How Apoptosis Prevents Infection Spread: A Vital Defense Mechanism
Within the bustling metropolis of our own bodies, a silent, orderly process unfolds millions of times every second. It’s a form of cellular self-sacrifice, a pre-programmed and meticulously executed sequence that is fundamental to our health, development, and, most critically, our defense against invading pathogens. This process is called apoptosis.
Often misunderstood as just “cell death,” apoptosis is far more elegant and vital than its simple definition suggests. It’s not the chaotic, inflammatory collapse of a cell due to injury or external trauma, but rather a profoundly controlled, meticulously clean dismantling that protects the surrounding tissue from harm. Far from being a mere ending, apoptosis is an essential process of renewal and defense, a biological ballet of elimination that maintains the delicate balance within our bodies. In this article, we will embark on a fascinating journey into the microscopic world of our cells to understand precisely what apoptosis is, how this remarkable mechanism shapes us from the earliest stages of development, and how it acts as one of our most potent, albeit invisible, defenders in the constant war against infection, disease, and the insidious threat of cancer.
What is Apoptosis? The Art of Controlled Demolition
To truly grasp the profound importance of apoptosis, we must first distinguish it from its messy, violent cousin, necrosis. Imagine a building being demolished. Necrosis is like an uncontrolled explosion—the building collapses indiscriminately, sending shrapnel, debris, and dust everywhere, causing widespread damage to the surrounding area, triggering alarm bells, and necessitating an immediate, emergency response. This is precisely what happens when a cell dies from acute trauma, exposure to potent toxins, or a sudden, severe lack of oxygen. The cell membrane loses its integrity, swells dramatically, bursts open, and spills its entire contents—including potent digestive enzymes and inflammatory signals—into the extracellular space. This cellular mayhem acts as a clarion call for the immune system, triggering a robust inflammatory response intended to clear the debris but often leading to collateral damage, pain, and further tissue injury in the adjacent healthy cells.
Apoptosis, on the other hand, is like a professional demolition crew carefully taking a building apart, piece by precise piece, with surgical precision. The process is internally driven, neat, contained, and above all, silent. When a cell receives the specific signal to initiate its own demise – whether from within due to irreparable DNA damage, or from external cues like the withdrawal of growth factors or the watchful eye of the immune system identifying it as a threat – it doesn’t swell and burst. Instead, it gracefully shrinks, its internal structures are meticulously reorganized, and its DNA is precisely fragmented. The cell then precisely packages its organelles and nuclear fragments into small, membrane-bound vesicles called “apoptotic bodies.” This meticulous packaging is crucial because it ensures that no inflammatory contents are spilled. These neatly bundled packages are then swiftly recognized and engulfed by specialized “scavenger” cells, primarily macrophages, in a process known as phagocytosis. This efficient, silent cleanup ensures that the demise of one cell does not disturb its neighbors, leaving behind no trace of its removal and triggering no detrimental inflammatory response. It is a pre-programmed, energy-dependent cascade of molecular events, orchestrated by a specific set of enzymes known as caspases, which act like molecular scissors, methodically dismantling the cell’s internal architecture in an orderly fashion.
The intricate and carefully choreographed process of programmed cell death, known as apoptosis, is fundamental to the development, maintenance, and health of multicellular organisms. The key steps in this vital biological pathway are precisely orchestrated by a specific family of cysteine proteases called caspases. Once activated, these highly specific “executioner” proteins initiate an irreversible and systematic shutdown of the cell, leading to its tidy demise.
Here’s a detailed breakdown of the apoptotic sequence:
The Signal: Initiation of the Demise The apoptotic pathway is triggered when the cell receives a definitive signal, which can originate from two primary sources. An external (extrinsic) signal often comes from immune cells, such as cytotoxic T lymphocytes or natural killer cells. These cells release specific death ligands (e.g., Fas ligand, TNF-alpha) that bind to corresponding “death receptors” on the target cell’s surface, initiating a signaling cascade aimed at eliminating infected, damaged, or superfluous cells. Conversely, an internal (intrinsic) signal arises from within the cell itself, typically in response to severe cellular stress or damage. This can include irreversible DNA damage, viral infection, endoplasmic reticulum stress, withdrawal of essential growth factors, or the presence of improperly folded proteins. Both pathways ultimately converge on the activation of caspases.
Caspase Activation: The Point of No Return Once a death signal is received (either extrinsic or intrinsic), a highly regulated cascade of caspase activity begins, setting the demolition in motion. This involves the sequential activation of initiator caspases (such as Caspase-8 and Caspase-9). These initiators, once activated, in turn cleave and activate a larger pool of executioner caspases (primarily Caspase-3, Caspase-6, and Caspase-7). This amplification cascade ensures that the cell’s destruction is rapid and efficient. Executioner caspases then systematically cleave hundreds of vital cellular proteins, dismantling the cell from within.
Cellular Condensation: Internal Reorganization As the executioner caspases become active, the cell undergoes profound morphological changes. Initially, the cell begins to shrink significantly, losing volume as water is expelled. Its internal scaffolding, the cytoskeleton (composed of actin filaments, microtubules, and intermediate filaments), collapses due to the cleavage of key structural proteins by caspases. This leads to a loss of cell shape and integrity. Simultaneously, the genetic material within the nucleus undergoes remarkable changes: the chromatin condenses tightly into compact, crescent-shaped masses against the nuclear envelope (a process called pyknosis), and the DNA is fragmented into nucleosome-sized units in a very specific, orderly way (known as karyorrhexis), unlike the random degradation seen in necrosis. This precise fragmentation is carried out by enzymes like Caspase-Activated DNase (CAD), ensuring the DNA can be neatly packaged.
Membrane Blebbing: Surface Indentations Emerge Following the internal condensation, the outer membrane of the cell begins to lose its smooth appearance and protrudes outwards in numerous, irregular bulges or bubbles. This dynamic process is known as “blebbing.” Blebbing is a hallmark sign of apoptosis, resulting from the detachment of the plasma membrane from the underlying compromised cytoskeleton and the rearrangement of membrane lipids. These blebs can vary in size and number and are a visual indicator that the cell is entering its final stages of programmed death.
Formation of Apoptotic Bodies: The Clean Package The blebs continue to grow and then pinch off from the main cell body, forming smaller, discrete, membrane-enclosed fragments called apoptotic bodies. Crucially, the cell’s internal contents – including organelles and fragmented nuclear material – are neatly packaged within these intact vesicles. This meticulous packaging serves a vital purpose: it prevents any leakage of potentially inflammatory cellular components into the surrounding tissue. In stark contrast to necrosis, where cell contents spill out and cause inflammation, the formation of apoptotic bodies ensures a quiet and non-inflammatory cell disposal.
The Clean-Up Crew: Phagocytic Engulfment and Recycling The final stage of apoptosis involves the efficient removal of the apoptotic bodies. Specialized immune cells, primarily professional phagocytes like macrophages and dendritic cells, or even neighboring healthy cells, act as the “clean-up crew.” They recognize specific “eat me” signals exposed on the surface of the apoptotic bodies (such as phosphatidylserine, which is normally on the inner leaflet of the membrane but flips to the outer leaflet during apoptosis). Upon recognition, these phagocytes rapidly engulf the apoptotic bodies, internalizing them into vesicles called phagolysosomes, where their components are degraded and recycled. The entire process is completed without eliciting an immune response or leaving a trace of damage or inflammation, maintaining tissue homeostasis.
The understanding of programmed cell death has revolutionized biology and medicine, offering insights into development, disease progression, and therapeutic strategies. As Sydney Brenner, Nobel laureate whose seminal work on C. elegans was pivotal in understanding programmed cell death, wisely stated, “Progress in science depends on new techniques, new discoveries and new ideas, probably in that order.” The detailed elucidation of apoptosis exemplifies this progression, from initial observations to the molecular mechanisms and their profound implications.
Apoptosis in Our Body’s Grand Design: Beyond Infection Control
While its critical role in clearing infected cells or regulating immune responses is a primary focus, it is essential to appreciate that apoptosis – or programmed cell death – is an indispensable cornerstone of our normal physiology, orchestrating the intricate processes fundamental to life itself. Far from being a chaotic event, apoptosis is a highly controlled, precise, and orderly cellular dismantling process that is vital for the health and integrity of our body.
From our earliest moments of development, apoptosis serves as a master sculptor, meticulously shaping our very form. During embryonic development (morphogenesis), it is apoptosis that undertakes the purposeful pruning of tissues to create the complex structures of organs and limbs. For instance, the transient webbing of tissue between our fingers and toes in the womb is precisely removed by apoptosis, allowing for the formation of individual, distinct digits. Similarly, it plays a crucial role in forming the intricate network of our nervous system and the creation of lumens (openings) within various organs.
Beyond this initial developmental phase, apoptosis continually serves as a master regulator of tissue homeostasis, ensuring a dynamic and essential balance between cellular proliferation (cell creation) and cellular elimination (cell removal). This constant fine-tuning is vital for maintaining the optimal function and architecture of all our tissues.
Tissue Maintenance and Renewal: In tissues characterized by high turnover rates, such as the epithelial lining of our gut (intestine) or our epidermis (outer skin layer), old, worn-out, or senescent cells are constantly being replaced. Apoptosis is the elegant and efficient mechanism that cleanly and quietly removes these old cells without triggering an inflammatory response, making way for the precise integration of new, healthy cells. This continuous process ensures tissue integrity, efficient function, and prevents the accumulation of damaged or aged cells that could impair organ performance.
Removing Damaged or Potentially Malignant Cells: Cells are constantly exposed to various stressors, including environmental toxins, UV radiation, and even errors during DNA replication. If a cell’s DNA is damaged beyond the body’s repair mechanisms, apoptosis is swiftly triggered to eliminate it. This crucial function acts as a primary biological defense mechanism against cancer. By removing cells with irreparable genetic mutations, apoptosis prevents them from becoming uncontrolled and potentially cancerous. It serves as an internal quality control system, safeguarding the organism from the proliferation of abnormal cells.
Immune System Regulation and Tolerance: Apoptosis is fundamental to the proper functioning and regulation of our immune system. After an infection has been successfully cleared, apoptosis is utilized to prune the vast majority of immune cells (lymphocytes) that proliferated to fight the pathogen, ensuring that the immune system returns to a resting state and preventing chronic inflammation or over-activity. More critically, during their development in the thymus and bone marrow, immune cells that are “self-reactive” – meaning they could mistakenly attack the body’s own healthy tissues – are identified and eliminated through apoptosis. This process, known as clonal deletion, is essential for establishing immune tolerance and preventing debilitating autoimmune diseases such as lupus or type 1 diabetes.
In essence, apoptosis is not merely a mechanism of cell death, but a sophisticated process of cellular control and renewal that is absolutely fundamental to life, growth, and the ongoing maintenance of our complex biological systems. It is, truly, a cornerstone of our body’s grand design.
The Frontline Defense: Apoptosis – An Elegant Strategy in Infection Control
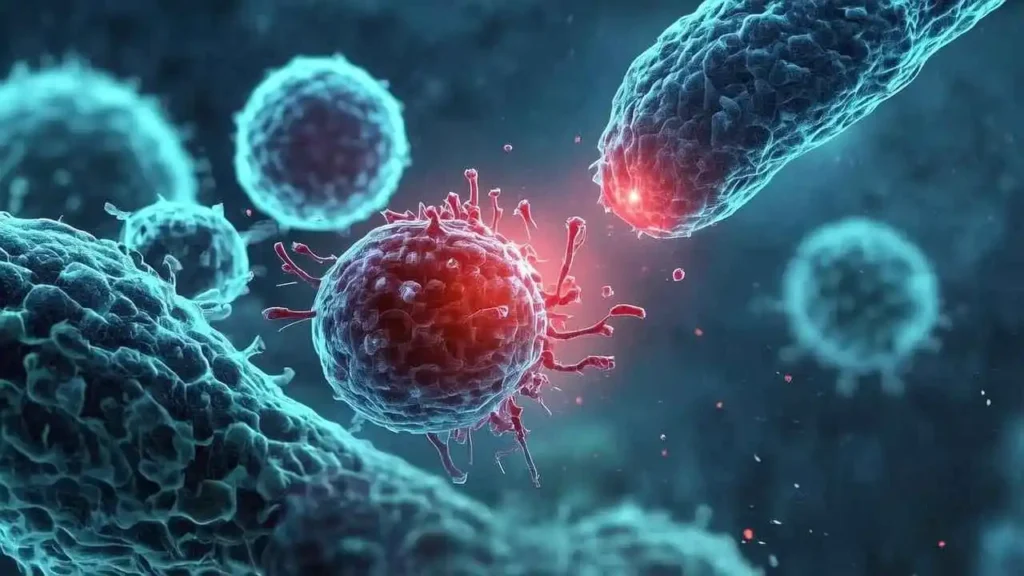
When an unwanted guest, particularly a pathogen like a virus, successfully invades our complex biological territory, its primary imperative is replication. Viruses, being obligate intracellular parasites, lack their own machinery for this crucial process. Therefore, their survival hinges entirely on their ability to hijack a host cell’s intricate metabolic pathways, ribosomes, and energy resources. It is precisely at this critical juncture that apoptosis, or programmed cell death, emerges as an extraordinarily powerful and often decisive antiviral and antimicrobial strategy. Far from a chaotic demise, apoptosis is a precisely orchestrated form of cellular altruism; the infected cell consciously and systematically sacrifices itself, not out of weakness, but for the greater good of the entire organism, preventing the pathogen’s spread and safeguarding the surrounding healthy tissues.
The Intricate Mechanism of Self-Sacrifice
Here’s a more detailed look at how this vital defense mechanism unfolds:
Upon viral infection, the host cell becomes a factory for the pathogen, rapidly churning out viral proteins, enzymes, and nucleic acids (DNA or RNA) – components that are inherently foreign to the uninfected cell. Our cells are equipped with sophisticated internal surveillance systems, collectively known as pattern recognition receptors (PRRs), strategically located within the cytoplasm and various organelles. These molecular sentinels, such as RIG-I, MDA5, and certain intracellular Toll-like receptors (TLRs), are specifically designed to detect these anomalous viral signatures – be it double-stranded RNA (a common viral intermediate), viral capsids, or even nascent viral proteins.
This detection acts as an urgent “danger signal,” signaling profound cellular stress and triggering a cascade of events that culminate in the activation of the intrinsic apoptotic pathway. This pathway is primarily regulated by the mitochondria. Upon receiving the danger signal, pro-apoptotic proteins (part of the Bcl-2 family) become activated, leading to mitochondrial outer membrane permeabilization. This crucial step results in the release of cytochrome c and other pro-apoptotic factors from the mitochondria into the cytoplasm. Cytochrome c then binds to Apaf-1, forming a complex known as the apoptosome, which in turn activates initiator caspases (like caspase-9). These initiator caspases then activate executioner caspases (such as caspase-3 and -7), which are the ultimate architects of cellular dismantling.
The Dual Goals: Halting Spread and Preventing Inflammation
By initiating its own destruction through this precise enzymatic process, the infected cell essentially commits suicide before the virus has had a chance to complete its replication cycle, assemble new infectious viral particles (virions), and egress from the cell. The executioner caspases meticulously break down the cell’s internal structures, causing the cell to shrink, its chromatin to condense, and its plasma membrane to form characteristic blebs, eventually fragmenting into smaller, membrane-bound sacs known as apoptotic bodies. Crucially, these apoptotic bodies cleanly encapsulate the partially formed viruses, viral components, and any cellular debris within their intact membranes.
This “clean up” strategy achieves two critical, interconnected goals:
It Stops Viral Egress and Spread: The virus is effectively trapped and eliminated within these contained apoptotic bodies before it can mature, burst out of the cell (a process called lysis), and spread to infect neighboring healthy cells. This prevents the exponential growth of the viral load and limits tissue damage. It’s a proactive measure that sacrifices one cell to save thousands.
It Avoids Widespread Inflammation and Tissue Damage: Unlike necrosis (uncontrolled cell death resulting from severe injury), which causes the cell to swell and burst, releasing its contents into the extracellular space, apoptosis is an immunologically “silent” process. Necrotic cells release a plethora of cellular contents, including damage-associated molecular patterns (DAMPs), which trigger a vigorous inflammatory response characterized by the recruitment of immune cells like neutrophils, contributing to widespread tissue damage, scarring, and potentially systemic inflammation. In contrast, the clean, membrane-bound apoptotic bodies display “eat me” signals (like phosphatidylserine on their surface), prompting their swift and efficient engulfment by professional phagocytes (such as macrophages and dendritic cells) in a process called efferocytosis. This rapid and orderly removal prevents the release of inflammatory cellular contents, thereby minimizing collateral tissue damage and maintaining immune homeostasis.
Beyond Viruses: A Broader Antimicrobial Role
While particularly pronounced and well-studied in viral infections due to the virus’s obligate intracellular lifestyle, this crucial mechanism isn’t limited to controlling viruses. Some intracellular bacteria, such as Mycobacterium tuberculosis (the causative agent of tuberculosis), Listeria monocytogenes, and certain Salmonella species, also reside and replicate within host cells. When these bacteria threaten the cell’s integrity or are detected by intracellular surveillance systems, the host cell can likewise undergo apoptosis. This traps the bacteria inside the apoptotic bodies, presenting them in a contained package for swift disposal by phagocytes, thus preventing their intracellular proliferation and subsequent spread.
In essence, apoptosis is an elegant and indispensable component of the innate immune response, an act of cellular selflessness that stands as a fundamental cornerstone in our body’s continuous battle against infectious invaders.
The Cellular Arms Race: When Pathogens Fight Back
Indeed, for millennia, pathogens have been locked in an intricate co-evolutionary dance with their hosts, constantly adapting to evade or subvert our sophisticated defense mechanisms. One of the most critical of these host defenses is apoptosis, or programmed cell death, a meticulous process the body uses to eliminate compromised or infected cells. However, the selective pressure exerted by this defense has driven remarkable ingenuity in the microbial world. Many viruses, for instance, have evolved highly specialized genes that express proteins specifically engineered to inhibit or manipulate the host cell’s apoptotic machinery.
These viral countermeasures can take various forms: they might directly block the crucial activation of caspases (the ‘executioner’ enzymes of apoptosis), mimic host anti-apoptotic proteins like Bcl-2, or interfere with the complex intracellular signaling pathways – both intrinsic and extrinsic – that culminate in cell death. The ultimate goal for the virus is clear: by disarming the cellular suicide program, they can prolong the life of the infected cell, transforming it into a clandestine ‘replication factory’ where countless new viral particles can be synthesized, assembled, and released before the cell’s demise, thereby maximizing viral propagation and ensuring their continued survival and spread.
This dynamic interplay establishes a fascinating and high-stakes “arms race” at the cellular and molecular level. On one side, the host’s immune system, particularly cytotoxic T lymphocytes and Natural Killer (NK) cells, actively seeks out and identifies infected cells, deploying signals that activate the apoptotic cascade, effectively sacrificing a few cells to save the whole. On the other side, the cunning virus deploys its anti-apoptotic arsenal, striving to keep its cellular sanctuary alive and productive. The delicate balance and ultimately, the outcome of this cellular tug-of-war, profoundly dictate the trajectory and severity of an infection. If the host’s pro-apoptotic mechanisms prevail, infection can be contained, viral load kept low, and symptoms minimized or even entirely absent. Conversely, if the viral counter-strategies successfully suppress apoptosis, the virus can replicate unchecked, leading to widespread tissue damage, increased viral shedding, and often, more severe or persistent disease. Understanding the intricate mechanics of this cellular battle is crucial, not only for comprehending disease pathogenesis but also for identifying novel therapeutic targets to tip the scales in favor of the host.
Apoptosis vs. Necrosis: A Tale of Two Endings
At a fundamental cellular level, life and death are not simple binaries. Cells don’t just “turn off”; they die through specific, and vastly different, processes. These two processes, while both culminating in the cessation of cellular function, unfold through vastly different mechanisms and carry profoundly distinct implications for the organism. To truly crystallize the difference between these two forms of cell death, let’s compare them side-by-side, highlighting their triggers, mechanisms, and ultimate consequences. Understanding this distinction is not just an academic exercise; it is key to appreciating the elegance and paramount importance of apoptosis in maintaining health, and the destructive nature of necrosis in disease.
Apoptosis: The Programmed, Orchestrated Exit
Imagine a cell performing a deliberate, internal decision to end its life for the greater good of the organism – a cellular “suicide” that is controlled, orderly, and beneficial. This is apoptosis, also known as Programmed Cell Death (PCD).
Triggered By: Internal signals (e.g., DNA damage, developmental cues, viral infection, aging) or external signals from other cells. It’s an active, energy-dependent process, requiring the cell to expend energy to execute its own demise.
The Process: Apoptosis is a highly regulated, systematic dismantling of the cell.
The cell shrinks, becoming smaller and denser.
Its chromatin (DNA) condenses and aggregates, often fragmenting into neatly packaged pieces.
The cell membrane begins to bleb – forming small, bubble-like protrusions.
Eventually, the cell fragments into multiple, membrane-bound “apoptotic bodies,” each containing intact organelles and nuclear fragments.
The Outcome: These apoptotic bodies are swiftly recognized and engulfed by phagocytic cells (like macrophages) before their contents spill out into the surrounding tissue. Crucially, this clean-up process is non-inflammatory. It’s a tidy, quiet exit that prevents damage to neighboring cells and maintains tissue homeostasis. Apoptosis is vital for embryonic development (e.g., removing webbing between fingers and toes), normal tissue turnover (e.g., shedding intestinal lining cells), immune system regulation (e.g., removing self-reactive immune cells), and eliminating potentially harmful cells (e.g., cancerous or virally infected cells). It’s the body’s way of ensuring quality control and proper development.
Necrosis: The Accidental, Catastrophic Rupture
Now, picture a cell subjected to overwhelming external trauma, a violent and uncontrolled death that leaves a mess in its wake. This is necrosis, often described as a cellular “homicide.”
Triggered By: Severe, unphysiological injury, such as acute trauma, lack of blood supply (ischemia), extreme temperatures, toxins, or overwhelming infection. It is a passive process, often occurring because the cell’s energy-producing machinery has failed.
The Process: Necrosis is a chaotic and destructive sequence of events.
The cell swells significantly due to uncontrolled ion and water influx.
Organelles within the cell, particularly mitochondria, also swell and become dysfunctional.
The cell membrane loses its integrity, becoming leaky and eventually rupturing.
This rupture leads to the uncontrolled release of the cell’s internal contents – including enzymes, cellular debris, and inflammatory mediators – into the extracellular space.
The Outcome: The spillage of intracellular material into the surrounding tissue triggers a robust and often damaging inflammatory response. This inflammation is the body’s attempt to clear the debris and repair the injury, but it can also cause further damage to adjacent healthy cells. Necrosis is always a pathological process, contributing to tissue damage in conditions like heart attacks (myocardial infarction), strokes, burns, and gangrene. It signifies severe cellular stress and injury.
The Stark Contrast: Cleanliness vs. Chaos
The contrast between apoptosis and necrosis could not be starker. Apoptosis is a precisely choreographed cellular ballet, a controlled and beneficial self-removal, leaving no trace and causing no collateral damage. Necrosis, on the other hand, is a chaotic eruption, a violent and messy demise that triggers inflammation and can perpetuate tissue injury.
Understanding this distinction is not merely an academic exercise. It is fundamental to comprehending the intricate balance of cellular life and death, guiding our understanding of health and disease. From embryonic development and the ongoing maintenance of tissues to the progression of cancers, autoimmune disorders, and various forms of organ damage, recognizing whether cells are undergoing an elegant, programmed exit or a destructive, accidental rupture is pivotal for diagnosis, prognosis, and the development of targeted therapies. It illuminates the astonishing sophistication of cellular life – and death – and underscores the pivotal role of programmed cell death in maintaining the delicate balance essential for health.
| Feature | Apoptosis (Programmed Cell Death) | Necrosis (Uncontrolled Cell Death) |
| Stimulus | Programmed physiological or pathological cues (e.g., development, DNA damage, infection) | Acute injury, trauma, lack of blood supply, toxins |
| Cellular Appearance | Cell shrinks, chromatin condenses, membrane blebs | Cell swells and becomes leaky |
| Plasma Membrane | Remains intact until the final stages; forms apoptotic bodies | Ruptures early, spilling cellular contents |
| DNA Breakdown | Orderly, non-random fragmentation into specific sizes | Random and diffuse degradation |
| Inflammation | No significant inflammatory response | Significant inflammatory response, tissue damage |
| Physiological Outcome | Clean removal of single cells by phagocytes; no tissue scarring | Affects groups of cells; leads to tissue damage and scarring |
Conclusion: The Unsung Hero of Cellular Health
As we have seen, apoptosis is far more than a simple end; it is a vital, dynamic mechanism woven into the very fabric of our existence. It is the sculptor of our developing form, the janitor that keeps our tissues clean and functional, and a vigilant guardian that stands ready to sacrifice individual cells to protect the entire organism from infection and cancer.
By understanding this quiet, controlled process, we gain a deeper appreciation for the profound complexity and resilience of the human body. Apoptosis is the unsung hero working tirelessly in the background, ensuring that life, at both the cellular and organismal level, can continue in an orderly, healthy, and protected manner. It is a beautiful testament to the idea that sometimes, a controlled ending is the key to a new beginning.
FAQs
1.What is apoptosis?
Apoptosis is a programmed cell death process that enables the removal of damaged or unnecessary cells without causing inflammation.
2. How does apoptosis help in fighting infections?
Apoptosis eliminates infected cells, thereby preventing pathogens from replicating and spreading within the body.
3. What triggers apoptosis during an infection?
Apoptosis can be triggered by various signals, including cytokines, DNA damage, and recognition of pathogens by immune cells, such as T-cells.
4. Can all cells undergo apoptosis?
Most cells can undergo apoptosis, but some, like certain stem cells and germ cells, have specific mechanisms to regulate their death.
5. What are the key proteins involved in the apoptosis process?
Key proteins include caspases, Bcl-2 family proteins, and death receptors, each contributing to the regulation and execution of apoptosis.
6. How can apoptosis be detected in a laboratory setting?
Techniques include flow cytometry, TUNEL assay, and Annexin V staining to recognize early apoptosis markers.
7. What is the difference between apoptosis and necrosis?
Apoptosis is a controlled, energy-dependent process that avoids inflammation, while necrosis is an uncontrolled cell death often leading to inflammation.
8. How does dysregulation of apoptosis impact health?
When apoptosis is dysregulated, it can lead to diseases; excessive apoptosis contributes to neurodegenerative diseases, while insufficient apoptosis may lead to cancer.
9. What role does apoptosis play in cancer progression?
Cancer cells often evade apoptosis, allowing them to survive and proliferate uncontrollably, making apoptosis a target for cancer therapies.
10. Can apoptosis influence autoimmune diseases?
Yes, inadequate apoptosis of immune cells can contribute to autoimmunity, allowing the immune system to attack the body’s own tissues.
11. What impact does aging have on apoptosis?
Aging may alter the regulation of apoptosis, leading to increased cell survival and contributing to age-related diseases.
12. How do viruses interfere with apoptosis?
Many viruses have evolved mechanisms to inhibit apoptosis, which allows them to persist and replicate within the host cell.
13. What is the relationship between apoptosis and inflammation?
Apoptosis helps regulate inflammation by removing immune cells after they are no longer needed, minimizing tissue damage and chronic inflammation.
14. How does the immune system utilize apoptosis?
The immune system employs apoptosis to eliminate infected cells and maintain homeostasis by clearing out excess immune cells after an infection resolves.
15. What are common biomarkers indicating apoptosis?
Common biomarkers include cytochrome c release from mitochondria and exposure of phosphatidylserine on the outer membrane of cells.
16. Can therapies induce apoptosis in cancer cells?
Yes, various cancer therapies, including chemotherapy and targeted therapies, aim to induce apoptosis in cancer cells.
17. What role does apoptosis play in tissue homeostasis?
Apoptosis removes excess cells and damaged cells, maintaining a balanced cell population and proper tissue function.
18. Is there a link between apoptosis and chronic diseases?
Yes, dysregulation of apoptosis is associated with chronic diseases such as diabetes, heart disease, and Parkinson’s disease.
19. How does nutrition affect apoptosis?
Certain nutrients and dietary compounds can influence apoptosis pathways and may enhance the capacity of cells to undergo apoptosis when necessary.
20. Are there drugs that can promote apoptosis?
Some drugs, including certain nonsteroidal anti-inflammatory drugs (NSAIDs) and retinoids, can promote apoptosis in specific contexts.
21. What happens if apoptosis is overly active in the body?
Excessive apoptosis can lead to tissue loss and contribute to conditions like neurodegeneration and ischemic damage.
22. Do all infections promote apoptosis?
Not all infections induce apoptosis; some pathogens can evade it and persist, while others trigger robust apoptotic responses.
23. How is apoptosis related to the development of therapeutic vaccines?
Therapeutic vaccines aim to stimulate immune responses that include apoptosis of infected or cancerous cells, improving treatment efficacy.
24. How do antioxidants influence apoptosis?
Antioxidants can protect cells from oxidative stress and modulate apoptosis, potentially preventing unnecessary cell death.
25. What role does apoptosis play in embryonic development?
Apoptosis is crucial during embryonic development for shaping organs and removing unnecessary cells, contributing to normal organogenesis.
26. Can exercise influence apoptosis?
Regular physical activity may enhance the apoptotic response in immune cells, promoting better clearance of infected or damaged cells.
27. How do genetic factors influence apoptosis?
Genetic mutations and polymorphisms can affect apoptosis pathways, altering susceptibility to diseases and treatment responses.
28. Are there therapies aimed at modulating apoptosis?
Yes, researchers are exploring therapies that can either inhibit or enhance apoptosis to treat a variety of diseases, including cancer and autoimmune disorders.
29. Is there a future for using apoptosis in genetic therapies?
Future therapies may involve using gene editing to influence apoptotic pathways as a strategy to treat diseases by selectively eliminating harmful cells.
30. What is the significance of apoptosis in the context of public health?
Understanding apoptosis can lead to novel therapeutic strategies and preventive measures for infectious diseases, cancer, and chronic conditions, ultimately improving public health outcomes.
Medical Disclaimer:
The information provided on this website is for general educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always
seek the advice of your physician or other qualified health provider with any questions you may have
regarding a medical condition. Never disregard professional medical advice or delay in seeking it
because of something you have read on this website.




