Blood Plasma: The Unsung Hero of Your Body’s Life Support System
Introduction
Blood plasma, the often-overlooked component of our circulatory system, serves as the liquid foundation upon which our body’s complex transportation network operates. This straw-colored fluid, constituting approximately 55% of our total blood volume, is far more than a simple medium for carrying blood cells. It is a sophisticated biological solution teeming with proteins, nutrients, hormones, and waste products, all working in concert to maintain homeostasis and support life.
The history of plasma research dates back to the early 20th century when scientists first began to separate blood into its constituent components. This discovery revolutionized medicine, paving the way for transfusion therapies and countless life-saving treatments. Today, plasma stands at the forefront of biomedical research and therapeutic development, offering hope to patients with rare diseases, immune deficiencies, and traumatic injuries.
In this comprehensive exploration of blood plasma, we will journey through its intricate composition, vital functions, medical applications, and the fascinating science behind plasma-derived therapies. We will also address common questions and misconceptions about this remarkable biological fluid that sustains life itself.
The Composition of Blood Plasma
At first glance, blood plasma appears to be a simple, yellowish liquid. However, this seemingly straightforward substance is actually a complex biochemical solution of remarkable sophistication. Understanding its composition provides insight into its numerous functions and medical applications.
Water: The Primary Component
Water constitutes approximately 92% of plasma volume, serving as the solvent in which all other plasma components are dissolved or suspended. This high water content is essential for several reasons. First, it provides the fluid medium necessary for blood flow through the vascular system. Second, water’s excellent solvent properties allow it to dissolve a wide range of substances, enabling the transport of nutrients, hormones, and waste products throughout the body. Third, water’s high heat capacity helps regulate body temperature by absorbing and distributing heat.
The water in plasma is not static but constantly exchanged with water in the body’s tissues through the processes of filtration and reabsorption at capillary beds. This dynamic equilibrium ensures that plasma volume remains relatively constant despite variations in water intake and loss.
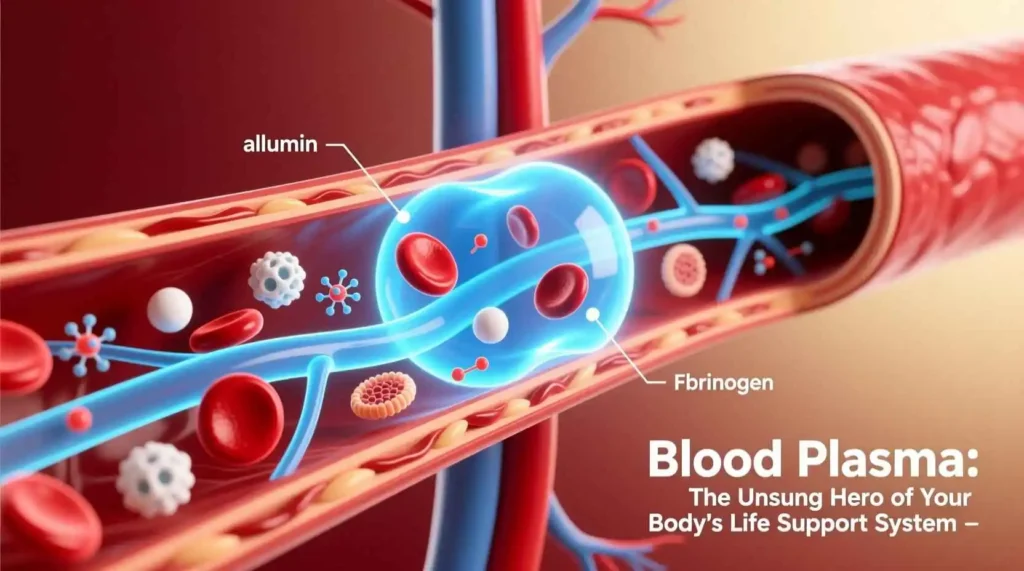
Plasma Proteins: The Multifunctional Workhorses
Plasma proteins make up about 7% of plasma volume and are perhaps the most functionally diverse components. These macromolecules are synthesized primarily in the liver, with the exception of gamma globulins (antibodies), which are produced by plasma cells derived from B lymphocytes. The major plasma proteins include albumin, globulins, and fibrinogen, each serving distinct and vital functions.
Albumin: The Abundant Multitasker
Albumin is the most abundant plasma protein, accounting for approximately 60% of the total plasma protein content. This versatile molecule, produced exclusively by the liver, performs several critical functions:
- Osmotic Regulation: Albumin is primarily responsible for maintaining the colloid osmotic pressure (oncotic pressure) of blood. This pressure prevents excessive fluid from leaking out of capillaries into the surrounding tissues. Without adequate albumin, fluid would accumulate in tissues, causing edema—a condition characterized by swelling, particularly in the extremities and abdomen.
- Transport Function: Albumin serves as a carrier for numerous substances that are poorly soluble in water. It binds and transports fatty acids, hormones (such as thyroid hormones and cortisol), bilirubin (a waste product from hemoglobin breakdown), calcium, and various drugs. This transport function is essential for the distribution of these substances throughout the body and their eventual delivery to target tissues or elimination organs.
- Buffering Capacity: Albumin contributes to the blood’s buffering capacity, helping to maintain the acid-base balance within a narrow pH range. This buffering action is crucial because even slight deviations from normal blood pH can disrupt cellular function and lead to serious health consequences.
- Antioxidant Properties: Albumin possesses antioxidant properties, helping to neutralize harmful free radicals in the bloodstream. This protective function helps prevent oxidative damage to cells and tissues throughout the body.
The liver produces approximately 12 grams of albumin daily, and under normal conditions, the human body contains about 250-300 grams of this vital protein. Albumin has a relatively long half-life of approximately 20 days, which contributes to the stability of plasma oncotic pressure.
Globulins: The Diverse Protectors and Transporters
Globulins constitute approximately 35% of plasma proteins and are divided into three main categories: alpha, beta, and gamma globulins. Each subgroup serves distinct functions in the body.
Alpha Globulins: These proteins include several important molecules such as alpha-1-antitrypsin (which protects tissues from enzymes released by inflammatory cells), alpha-1-acid glycoprotein (an acute-phase protein that increases during inflammation), and alpha-2-macroglobulin (a large protein that inhibits various enzymes). Alpha globulins also include binding proteins for hormones and other substances.
Beta Globulins: This group includes transferrin (which transports iron), beta-lipoproteins (which transport lipids), and complement components (which participate in immune responses). Beta globulins also include plasminogen, a precursor to plasmin, an enzyme that dissolves blood clots.
Gamma Globulins: Also known as immunoglobulins or antibodies, these proteins are produced by plasma cells (derived from B lymphocytes) in response to foreign substances (antigens). Gamma globulins are essential for the adaptive immune response, providing specific defense against pathogens. There are five classes of immunoglobulins:
- IgG: The most abundant antibody in blood and tissue fluids, IgG provides long-term protection against pathogens. It can cross the placenta, providing passive immunity to the fetus.
- IgA: Found primarily in mucosal secretions such as saliva, tears, and breast milk, IgA provides localized immune protection at body surfaces.
- IgM: The largest antibody, IgM is the first antibody produced during an initial immune response. It is particularly effective at activating the complement system.
- IgD: Present in small amounts in blood, IgD functions primarily as a receptor on B cells.
- IgE: Involved in allergic reactions and defense against parasitic infections, IgE binds to mast cells and basophils, triggering the release of inflammatory mediators.
The production of gamma globulins is a dynamic process that increases in response to infection or vaccination. This adaptability allows the immune system to respond effectively to a wide range of pathogens.
Fibrinogen: The Clotting Catalyst
Fibrinogen, also known as Factor I, is a large glycoprotein that plays a central role in blood clotting (coagulation). Produced by the liver, fibrinogen constitutes approximately 4% of plasma proteins. When blood vessels are damaged, a complex cascade of reactions is initiated, culminating in the conversion of fibrinogen to fibrin by the enzyme thrombin.
Fibrin molecules polymerize to form long, insoluble strands that create a mesh-like structure at the site of injury. This fibrin mesh traps platelets and blood cells, forming a clot that stops bleeding and provides a scaffold for tissue repair. Once healing is complete, the fibrinolytic system breaks down the fibrin mesh through the action of plasmin, restoring normal blood flow.
Fibrinogen is also an acute-phase protein, meaning its levels increase in response to inflammation, tissue injury, or infection. Elevated fibrinogen levels are associated with an increased risk of cardiovascular disease, as they can promote blood clot formation and contribute to atherosclerosis.
Other Plasma Components
Beyond the major proteins, plasma contains numerous other substances essential for bodily functions:
Electrolytes: These ionized minerals include sodium, potassium, calcium, magnesium, chloride, bicarbonate, and phosphate. Electrolytes are crucial for maintaining fluid balance, nerve conduction, muscle contraction, and acid-base equilibrium. The precise concentrations of these ions are tightly regulated by hormones such as aldosterone, parathyroid hormone, and calcitonin, as well as by the kidneys.
Nutrients: Plasma transports various nutrients absorbed from the digestive system, including glucose (the primary energy source for cells), amino acids (building blocks for proteins), lipids (fats and cholesterol), and vitamins. These nutrients are delivered to cells throughout the body for energy production, growth, and maintenance.
Hormones: Endocrine glands secrete hormones directly into the bloodstream, where they are transported by plasma to their target tissues. Hormones such as insulin, glucagon, cortisol, thyroid hormones, and reproductive hormones regulate numerous physiological processes, including metabolism, growth, stress response, and reproduction.
Waste Products: Plasma carries waste products generated by cellular metabolism to organs of excretion. These include urea and creatinine (nitrogenous waste products excreted by the kidneys), bilirubin (a breakdown product of hemoglobin excreted by the liver), and carbon dioxide (transported to the lungs for elimination).
Gases: Plasma contains dissolved gases, primarily oxygen and carbon dioxide. Although most oxygen is transported by hemoglobin in red blood cells, a small amount dissolves directly in plasma. Carbon dioxide is transported in three forms: dissolved in plasma, as bicarbonate ions, and bound to hemoglobin.
Functions of Blood Plasma
The composition of plasma directly relates to its diverse functions in the body. These functions are essential for maintaining homeostasis and supporting life.
Maintaining Blood Volume and Pressure
Plasma plays a critical role in maintaining blood volume and pressure through several mechanisms:
- Osmotic Pressure: The proteins in plasma, particularly albumin, create colloid osmotic pressure that draws water into the vascular system. This pressure counteracts the hydrostatic pressure that pushes fluid out of capillaries, maintaining a balance that prevents excessive fluid accumulation in tissues.
- Fluid Balance: Plasma serves as a reservoir for water that can be shifted between the bloodstream and tissues as needed. When the body becomes dehydrated, water moves from tissues into the bloodstream to maintain blood volume. Conversely, when fluid intake is excessive, the kidneys excrete the excess water to maintain proper blood volume.
- Blood Pressure Regulation: The volume of plasma directly affects blood pressure. When plasma volume decreases, blood pressure drops, triggering compensatory mechanisms such as increased heart rate, vasoconstriction, and the release of hormones like renin and aldosterone, which work to restore blood volume and pressure.
Transportation of Substances
Plasma serves as the body’s primary transportation medium, carrying a wide variety of substances to and from different tissues:
- Nutrient Delivery: After absorption from the digestive system, nutrients are transported in the plasma to cells throughout the body. Glucose, fatty acids, amino acids, vitamins, and minerals are all delivered to cells for energy production, growth, and maintenance.
- Waste Removal: Metabolic waste products generated by cells are carried in the plasma to organs of excretion. The kidneys filter urea, creatinine, and other waste products from the plasma, while the liver processes bilirubin and other toxins for elimination.
- Hormone Transport: Hormones secreted by endocrine glands are transported in the plasma to their target tissues, where they exert their effects. Some hormones bind to specific carrier proteins in plasma, which prolongs their half-life and regulates their availability to tissues.
- Gas Exchange: Although most oxygen is carried by hemoglobin in red blood cells, plasma transports dissolved oxygen and carbon dioxide between the lungs and tissues. Carbon dioxide is particularly soluble in plasma, where it is converted to bicarbonate ions for efficient transport.
Immune Function
Plasma plays a crucial role in both innate and adaptive immunity:
- Antibody Transport: The gamma globulins (antibodies) in plasma provide specific immune defense against pathogens. These antibodies recognize and neutralize foreign invaders, marking them for destruction by other components of the immune system.
- Complement System: Plasma contains complement proteins that form part of the innate immune system. When activated, these proteins work together to destroy pathogens directly, enhance phagocytosis, and promote inflammation.
- Cytokine Transport: Plasma transports signaling molecules called cytokines, which coordinate immune responses by facilitating communication between immune cells. These molecules help regulate inflammation, fever, and the activation of various immune functions.
Blood Clotting
The coagulation system, which prevents excessive bleeding after injury, relies heavily on plasma components:
- Clotting Factors: Plasma contains numerous clotting factors (proteins) that interact in a cascade to form blood clots. These factors include fibrinogen, prothrombin, and various other proteins that are activated in sequence when blood vessels are damaged.
- Fibrin Formation: The conversion of fibrinogen to fibrin is the final step in the coagulation cascade. Fibrin strands form a mesh that traps platelets and blood cells, creating a stable clot that stops bleeding.
- Regulatory Proteins: Plasma also contains proteins that regulate the clotting process, preventing excessive clot formation that could lead to thrombosis. These regulatory proteins include antithrombin, protein C, protein S, and tissue factor pathway inhibitor.
Temperature Regulation
Plasma contributes to the body’s temperature regulation through several mechanisms:
- Heat Distribution: The high water content of plasma allows it to absorb and distribute heat throughout the body. This helps maintain a uniform body temperature and prevents localized overheating.
- Heat Dissipation: When the body needs to cool down, blood vessels near the skin surface dilate, increasing blood flow to the skin. The water in plasma can then release heat to the environment through radiation, convection, and evaporation.
- Sweat Production: Plasma provides the water that is secreted as sweat, which evaporates from the skin surface to cool the body. During sweating, plasma volume decreases, triggering thirst mechanisms that encourage fluid intake to restore plasma volume.
Acid-Base Balance
Plasma helps maintain the body’s acid-base balance within a narrow pH range (approximately 7.35-7.45):
- Buffering Systems: Plasma contains several buffering systems that neutralize acids and bases, preventing significant changes in pH. The bicarbonate buffer system is particularly important, with bicarbonate ions in plasma reacting with hydrogen ions to form carbonic acid, which then breaks down into carbon dioxide and water.
- Protein Buffers: Plasma proteins, especially albumin, contribute to buffering capacity by accepting or releasing hydrogen ions as needed to maintain pH balance.
- Electrolyte Balance: The precise regulation of electrolyte concentrations in plasma helps maintain proper pH. For example, the kidneys regulate bicarbonate and hydrogen ion concentrations to compensate for acid-base disturbances.
Plasma Collection and Processing
The collection and processing of plasma are critical steps in making this valuable biological resource available for medical and research purposes. These processes require specialized equipment, rigorous protocols, and careful attention to safety and quality control.
Plasmapheresis: The Collection Process
Plasmapheresis is the procedure used to collect plasma from donors. This process separates plasma from blood cells, allowing the cells to be returned to the donor while the plasma is collected for further processing. The plasmapheresis procedure involves several steps:
- Donor Screening: Before donation, potential donors undergo a screening process to ensure they meet eligibility criteria. This includes a health history questionnaire, physical examination, and tests for certain infectious diseases.
- Venipuncture: A trained phlebotomist inserts a needle into a vein in the donor’s arm, typically in the antecubital fossa (the inner elbow area). The needle is connected to tubing that leads to the plasmapheresis machine.
- Blood Separation: The plasmapheresis machine draws whole blood from the donor and separates it into its components using centrifugation or filtration methods. The heavier blood cells (red blood cells, white blood cells, and platelets) are separated from the lighter plasma.
- Plasma Collection: The separated plasma is collected into a sterile collection bag, while the blood cells are mixed with an anticoagulant solution to prevent clotting.
- Return of Blood Cells: The blood cells, along with the anticoagulant solution, are returned to the donor through the same needle or a needle in the opposite arm. This process continues until the target plasma volume is collected, typically 600-800 milliliters per donation.
- Completion and Post-Donation Care: Once the target plasma volume is collected, the needle is removed, and pressure is applied to the puncture site to prevent bleeding. Donors are typically advised to rest briefly and consume fluids and snacks to replenish their volume.
The entire plasmapheresis process usually takes about 90 minutes, significantly longer than a whole blood donation. However, because the blood cells are returned to the donor, individuals can donate plasma more frequently than whole blood—up to twice in a seven-day period with at least one day between donations, according to current guidelines.
Plasma Storage and Preservation
After collection, plasma must be properly stored and preserved to maintain its quality and therapeutic properties:
- Freezing: Fresh plasma is typically frozen within 24 hours of collection to preserve the activity of labile clotting factors. When frozen within 8 hours of collection, it is designated as Fresh Frozen Plasma (FFP). When frozen between 8 and 24 hours after collection, it is labeled as Plasma Frozen Within 24 Hours (PF24).
- Storage Temperature: Plasma is stored at temperatures below -18°C (0°F), with many facilities maintaining temperatures at -30°C (-22°F) or lower. These freezing temperatures preserve the activity of plasma proteins and prevent microbial growth.
- Thawing: When needed for transfusion, frozen plasma is thawed in a controlled water bath at 30-37°C (86-99°F). Thawed plasma should be used within 24 hours if stored at 1-6°C (34-43°F) or within 5 days if stored at room temperature.
- Quality Control: Throughout storage and handling, plasma is subject to rigorous quality control measures, including visual inspection for abnormalities, testing for infectious diseases, and monitoring of storage conditions.
Plasma Fractionation
Plasma fractionation is the industrial process of separating plasma into its individual protein components. This complex process involves several steps:
- Thawing and Pooling: Frozen plasma units are thawed and pooled together to create large batches for processing. Pooling allows for the efficient production of plasma derivatives while diluting any potential contaminants that might be present in individual units.
- Fractionation Methods: Several methods are used to separate plasma proteins, including:
- Cohn Process: This cold ethanol fractionation method, developed by Edwin Cohn during World War II, uses varying concentrations of ethanol, temperature, and pH to precipitate different protein fractions sequentially.
- Chromatography: Various chromatographic techniques, including ion exchange, affinity, and size exclusion chromatography, are used to separate proteins based on their physical and chemical properties.
- Membrane Filtration: Ultrafiltration and other membrane-based techniques are used to separate proteins based on their molecular size.
- Purification and Viral Inactivation: After initial separation, each protein fraction undergoes further purification steps to remove impurities. Additionally, viral inactivation or removal steps are implemented to ensure the safety of plasma-derived products. These methods include:
- Solvent/Detergent Treatment: This method disrupts the lipid envelopes of viruses, rendering them non-infectious.
- Heat Treatment: Pasteurization (heating at 60°C for 10 hours) or dry heat treatment can inactivate viruses.
- Nanofiltration: Filters with very small pore sizes (15-20 nanometers) can remove viruses based on size exclusion.
- Low pH Incubation: Some viruses are inactivated by incubating the product at low pH for extended periods.
- Formulation and Packaging: The purified proteins are formulated into stable preparations, often with stabilizers added to maintain protein activity during storage. The final products are packaged in sterile containers, labeled, and distributed for clinical use.
The fractionation process yields several valuable plasma-derived products, including albumin, immunoglobulins, clotting factors, and other therapeutic proteins. Each product undergoes rigorous quality control testing to ensure safety, purity, and potency before being released for clinical use.
Medical Uses of Plasma





