When Every Sip and Bite Becomes a Hazard: Understanding Why We Cough While Eat or Drink
We’ve all had that embarrassing moment: taking a sip of water or a bite of food, and suddenly, a violent cough erupts. It feels like the material went “down the wrong pipe.” While an occasional cough like this is normal – perhaps we swallowed too quickly or weren’t paying attention – for some of us, this happens frequently, with almost anything we consume, even just water. When this becomes a regular occurrence, it’s more than just an inconvenience; it’s our body sending a signal that something might not be working quite right with the complex process of swallowing.
We understand the frustration, the anxiety, and sometimes even the fear that can come with this experience. It makes eating and drinking, activities that should be simple and enjoyable, stressful. It’s a common concern that brings many people to seek answers. Let’s delve into why this happens, the potential causes behind it, and the ways we can manage and treat it.
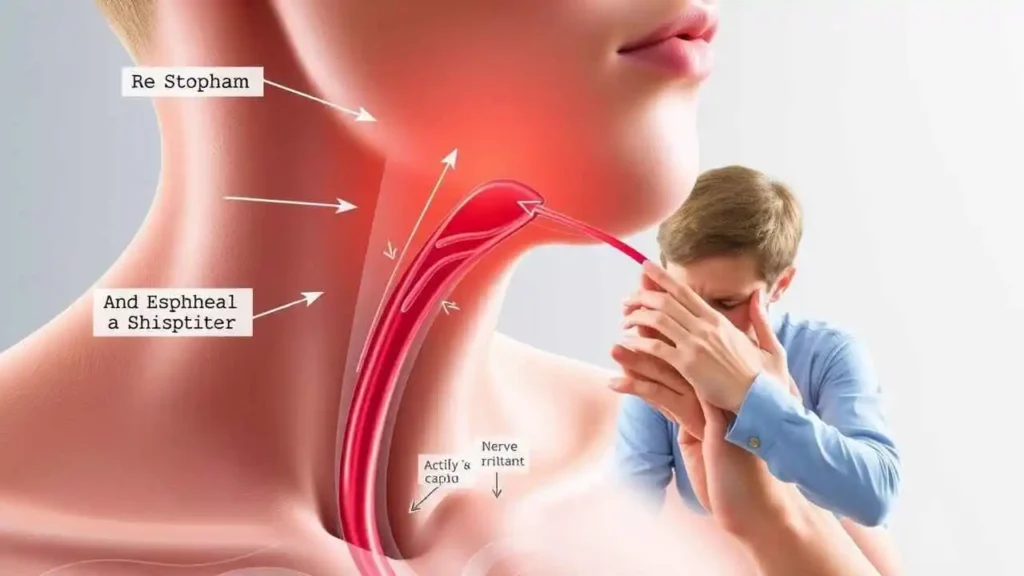
At its core, coughing while eating or drinking is often a protective reflex triggered when food, liquid, or even saliva enters the airway (trachea) instead of going down the esophagus towards the stomach. This unintended journey into the airway is called aspiration. Our body’s response is to cough forcefully to try and expel the foreign material, preventing it from reaching the lungs.
When we cough frequently during or immediately after swallowing, it suggests that our swallowing mechanism might be impaired, a condition known as dysphagia. Dysphagia can range from mild difficulty to severe problems that impact nutrition and hydration. Coughing during swallowing is a primary symptom indicating that aspiration may be occurring.
“The throat is the guardian of the gate between the air we breathe and the food we eat. When that gate falters, the simplest acts become fraught with danger.” – Inspired by acknowledging the body’s intricate design.
So, why would our body’s natural protective system, this incredible act of swallowing, suddenly falter? Many factors and underlying conditions can contribute to dysphagia and the subsequent coughing while eating or drinking. We can broadly categorize the causes:
Possible Causes of Coughing While Swallowing
| Cause Category | Examples / Associated Conditions | How it Affects Swallowing |
| Neurological Conditions | Stroke, Parkinson’s Disease, Amyotrophic Lateral Sclerosis (ALS), Multiple Sclerosis (MS), Dementia, Myasthenia Gravis | Affects the nerves and muscles controlling swallowing, leading to poor coordination or weakness. |
| Structural Issues | Esophageal Strictures (narrowing), Zenker’s Diverticulum (pouch near esophagus), Tumors (in throat, esophagus, or chest) | Obstructs the passage of food/liquid or affects the mechanics of swallowing. |
| Muscle Weakness | Aging (Presbyphagia), General Deconditioning, Muscular Dystrophy | Muscles involved in swallowing become weaker or less coordinated over time or due to disease. |
| Gastrointestinal Issues | Severe Gastroesophageal Reflux Disease (GERD), Achalasia | Reflux can irritate the airway, make it more sensitive, or even lead to aspiration of stomach contents. Achalasia affects esophageal muscle function. |
| Medication Side Effects | Sedatives, Antihistamines, Antipsychotics, certain Blood Pressure medications | Can cause drowsiness, dry mouth, or reduced muscle coordination, impacting swallowing safety. |
| Infections | Upper Respiratory Infections, Pneumonia (especially aspiration pneumonia) | Can cause inflammation or general weakness that impacts swallowing coordination. |
| Head/Neck Trauma or Surgery | Injuries to the head, neck, or throat; Post-surgical changes (e.g., after throat or esophageal surgery) | Can directly damage swallowing structures or nerves, or alter anatomy. |
| Radiation Therapy | For head/neck cancers | Can cause inflammation, scarring, and muscle stiffening over time, affecting swallowing function. |
Let’s look a little closer at some of these:
- Neurological Issues: These are very common culprits. Swallowing is a complex process involving precise coordination between the brain and numerous muscles in the mouth, throat, and esophagus. Conditions like stroke, Parkinson’s, MS, or ALS disrupt these neural signals, making it difficult to coordinate the muscle movements needed to effectively move food or liquid from the mouth to the stomach without entering the airway. Even conditions like dementia can affect the cognitive aspect of eating and swallowing safely.
- Muscle Weakness: As we age, the muscles throughout our body, including those involved in swallowing, can naturally lose some strength and flexibility. This age-related change is sometimes called presbyphagia. However, muscle weakness can also stem from general deconditioning, nutritional deficiencies, or specific muscle diseases. Weak swallowing muscles struggle to propel food downwards and protect the airway effectively.
- Structural Problems: Physical blockages or abnormalities in the throat or esophagus can impede the normal flow of food and liquid. Narrowing (strictures) from inflammation, scarring, or tumors forces swallowed material to back up or spill over into the airway. Conditions like Zenker’s Diverticulum create a pouch that can trap food, which is then aspirated later.
- Gastroesophageal Reflux Disease (GERD): While primarily affecting the stomach and esophagus, severe GERD can have significant impacts on the airway. Stomach acid can irritate the vocal cords and airways, making them hypersensitive and triggering coughs. In some cases, silent aspiration (reflux material entering the airway without a clear sensation) can occur, leading to airway irritation and chronic cough, or contribute to pneumonia.
- Medications: Many common medications list dry mouth, drowsiness, or reduced muscle coordination as side effects. While seemingly minor, these can interfere with the delicate process of swallowing safety. Reduced saliva makes forming a proper bolus difficult, while drowsiness can impair awareness and reflex timing.
When Should We Be Concerned?
Occasional coughing while swallowing is usually harmless. However, if you or someone you know experiences frequent coughing with liquids (especially water), food, or even saliva, it’s a sign that warrants medical attention. We should be particularly concerned if these symptoms are accompanied by:
- Persistent coughing after swallowing
- Feeling like food or liquid is stuck in the throat
- Wet or gurgly voice changes during or after eating/drinking
- Difficulty breathing during or after meals
- Recurrent respiratory infections or pneumonia (especially aspiration pneumonia)
- Unexplained weight loss
- Pain while swallowing
- Spitting up food or liquid (regurgitation)
Ignoring persistent coughing while swallowing can lead to serious complications, including malnutrition, dehydration, and potentially life-threatening aspiration pneumonia.
How is This Diagnosed?
If you’re experiencing these issues, the first step is to consult a doctor, ideally a primary care physician who can refer you to specialists like a neurologist, gastroenterologist, or an otolaryngologist (ENT doctor).
A key professional involved in diagnosing and managing swallowing disorders is a Speech-Language Pathologist (SLP) with expertise in dysphagia. The diagnostic process often involves:
- Clinical Swallow Examination: The doctor or SLP will take a detailed history of your symptoms, review your medical history and medications, and observe you eating and drinking different textures and consistencies. They may feel your throat while you swallow and listen to your voice and breathing.
- Instrumental Swallow Studies: If the clinical exam suggests a problem, objective tests may be performed:
- Videofluoroscopic Swallow Study (VFSS) or Modified Barium Swallow (MBS): You swallow foods and liquids mixed with barium (which shows up on X-ray) while being filmed. This allows the medical team to see exactly what happens to the material as it travels through your mouth, throat, and esophagus, and whether it enters the airway.
- Fiberoptic Endoscopic Evaluation of Swallowing (FEES): A flexible tube with a camera is passed through your nose into your throat. You are then given different foods and liquids stained with dye. The camera allows the SLP to directly visualize the swallowing structures before and after you swallow, observing residue or aspiration.
These tests help identify what is causing the problem (e.g., weak muscles, structural issue), where the problem is occurring, and what consistencies (thin liquids, thick liquids, certain food textures) are most problematic or safest.
Treatment and Management
The good news is that dysphagia and coughing while swallowing can often be managed effectively. Treatment depends on the underlying cause and the severity of the swallowing difficulty. A multidisciplinary team, often including doctors, SLPs, dietitians, and occupational therapists, may be involved. Treatment approaches include:
- Addressing the Underlying Cause:
- Treating neurological conditions with appropriate therapies and medications.
- Managing GERD with medication or lifestyle changes.
- Surgery to correct structural abnormalities or remove tumors.
- Adjusting medications that may be contributing to symptoms.
- Swallowing Therapy (Speech-Language Pathology): This is a cornerstone of dysphagia management. An SLP can teach you specific exercises and techniques to improve swallowing function:
- Strengthening Exercises: Working muscles involved in swallowing to improve their strength and range of motion.
- Coordination Exercises: Practicing sequences of swallowing movements.
- Sensory Techniques: Sometimes, stimulating the swallowing reflex can help.
- Postural Techniques: Learning specific head or body positions during swallowing (e.g., chin tuck, head turn) that can help redirect food/liquid and protect the airway.
- Dietary Modifications: This involves changing the consistency of foods and liquids to make them safer to swallow.
- Thickened Liquids: Thin liquids like water are the most common cause of aspiration. Thickening agents can be added to liquids to slow them down, making them easier to control and less likely to enter the airway. Thickening can be done to different levels (nectar-thick, honey-thick, pudding-thick).
- Modified Food Textures: Foods can be pureed, minced, or chopped finely to make them easier to chew and swallow safely. Avoiding mixed textures (like soup with chunks) might also be recommended. A dietitian can help ensure nutritional needs are met with these modifications.
- General Strategies and Tips:
- Eat and drink slowly, taking small bites or sips.
- Ensure proper positioning – sit upright at 90 degrees during meals and remain upright for at least 30 minutes afterward.
- Minimize distractions while eating (turn off the TV, put down your phone).
- Consider swallowing twice per bite or sip if recommended by your SLP.
- Maintain good oral hygiene to reduce the risk of bacteria entering the lungs if aspiration occurs.
In severe cases where aspiration is significant despite interventions, or if swallowing is unsafe for maintaining nutrition and hydration, alternative feeding methods like a feeding tube (e.g., nasogastric or gastrostomy tube) may be necessary to ensure adequate intake and prevent complications while other treatments are ongoing or if swallowing function cannot be fully restored.
Living With Swallowing Difficulties





