to albumin preparations. Caution is advised in patients with cardiac failure, renal impairment, or conditions where sodium overload is problematic.
Cost-Effectiveness Considerations
Albumin is significantly more expensive than crystalloid solutions, raising questions about cost-effectiveness:
- Volume Expansion: For simple volume expansion, crystalloids are generally more cost-effective and equally effective in most situations.
- Specific Indications: In approved indications like spontaneous bacterial peritonitis or large-volume paracentesis, albumin’s benefits justify its cost by reducing complications and hospital stays.
- Resource-Limited Settings: In environments with limited resources, the high cost of albumin may restrict its use to situations where clear benefits exist.
- Pharmacoeconomic Analyses: Studies suggest that when used appropriately, albumin may be cost-effective by reducing complications and length of stay in specific patient populations.
The decision to use albumin should balance clinical benefits against costs, considering both individual patient needs and broader healthcare resource allocation.
Albumin in Nutrition and Diet
Albumin’s relationship with nutrition is complex and multifaceted. While commonly used as a nutritional marker, albumin levels are influenced by numerous non-nutritional factors, and its role in nutritional interventions requires careful consideration.
Albumin as a Nutritional Marker
Albumin has traditionally been regarded as a key indicator of nutritional status, particularly protein nutrition. However, its utility in this role has several important nuances:
- Reflects Chronic Status: Due to its long half-life (approximately 20 days), albumin reflects nutritional changes over weeks to months rather than days. This makes it less useful for monitoring acute nutritional interventions.
- Influenced by Non-Nutritional Factors: Inflammation, liver disease, kidney disease, hydration status, and other medical conditions significantly affect albumin levels, often independent of nutritional status.
- Insensitive to Mild Deficiencies: Albumin levels may remain normal despite significant protein depletion, as the body prioritizes maintaining albumin synthesis until reserves are severely compromised.
- Better for Prognosis Than Diagnosis: While low albumin predicts poor outcomes in many conditions, it is not a sensitive or specific diagnostic tool for malnutrition.
These limitations have led to the development of more comprehensive nutritional assessment tools that incorporate albumin alongside other markers such as prealbumin, transferrin, retinol-binding protein, and anthropometric measurements.
Protein Requirements and Albumin Synthesis
Dietary protein intake directly influences albumin synthesis, though the relationship is not linear:
- Adequate Protein Intake: In healthy individuals with normal protein intake (0.8-1.0 g/kg/day), albumin synthesis matches degradation, maintaining stable levels.
- High Protein Intake: Excessive protein consumption does not significantly increase albumin synthesis beyond normal levels, as synthesis is tightly regulated by oncotic pressure and other feedback mechanisms.
- Protein Restriction: Severe protein restriction (less than 0.5 g/kg/day) gradually reduces albumin synthesis, leading to hypoalbuminemia over weeks to months.
- Essential Amino Acids: Albumin synthesis requires adequate essential amino acids, particularly branched-chain amino acids. Deficiencies in these specific amino acids can impair synthesis even with sufficient total protein intake.
- Energy Intake: Adequate calorie intake is necessary for efficient protein utilization. Inadequate energy intake leads to protein being used for energy rather than synthesis, contributing to hypoalbuminemia.
These factors highlight the importance of balanced nutrition for maintaining albumin levels, with both protein quantity and quality playing crucial roles.
Albumin in Malnutrition States
Malnutrition profoundly affects albumin metabolism through several mechanisms:
- Protein-Energy Malnutrition (PEM): In severe PEM, albumin synthesis decreases significantly due to limited substrate availability and hormonal changes. Hypoalbuminemia contributes to edema, immune dysfunction, and poor wound healing.
- Kwashiorkor: This form of PEM, characterized by adequate calorie intake but inadequate protein, typically presents with severe hypoalbuminemia and edema.
- Marasmus: In chronic calorie and protein deficiency, albumin levels may be relatively preserved initially but decline as malnutrition progresses.
- Anorexia Nervosa: Hypoalbuminemia develops in severe cases due to prolonged inadequate protein intake and may predict medical complications.
- Cancer Cachexia: This complex metabolic syndrome involves inflammation, increased energy expenditure, and muscle wasting, leading to hypoalbuminemia despite adequate intake in some cases.
In these conditions, albumin levels correlate with disease severity and prognosis, though nutritional rehabilitation requires comprehensive approaches beyond simply increasing albumin concentrations.
Nutritional Interventions and Albumin
Nutritional strategies to improve albumin levels must address underlying causes and consider the protein’s unique metabolism:
- Oral Nutritional Supplements: High-protein oral supplements can gradually increase albumin levels in malnourished patients, though effects may take weeks to become evident.
- Enteral Nutrition: Tube feeding with high-protein formulas effectively raises albumin levels in patients with functional gastrointestinal tracts.
- Parenteral Nutrition: Intravenous nutrition support can provide amino acids directly, bypassing gastrointestinal limitations. However, albumin synthesis may not normalize immediately due to underlying inflammation or other factors.
- Specific Nutrients: Certain nutrients may support albumin synthesis, including:
- Branched-chain amino acids (leucine, isoleucine, valine)
- Arginine and glutamine (conditionally essential amino acids)
- Zinc and copper (cofactors for protein synthesis)
- Vitamin B6 (involved in amino acid metabolism)
- Albumin Infusions: While intravenous albumin rapidly increases serum levels, this does not address underlying nutritional deficiencies and should not replace nutritional support.
Successful nutritional interventions require patience, as albumin levels respond slowly to dietary changes. Monitoring should include multiple parameters beyond albumin to assess overall nutritional status.
Albumin in Special Populations
Certain populations have unique considerations regarding albumin and nutrition:
- Elderly: Aging is associated with reduced albumin synthesis and increased inflammation (“inflammaging”). Older adults may require higher protein intake (1.0-1.2 g/kg/day) to maintain albumin levels and muscle mass.
- Critically Ill: In critical illness, inflammation suppresses albumin synthesis despite adequate nutrition. Aggressive protein supplementation (1.2-2.0 g/kg/day) may help mitigate losses but may not normalize levels during acute illness.
- Chronic Kidney Disease: Patients with CKD often have hypoalbuminemia due to proteinuria, inflammation, and dietary restrictions. Protein intake must balance nutritional needs against renal workload.
- Liver Disease: In cirrhosis, branched-chain amino acid supplements may improve albumin synthesis more effectively than standard protein sources.
- Post-Surgical Patients: After major surgery, increased protein requirements (1.2-1.5 g/kg/day) support wound healing and albumin synthesis, particularly in patients with preoperative hypoalbuminemia.
These populations require individualized nutritional approaches that consider their unique physiological challenges and albumin metabolism.
Dietary Sources of Albumin-Precursor Nutrients
While albumin itself is not obtained directly from diet, several nutrients support its synthesis:
- High-Quality Proteins: Animal proteins (meat, poultry, fish, eggs, dairy) provide all essential amino acids in optimal ratios for albumin synthesis. Plant proteins (legumes, grains, nuts) can also support synthesis when combined to ensure complete amino acid profiles.
- Specific Amino Acids: Foods rich in branched-chain amino acids include dairy products, meat, and legumes. Arginine is found in nuts, seeds, and meat, while glutamine is abundant in protein-rich foods and some vegetables.
- Micronutrients: Zinc (oysters, beef, pumpkin seeds), copper (shellfish, nuts, seeds), and vitamin B6 (chicken, fish, potatoes) support protein synthesis and should be included in balanced diets.
- Calories: Adequate energy from carbohydrates and fats prevents protein from being used for energy, allowing it to support albumin synthesis.
A balanced diet with sufficient high-quality protein and adequate calories provides the foundation for maintaining healthy albumin levels in most individuals.
Future Directions and Research
The study of albumin continues to evolve, with ongoing research expanding our understanding of its functions, refining its clinical applications, and exploring novel therapeutic possibilities. Several exciting developments promise to shape the future of albumin in medicine and biotechnology.
Advanced Albumin-Based Biomarkers
Research is uncovering new ways to leverage albumin’s properties for diagnostic and prognostic purposes:
- Post-Translational Modifications: Advanced mass spectrometry techniques are identifying specific modifications to albumin (such as oxidation, glycation, and cysteinylation) that may serve as early markers for diseases like diabetes, cardiovascular disease, and neurodegenerative disorders.
- Albumin-Bound Metabolites: Comprehensive profiling of molecules bound to albumin in health and disease may reveal novel biomarker panels for conditions ranging from cancer to metabolic syndrome.
- MicroRNA Carriers: Albumin binds and stabilizes microRNAs in circulation. These albumin-associated microRNAs are being investigated as potential biomarkers for various cancers and other diseases.
- Glycated Albumin Variants: Beyond total glycated albumin, specific glycation sites and patterns may provide more precise information about glycemic control and diabetic complications.
These advanced biomarkers could enable earlier disease detection, more accurate prognostication, and personalized treatment approaches.
Novel Therapeutic Applications
Albumin’s unique properties make it an attractive platform for developing new therapies:
- Drug Delivery Systems: Albumin nanoparticles and conjugates are being developed to improve drug solubility, stability, and targeting. Examples include albumin-bound paclitaxel (Abraxane) for cancer treatment and experimental formulations for antifungal and antiviral drugs.
- Half-Life Extension: Fusing therapeutic proteins to albumin or engineering albumin-binding domains can significantly extend their half-life in circulation, reducing dosing frequency for treatments like interferons, growth factors, and monoclonal antibodies.
- Recombinant Albumin: Recombinant human albumin produced in yeast, plants, or transgenic animals may offer a safer, more consistent alternative to plasma-derived albumin, reducing concerns about blood-borne pathogens.
- Albumin-Based Oxygen Carriers: Modified albumin molecules are being explored as artificial oxygen carriers for transfusion alternatives, potentially addressing blood shortages and transfusion-related complications.
These innovations could expand albumin’s therapeutic role beyond its current applications, improving treatment efficacy and safety across multiple medical fields.
Albumin in Regenerative Medicine
Emerging research suggests albumin may play important roles in tissue engineering and regenerative medicine:
- Stem Cell Culture: Albumin is a critical component in culture media for stem cells, supporting cell growth and maintaining pluripotency. Defined albumin formulations may improve consistency in stem cell manufacturing.
- Tissue Engineering Scaffolds: Albumin-based hydrogels and scaffolds are being developed for tissue engineering applications, offering biocompatibility and tunable properties for supporting cell growth and differentiation.
- Wound Healing: Albumin’s roles in maintaining oncotic pressure, binding growth factors, and modulating inflammation make it an attractive component for advanced wound dressings and healing formulations.
- Organ Preservation: Albumin solutions are being optimized for organ preservation during transplantation, potentially extending viable preservation times and improving graft function.
These applications leverage albumin’s biocompatibility and multifunctional nature to support regenerative approaches across various medical specialties.
Personalized Medicine Approaches
Advances in genomics and proteomics are enabling more personalized approaches to albumin-related care:
- Pharmacogenomics: Genetic variations in albumin structure or metabolism may influence drug binding and efficacy. Understanding these variations could help personalize drug dosing and selection.
- Albumin Phenotyping: Comprehensive characterization of albumin variants and modifications in individual patients may provide insights into disease susceptibility and progression.
- Nutrigenomics: Research into how genetic variations affect albumin metabolism could inform personalized nutritional recommendations for maintaining healthy albumin levels.
- Biomarker Panels: Combining albumin measurements with other molecular markers may create more accurate predictive models for disease risk and treatment response.
These personalized approaches could optimize albumin-related interventions based on individual patient characteristics.
Technological Innovations
New technologies are enhancing our ability to study and utilize albumin:
- Structural Biology: Advanced techniques like cryo-electron microscopy and molecular dynamics simulations are providing unprecedented insights into albumin’s structure and dynamics at atomic resolution.
- Microfluidics and Lab-on-a-Chip: Miniaturized devices are enabling rapid, point-of-care albumin testing with small sample volumes, potentially improving access to albumin measurements in resource-limited settings.
- Artificial Intelligence: Machine learning algorithms are being applied to albumin data to identify patterns predictive of disease outcomes and treatment responses.
- Synthetic Biology: Engineered albumin variants with enhanced or novel functions are being developed for research and therapeutic applications.
These technological advances promise to accelerate albumin research and translate findings more rapidly into clinical practice.
Addressing Global Health Challenges
Albumin research is also addressing pressing global health issues:
- Blood Safety: Continued improvements in albumin purification and pathogen inactivation are enhancing the safety of plasma-derived products worldwide.
- Cost Reduction: Research into more efficient production methods, including recombinant technologies, may reduce the cost of albumin products, increasing accessibility in low-resource settings.
- Alternative Indications: Exploring albumin’s potential in neglected tropical diseases and conditions prevalent in developing regions could expand its global health impact.
- Nutritional Interventions: Developing cost-effective albumin-supportive nutritional strategies could help address malnutrition in vulnerable populations worldwide.
These efforts aim to maximize albumin’s benefits while ensuring equitable access across diverse healthcare systems.
Conclusion
Albumin stands as one of the most remarkable molecules in human physiology, a true multitasker whose importance extends far beyond its abundance in blood plasma. Throughout this comprehensive exploration, we have uncovered the intricate ways in which albumin influences nearly every aspect of human health, from maintaining fluid balance and transporting essential substances to modulating immune responses and protecting against oxidative stress. Its clinical significance spans numerous medical specialties, serving as both a valuable biomarker and a therapeutic agent in diverse disease states.
The journey through albumin’s world reveals several key insights. First, albumin’s versatility stems from its unique molecular structure, which enables it to interact with countless substances while maintaining stability in the harsh environment of the bloodstream. Second, its role as a diagnostic and prognostic marker, while valuable, requires careful interpretation in context with other clinical findings, given its sensitivity to non-nutritional factors like inflammation and hydration status. Third, the therapeutic applications of albumin continue to evolve, with ongoing research refining its indications and exploring novel uses in drug delivery, regenerative medicine, and beyond.
As we look to the future, albumin research promises exciting developments that could transform medical practice. Advanced biomarkers based on albumin modifications and binding partners may enable earlier disease detection and more personalized treatment approaches. Novel therapeutic applications leveraging albumin’s biocompatibility and multifunctionality could improve drug delivery, extend the half-life of therapeutic proteins, and support regenerative medicine initiatives. Technological innovations will enhance our ability to study albumin at molecular levels and develop more accessible testing methods.
Yet, despite these advances, the fundamental importance of albumin in human health remains unchanged. This abundant multitasker continues to perform its countless essential functions silently and efficiently, sustaining life in ways we are only beginning to fully appreciate. As our understanding of albumin deepens, so too does our appreciation for the elegant complexity of biological systems and the remarkable molecules that make human life possible.
For healthcare providers, researchers, and patients alike, albumin serves as a reminder of the interconnectedness of physiological processes and the importance of looking beyond obvious symptoms to understand underlying mechanisms. By continuing to study albumin and its myriad roles, we not only advance medical science but also gain insights into the fundamental principles that govern health and disease. In the ever-evolving landscape of medicine, albumin remains a constant—a testament to nature’s ingenuity and a cornerstone of human physiology.
FAQs
- What is albumin and why is it important?
Albumin is the most abundant protein in human blood plasma, synthesized in the liver. It plays crucial roles in maintaining oncotic pressure, transporting various substances, and providing antioxidant protection. Its importance lies in its multifunctionality, supporting fluid balance, nutrient delivery, detoxification, and overall homeostasis.
- How is albumin measured in clinical practice?
Albumin is typically measured in serum or plasma using automated clinical chemistry analyzers. Common methods include the bromocresol green (BCG) and bromocresol purple (BCP) dye-binding techniques, as well as immunoassays like immunoturbidimetry. Results are reported in grams per deciliter (g/dL) or grams per liter (g/L).
- What is the normal range for albumin levels?
The normal range for serum albumin in adults is typically 3.5 to 5.0 g/dL (35 to 50 g/L). However, reference ranges may vary slightly between laboratories and can be influenced by factors such as age, sex, and pregnancy.
- What causes low albumin levels (hypoalbuminemia)?
Hypoalbuminemia can result from decreased production (liver disease, malnutrition), increased loss (kidney disease, protein-losing enteropathy, burns), altered distribution (inflammation, capillary leak syndrome), or a combination of these factors. Common causes include cirrhosis, nephrotic syndrome, severe malnutrition, and chronic inflammatory conditions.
- What are the symptoms of low albumin?
Symptoms of hypoalbuminemia include edema (swelling, particularly in legs, ankles, and abdomen), fatigue, muscle weakness, poor wound healing, and increased susceptibility to infections. In severe cases, fluid accumulation in body cavities (ascites, pleural effusions) may occur.
- Can high albumin levels be a problem?
Hyperalbuminemia (elevated albumin) is less common than hypoalbuminemia and is usually caused by dehydration, which concentrates all blood proteins. True hyperalbuminemia is rare and not typically associated with specific diseases. Treatment focuses on addressing the underlying cause, usually rehydration.
- How does albumin maintain fluid balance in the body?
Albumin maintains fluid balance primarily through its oncotic pressure effect. As the most abundant plasma protein, it attracts water and holds it within blood vessels, preventing excessive leakage into tissues. This osmotic effect is crucial for maintaining blood volume and preventing edema.
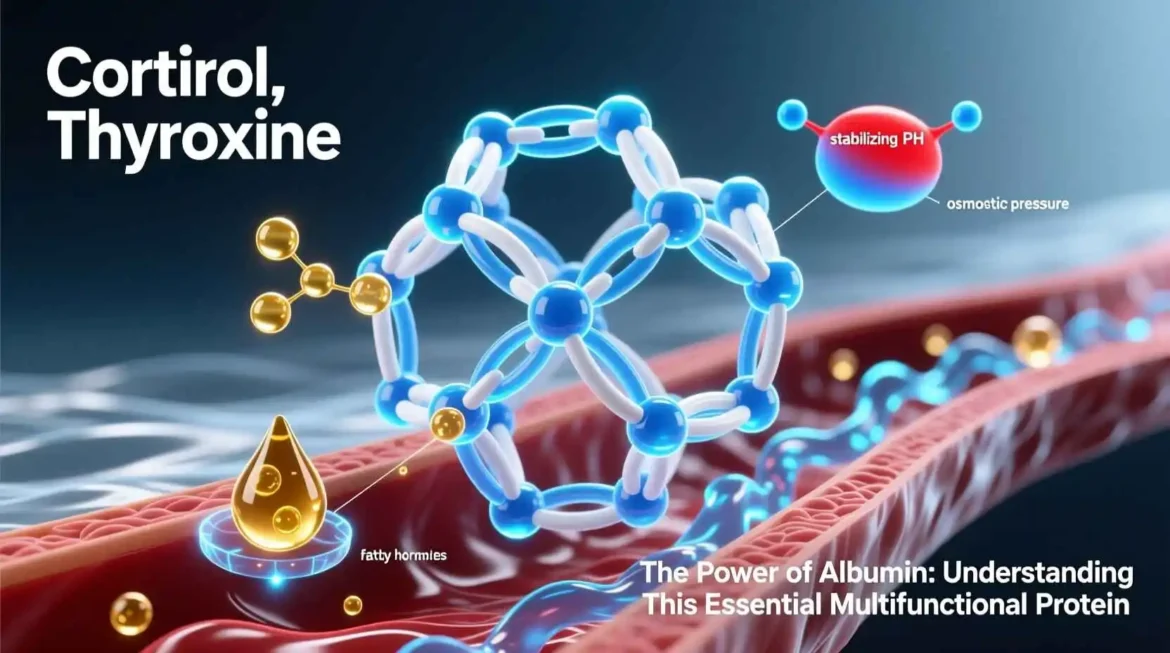
- What substances does albumin transport in the blood?
Albumin transports a wide variety of substances including fatty acids, hormones (thyroxine, cortisol, testosterone), bilirubin, metal ions (calcium, copper, zinc), drugs (antibiotics, anticoagulants), and toxins. Each albumin molecule has multiple binding sites that allow it to carry several molecules simultaneously.
- How does albumin function as an antioxidant?
Albumin acts as an antioxidant through several mechanisms: its free thiol group at cysteine-34 scavenges reactive oxygen species, it binds transition metals like copper and iron to prevent free radical formation, and it protects other molecules from oxidation by binding them.
- What is the relationship between albumin and nutrition?
Albumin is commonly used as a marker of nutritional status, particularly protein nutrition. However, its levels are influenced by multiple factors beyond nutrition, including inflammation, liver function, and kidney disease. While severe malnutrition causes hypoalbuminemia, mild to moderate deficiencies may not significantly affect albumin levels due to its long half-life.
- How is albumin used as a therapeutic agent?
Therapeutic albumin, derived from human plasma, is used for volume expansion in hypovolemia, raising oncotic pressure in hypoalbuminemia, and specific indications like spontaneous bacterial peritonitis in cirrhosis, large-volume paracentesis, and burn resuscitation. It is available in various concentrations (5%, 20%, 25%) for different clinical needs.
- What are the risks associated with albumin infusions?
Potential risks of albumin infusions include volume overload (leading to pulmonary edema), hypertension, allergic reactions (rare), coagulopathy (with large volumes), electrolyte imbalances (particularly hypernatremia), and metabolic alkalosis. Caution is advised in patients with cardiac or renal impairment.
- How does liver disease affect albumin levels?
Liver disease impairs albumin synthesis, leading to hypoalbuminemia. In cirrhosis, reduced production is compounded by increased losses due to portal hypertension and malnutrition. Albumin levels correlate with disease severity and are incorporated into prognostic scoring systems like Child-Pugh and MELD.
- What role does albumin play in kidney disease?
In kidney disease, albumin serves as both a marker and a contributor to pathology. Urinary albumin excretion indicates glomerular damage, while hypoalbuminemia results from urinary losses in nephrotic syndrome. Albuminuria itself contributes to kidney damage by promoting tubulointerstitial inflammation and oxidative stress.
- How does inflammation affect albumin levels?
Inflammation reduces albumin levels through multiple mechanisms: inflammatory cytokines suppress albumin synthesis in the liver, increase vascular permeability (shifting albumin to interstitial spaces), and accelerate catabolism. This inflammatory hypoalbuminemia occurs in conditions like sepsis, trauma, and autoimmune diseases.
- What is ischemia-modified albumin (IMA)?
Ischemia-modified albumin is a form of albumin with altered metal-binding capacity that occurs during myocardial ischemia. It serves as a biomarker for acute coronary syndromes, rising rapidly after ischemic events and potentially aiding in early diagnosis when combined with other cardiac markers.
- How does albumin affect drug metabolism and efficacy?
Albumin binds many drugs, affecting their distribution, metabolism, and elimination. Hypoalbuminemia increases the free fraction of highly protein-bound drugs, potentially enhancing their effects or toxicity. This is particularly important for drugs like warfarin, phenytoin, and NSAIDs, where dosing may need adjustment in patients with low albumin.
- What is glycated albumin and how is it used?
Glycated albumin reflects average blood glucose levels over the past 2-3 weeks, providing a shorter-term glycemic indicator than hemoglobin A1c. It is particularly useful in conditions affecting red blood cell turnover, such as hemolytic anemia or pregnancy, where A1c may be unreliable.
- How does albumin contribute to wound healing?
Albumin supports wound healing through several mechanisms: maintaining oncotic pressure to reduce edema, binding and delivering growth factors, providing antioxidant protection, and supporting immune function. Hypoalbuminemia is associated with poor wound healing and increased complication rates after surgery.
- What is the relationship between albumin and cardiovascular disease?
Albumin influences cardiovascular health through fluid balance maintenance, vascular function support, and lipid metabolism. Hypoalbuminemia is associated with worse outcomes in heart failure and coronary artery disease, reflecting both nutritional status and systemic inflammation. Albumin’s antioxidant properties may also protect against atherosclerosis.
- How does albumin function in the immune system?
Albumin exhibits immunomodulatory effects by binding and neutralizing pro-inflammatory substances, modulating leukocyte activation, and affecting cytokine production. It also binds bacterial endotoxins and other pathogen-associated molecular patterns, helping to regulate immune responses and prevent excessive inflammation.
- What is familial dysalbuminemic hyperthyroxinemia?
Familial dysalbuminemic hyperthyroxinemia is a rare inherited condition caused by mutations in the albumin gene that increase its binding affinity for thyroxine (T4). This leads to elevated total T4 levels with normal free T4 and thyroid-stimulating hormone, resulting in a euthyroid state that can be mistaken for hyperthyroidism.
- How does albumin affect calcium levels in the blood?
Approximately 40-45% of circulating calcium is bound to albumin. Changes in albumin concentration directly affect total calcium levels, though ionized (free) calcium remains relatively stable. The albumin-corrected calcium formula adjusts total calcium based on albumin concentration to estimate ionized calcium status more accurately.
- What is analbuminemia?
Analbuminemia is an extremely rare autosomal recessive disorder characterized by the absence or severe deficiency of albumin. Despite very low or undetectable albumin levels, affected individuals often have mild symptoms due to compensatory increases in other plasma proteins. This condition highlights the body’s ability to adapt to albumin deficiency.
- How does albumin influence drug dosing in clinical practice?
Albumin levels influence drug dosing, particularly for highly protein-bound medications with narrow therapeutic indices. In hypoalbuminemia, reduced protein binding increases the free fraction of drugs, potentially requiring dose adjustments to avoid toxicity. This is crucial for drugs like warfarin, phenytoin, and certain antibiotics.
- What is the role of albumin in cancer?
In cancer, albumin serves as a prognostic marker, with hypoalbuminemia correlating with advanced disease and poor survival. Cancer-related inflammation, malnutrition, and increased catabolism contribute to low albumin levels. Albumin infusions may be used in cancer patients with severe hypoalbuminemia, though they do not address underlying causes.
- How does albumin affect laboratory test results?
Albumin can influence various laboratory tests beyond its own measurement. It affects total calcium levels, hormone measurements (by binding hormones), drug levels (by altering protein binding), and colorimetric assays (by interfering with dye-binding). Laboratories often use albumin correction formulas or alternative methods to account for these effects.
- What is the difference between albumin and prealbumin?
Albumin and prealbumin (transthyretin) are both plasma proteins used as nutritional markers, but they differ significantly. Prealbumin has a shorter half-life (2-3 days vs. 20 days for albumin), making it more sensitive to acute nutritional changes. Prealbumin also binds thyroxine and retinol-binding protein, while albumin has broader transport functions.
- How does albumin function in critical care settings?
In critical care, albumin levels serve as prognostic indicators, with hypoalbuminemia associated with increased mortality and complications. Albumin may be used therapeutically in specific situations like septic shock (after initial crystalloid resuscitation), cirrhosis with complications, and large-volume paracentesis. Its use must be balanced against cost and potential risks.
- What future developments are expected in albumin research?
Future albumin research will likely focus on advanced biomarkers based on albumin modifications, novel drug delivery systems using albumin nanoparticles, recombinant albumin production, and expanded therapeutic applications in regenerative medicine. Personalized medicine approaches may use albumin characteristics to tailor treatments, while technological innovations will improve testing methods and deepen our understanding of albumin’s functions.
Disclaimer: The content on this blog is for informational purposes only. Author’s opinions are personal and not endorsed. Efforts are made to provide accurate information, but completeness, accuracy, or reliability are not guaranteed. Author is not liable for any loss or damage resulting from the use of this blog. It is recommended to use information on this blog at your own terms.