Complete Guide to Arthritis Diagnosis: Tests and Procedures Explained
Arthritis is a term that encompasses more than 100 different conditions affecting the joints and surrounding tissues, causing pain, stiffness, and reduced mobility. As one of the leading causes of disability worldwide, arthritis affects people of all ages, genders, and backgrounds. This comprehensive guide explores the various types of arthritis, their causes, symptoms, diagnostic approaches, and natural prevention strategies through lifestyle modifications and remedies.
The Complex World of Arthritis
Arthritis is not a single disease but a complex group of musculoskeletal disorders characterized by inflammation and degeneration of joints. The word arthritis comes from the Greek words “arthro” (joint) and “itis” (inflammation), highlighting the inflammatory nature of many forms of the condition. While commonly associated with aging, arthritis can affect individuals at any stage of life, including children.
The impact of arthritis extends far beyond joint pain. It can significantly affect quality of life, limiting daily activities, reducing work productivity, and impacting mental health. According to the World Health Organization, more than 350 million people worldwide live with arthritis, with millions more experiencing early symptoms or at risk of developing the condition.
Understanding the different types of arthritis is crucial for proper management and treatment. Each type has distinct characteristics, causes, and progression patterns, requiring tailored approaches to care and lifestyle adjustments.
Types of Arthritis
The diverse family of arthritis conditions can be broadly categorized into inflammatory and non-inflammatory types, though some forms exhibit characteristics of both categories.
Osteoarthritis (OA)
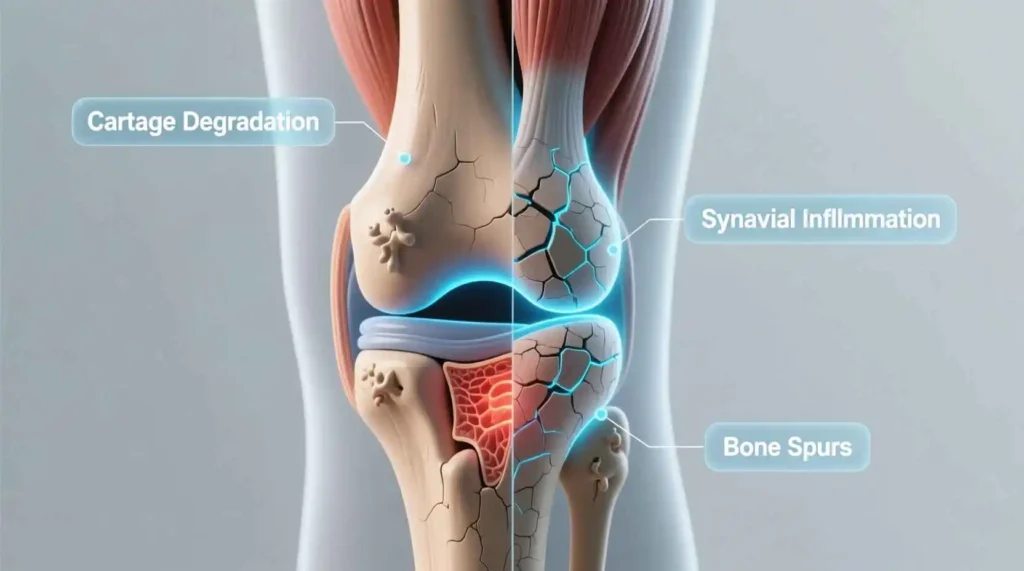
Osteoarthritis, often referred to as “wear-and-tear” arthritis, is the most common form of arthritis, affecting millions of people worldwide. This degenerative joint disease occurs when the protective cartilage that cushions the ends of bones wears down over time, leading to bone rubbing against bone.
OA primarily affects weight-bearing joints such as the knees, hips, spine, and hands. The condition typically develops gradually and worsens over time, causing pain, stiffness, and reduced flexibility. Unlike inflammatory forms of arthritis, OA is not an autoimmune condition but rather a result of mechanical stress and biological changes in the joint.
Risk factors for osteoarthritis include age, obesity, joint injuries, genetics, and occupations that place repetitive stress on specific joints. While OA was once considered an inevitable part of aging, research now shows that it’s a complex interplay of mechanical, metabolic, and inflammatory factors.
Rheumatoid Arthritis (RA)
Rheumatoid arthritis is a chronic autoimmune disorder that primarily affects the joints. In RA, the immune system mistakenly attacks the synovium, the lining of the membranes that surround the joints. This attack causes inflammation that thickens the synovium, eventually destroying cartilage and bone within the joint.
Unlike osteoarthritis, RA typically affects joints symmetrically—if one knee is affected, the other knee is likely affected as well. The condition can also affect other body systems, including the skin, eyes, lungs, heart, and blood vessels.
RA often begins in smaller joints, such as those in the hands and feet, before progressing to larger joints. The disease follows a pattern of flares (periods of increased disease activity) and remissions (periods of reduced symptoms). Women are two to three times more likely than men to develop RA, and the condition usually begins between ages 30 and 60.
Psoriatic Arthritis (PsA)
Psoriatic arthritis is a form of inflammatory arthritis that affects some people with psoriasis, an autoimmune skin condition characterized by red, scaly patches. PsA can develop at any time, but it most commonly appears between ages 30 and 50, often about 10 years after the onset of psoriasis.
This type of arthritis can affect any joint in the body and tends to affect joints asymmetrically. PsA can cause distinctive symptoms such as sausage-like swelling of fingers and toes (dactylitis), foot pain at the points where tendons and ligaments attach to bones (enthesitis), and lower back pain due to inflammation in the sacroiliac joints.
Psoriatic arthritis exists on a spectrum, with some individuals experiencing mild symptoms while others develop severe joint damage. The condition can also affect other body parts, including the nails, eyes, and cardiovascular system.
Ankylosing Spondylitis (AS)
Ankylosing spondylitis is a type of arthritis that primarily affects the spine, though it can involve other joints as well. AS is characterized by inflammation of the spinal joints (vertebrae) that can lead to severe, chronic pain and discomfort. Over time, the inflammation can cause the vertebrae to fuse together, resulting in a rigid spine and a stooped posture.
AS typically begins in early adulthood, with symptoms often appearing between ages 17 and 45. Men are more likely to develop AS than women, and there appears to be a genetic component, as many people with AS have the HLA-B27 gene.
In addition to spinal symptoms, AS can cause inflammation in other parts of the body, including the eyes (uveitis), heart, and lungs. Early diagnosis and treatment are crucial to prevent permanent spinal damage and maintain mobility.
Gout
Gout is a form of inflammatory arthritis caused by the accumulation of urate crystals in joints, resulting from high levels of uric acid in the blood. This condition often manifests as sudden, severe attacks of pain, swelling, redness, and tenderness in the joints, frequently starting in the big toe.
Gout affects men more often than women, though women’s risk increases after menopause. Risk factors for gout include diet (particularly consumption of purine-rich foods like red meat and seafood), obesity, certain medications, family history, and medical conditions like high blood pressure and diabetes.
Without treatment, gout can lead to chronic arthritis, tophi (lumps of urate crystals under the skin), and kidney stones. The condition follows a pattern of acute flares followed by periods of remission, though some individuals may develop chronic gout with persistent symptoms.
Juvenile Arthritis (JA)
Juvenile arthritis is an umbrella term for autoimmune and inflammatory conditions that develop in children under the age of 16. The most common type is juvenile idiopathic arthritis (JIA), which has several subtypes including oligoarthritis, polyarthritis, systemic arthritis, and enthesitis-related arthritis.
Children with JA experience similar symptoms to adults with arthritis, including joint pain, swelling, stiffness, and reduced mobility. However, JA can also affect growth and development, potentially causing growth abnormalities in affected joints.
The causes of JA are not fully understood, but research suggests a combination of genetic predisposition and environmental triggers. Early diagnosis and treatment are essential to minimize joint damage, preserve growth potential, and maintain quality of life for affected children.
Other Forms of Arthritis
Beyond the more common types, numerous other forms of arthritis exist, each with unique characteristics:
- Lupus (Systemic Lupus Erythematosus): An autoimmune disease that can affect joints, skin, brain, lungs, kidneys, and blood vessels.
- Fibromyalgia: A condition characterized by widespread musculoskeletal pain, fatigue, sleep, memory, and mood issues.
- Reactive Arthritis: Develops in response to an infection in another part of the body, often in the intestines, genitals, or urinary tract.
- Septic Arthritis: Caused by a bacterial or fungal infection inside a joint, requiring prompt medical treatment.
- Polymyalgia Rheumatica: An inflammatory disorder causing muscle pain and stiffness, particularly in the shoulders and hips.
- Thumb Arthritis: A common form of osteoarthritis affecting the joint at the base of the thumb.
Causes and Risk Factors for Arthritis
The development of arthritis involves a complex interplay of genetic, environmental, and lifestyle factors. While the specific causes vary depending on the type of arthritis, several common risk factors contribute to the development and progression of the condition.
Genetic Factors
Genetics play a significant role in many forms of arthritis. Certain genetic variations can increase susceptibility to specific types of arthritis or influence disease severity:
- Family history is a known risk factor for osteoarthritis, rheumatoid arthritis, gout, and ankylosing spondylitis.
- The HLA-B27 gene is strongly associated with ankylosing spondylitis and other spondyloarthropathies.
- Specific genetic markers have been identified that increase the risk of rheumatoid arthritis, particularly in individuals with a family history of the disease.
- Genetic variations affecting cartilage structure and metabolism can influence the development of osteoarthritis.
While genetics can predispose individuals to arthritis, they rarely tell the whole story. Environmental factors and lifestyle choices often interact with genetic susceptibility to trigger disease onset.
Age and Gender
Age is one of the most significant risk factors for many types of arthritis:
- Osteoarthritis risk increases with age as cartilage naturally wears down over time.
- Rheumatoid arthritis can occur at any age but is most common between ages 30 and 60.
- Ankylosing spondylitis typically begins in early adulthood, with symptoms often appearing between ages 17 and 45.
- Gout risk increases with age, particularly in men over 40 and postmenopausal women.
Gender also influences arthritis risk:
- Women are more likely than men to develop rheumatoid arthritis, lupus, and fibromyalgia.
- Men are more likely to develop gout and ankylosing spondylitis.
- Osteoarthritis affects both genders, though women are more likely to develop it after age 50.
Joint Injury and Overuse
Physical stress on joints can contribute to the development of arthritis, particularly osteoarthritis:
- Previous joint injuries, such as those sustained in sports or accidents, increase the risk of developing arthritis in the affected joint later in life.
- Occupations that involve repetitive motions, heavy lifting, or prolonged standing can place excessive stress on joints, accelerating cartilage breakdown.
- Athletic activities that involve high-impact or repetitive joint stress may increase arthritis risk, particularly if injuries occur.
- Obesity places additional stress on weight-bearing joints like knees and hips, accelerating cartilage degeneration.
Autoimmune Factors
In autoimmune forms of arthritis, the immune system mistakenly attacks healthy tissues, leading to inflammation and joint damage:
- Rheumatoid arthritis occurs when the immune system attacks the synovium, the lining of the joints.
- In psoriatic arthritis, both skin and joint tissues are targeted by the immune system.
- Lupus is a systemic autoimmune disease that can affect multiple organs, including joints.
- The exact triggers for autoimmune responses in arthritis are not fully understood but likely involve a combination of genetic susceptibility and environmental factors.
Metabolic Factors
Metabolic abnormalities can contribute to certain types of arthritis:
- Gout results from elevated levels of uric acid in the blood, which can form crystals in joints.
- Diabetes and obesity are associated with an increased risk of osteoarthritis, possibly due to inflammatory processes and mechanical stress on joints.
- Hemochromatosis, a condition of iron overload, can lead to a specific type of arthritis.
- Pseudogout is caused by the accumulation of calcium pyrophosphate crystals in joints, often associated with metabolic changes in aging.
Environmental Triggers
Various environmental factors may trigger or exacerbate arthritis:
- Infections can trigger reactive arthritis or initiate autoimmune responses in susceptible individuals.
- Smoking is a known risk factor for rheumatoid arthritis and can worsen disease progression.
- Certain occupations involving exposure to silica or other mineral dusts may increase arthritis risk.
- Climate and weather conditions can influence arthritis symptoms, though they do not cause the disease.
Lifestyle Factors
Several lifestyle choices can influence arthritis risk and progression:
- Obesity significantly increases the risk of developing osteoarthritis, particularly in weight-bearing joints.
- Physical inactivity can lead to muscle weakness and reduced joint stability, potentially accelerating arthritis development.
- Poor nutrition can contribute to inflammation and inadequate tissue repair.
- Chronic stress may exacerbate inflammation and pain perception in arthritis.
Symptoms of Arthritis
Arthritis symptoms vary depending on the type of arthritis, the joints affected, and the severity of the condition. However, several common symptoms characterize most forms of arthritis, though their presentation and intensity can differ significantly among individuals.
Joint Pain
Pain is the most common and often the most debilitating symptom of arthritis. The characteristics of arthritis pain can provide clues about the type and severity of the condition:
- In osteoarthritis, pain typically worsens with activity and improves with rest. It often starts gradually and increases over years.
- Rheumatoid arthritis pain is often described as throbbing or aching and is usually worse in the morning and after periods of inactivity.
- Gout pain is typically sudden and severe, often described as the worst pain ever experienced. It commonly affects the big toe but can occur in other joints.
- Inflammatory arthritis pain often improves with gentle activity but worsens with prolonged inactivity.
- Pain may be localized to specific joints or widespread, depending on the type of arthritis.
Joint Stiffness
Stiffness is another hallmark symptom of arthritis, particularly in the morning or after periods of inactivity:
- Morning stiffness lasting less than 30 minutes is more characteristic of osteoarthritis.
- Morning stiffness lasting more than an hour is more typical of inflammatory arthritis like rheumatoid arthritis.
- Stiffness after sitting for extended periods (gelling) is common in many forms of arthritis.
- Stiffness may improve with gentle movement and activity in inflammatory forms of arthritis.
Swelling and Inflammation
Joint swelling is a visible sign of inflammation and is more prominent in inflammatory forms of arthritis:
- Rheumatoid arthritis often causes visible swelling, warmth, and redness in affected joints.
- In osteoarthritis, swelling may be less pronounced and is often due to bone spurs or fluid accumulation.
- Gout typically causes intense swelling, redness, and warmth in the affected joint during acute attacks.
- Swelling in psoriatic arthritis may be accompanied by the characteristic skin changes of psoriasis.
- Persistent swelling can lead to joint deformity over time if left untreated.
Reduced Range of Motion
Arthritis can limit the normal movement of affected joints:
- Difficulty bending or straightening joints completely is common in many forms of arthritis.
- In osteoarthritis, reduced range of motion often develops gradually as cartilage wears away.
- Inflammatory arthritis may cause more rapid loss of joint mobility due to inflammation and tissue damage.
- Joint contractures (permanent bending of joints) can occur in advanced or untreated arthritis.
- Reduced range of motion can significantly impact daily activities and quality of life.
Fatigue
Fatigue is a common but often overlooked symptom of arthritis, particularly in inflammatory forms:
- In rheumatoid arthritis and other inflammatory conditions, fatigue results from the body’s inflammatory response and the energy required to manage chronic pain.
- Fatigue in arthritis can be debilitating, affecting work performance, social activities, and overall quality of life.
- Sleep disturbances due to pain can contribute to fatigue in arthritis patients.
- Fatigue may fluctuate with disease activity, worsening during flares and improving during remissions.
- Managing fatigue often requires a comprehensive approach addressing both physical and emotional aspects.
Systemic Symptoms
Some forms of arthritis can affect the entire body, causing symptoms beyond the joints:
- Rheumatoid arthritis can cause fever, weight loss, and inflammation in other organs like the eyes, lungs, and heart.
- Lupus, a systemic autoimmune condition, can cause a characteristic butterfly rash on the face, hair loss, and kidney problems.
- Psoriatic arthritis may be accompanied by skin lesions, nail changes, and eye inflammation.
- Ankylosing spondylitis can cause inflammation in the eyes (uveitis), heart, and lungs.
- Gout can lead to kidney stones and tophi (urate crystal deposits under the skin).
Joint Deformities
Over time, persistent inflammation and joint damage can lead to visible changes in joint structure:
- In rheumatoid arthritis, joint deformities such as swan-neck deformity (hyperextension of the middle joint of the finger with flexion of the end joint) and boutonnière deformity (flexion of the middle joint with hyperextension of the end joint) can develop.
- Osteoarthritis may cause bony enlargements called Heberden’s nodes (at the end joints of fingers) and Bouchard’s nodes (at the middle joints of fingers).
- Severe ankylosing spondylitis can lead to fusion of the spine, resulting in a stooped posture.
- Chronic gout can cause tophi, which are lumps of urate crystals that can deform joints.
Numbness and Tingling
Some forms of arthritis can compress nerves, leading to neurological symptoms:
- Cervical spine arthritis can cause compression of the spinal cord or nerve roots, leading to numbness, tingling, or weakness in the arms and legs.
- Carpal tunnel syndrome, which can be associated with rheumatoid arthritis, causes numbness and tingling in the hands and fingers.
- Peripheral neuropathy can occur in conditions like lupus, causing numbness and tingling in the extremities.
Diagnosis of Arthritis
Diagnosing arthritis involves a comprehensive evaluation that includes medical history, physical examination, laboratory tests, and imaging studies. Early and accurate diagnosis is crucial for implementing appropriate treatment strategies and preventing joint damage.
Medical History
A detailed medical history is the foundation of arthritis diagnosis. Healthcare providers will ask about:
- Symptom onset, duration, and progression
- Specific joints affected and the pattern of involvement
- Character and severity of pain, stiffness, and swelling
- Factors that worsen or improve symptoms
- Morning stiffness duration and its effect on daily activities
- Family history of arthritis or autoimmune conditions
- Previous joint injuries or surgeries
- Occupational and recreational activities that may stress joints
- Other medical conditions and medications
- Presence of systemic symptoms like fever, weight loss, or fatigue
The pattern of symptoms can provide important clues about the type of arthritis. For example, symmetric joint involvement is more typical of rheumatoid arthritis, while asymmetric involvement may suggest psoriatic arthritis or gout.
Physical Examination





