CRIF With PFN Surgery: A Comprehensive Guide
Introduction to CRIF With PFN Surgery
CRIF (Closed Reduction Internal Fixation) with PFN (Proximal Femoral Nail) is a sophisticated surgical procedure primarily used to treat fractures of the proximal femur, particularly intertrochanteric and subtrochanteric fractures. This minimally invasive technique has revolutionized the management of hip fractures, offering patients improved outcomes and faster recovery times compared to traditional surgical methods.
The proximal femur, which includes the femoral head, neck, and the region immediately below the trochanters, is a critical weight-bearing structure. Fractures in this area are common among the elderly population due to osteoporosis but can also occur in younger individuals following high-impact trauma. The PFN system represents a significant advancement in fracture fixation technology, providing stable internal support while allowing for early mobilization.
This comprehensive guide will delve into every aspect of CRIF with PFN surgery, from the anatomy of the femur to the surgical technique, recovery process, potential complications, and long-term outcomes. Whether you’re a patient preparing for this procedure, a medical student seeking to understand the technique, or a healthcare professional looking to expand your knowledge, this article will provide valuable insights into this important surgical intervention.
Anatomy of the Proximal Femur
Understanding the anatomy of the proximal femur is essential for comprehending the significance of CRIF with PFN surgery. The proximal femur consists of several key structures:
The femoral head is the rounded, ball-like structure that articulates with the acetabulum of the pelvis to form the hip joint. It is covered with articular cartilage, which allows for smooth movement within the joint. The femoral neck connects the head to the shaft of the femur at an angle of approximately 125 degrees, which is crucial for optimal biomechanical function.
The greater and lesser trochanters are bony prominences that serve as attachment sites for various muscles. The greater trochanter is located laterally and provides attachment for the gluteus medius, gluteus minimus, and piriformis muscles. The lesser trochanter is situated medially and serves as the insertion point for the iliopsoas muscle. The region between these trochanters is known as the intertrochanteric area, while the area just below the trochanters is called the subtrochanteric region.
Blood supply to the femoral head is primarily provided by the medial femoral circumflex artery, with additional contributions from the lateral femoral circumflex artery and the artery of the ligamentum teres. This vascular supply is particularly vulnerable in fractures of the femoral neck, which can lead to avascular necrosis if not properly addressed.
The biomechanics of the proximal femur are designed to withstand significant forces during weight-bearing activities. The trabecular bone within the femoral head and neck is organized along stress lines, providing maximum strength with minimal material. This delicate balance can be disrupted by fractures, leading to instability and loss of function.
Types of Proximal Femoral Fractures
Proximal femoral fractures can be classified into several categories based on their location and fracture pattern. Understanding these classifications is crucial for determining the appropriate treatment approach, including whether CRIF with PFN is the optimal choice.
Femoral neck fractures occur between the femoral head and the intertrochanteric line. These fractures are further classified using the Garden classification system:
- Type I: Incomplete or valgus-impacted fracture
- Type II: Complete fracture without displacement
- Type III: Complete fracture with partial displacement
- Type IV: Complete fracture with total displacement
Intertrochanteric fractures occur between the greater and lesser trochanters. The Evans-Jensen classification system is commonly used:
- Type I: Stable, two-part fracture
- Type II: Unstable, three-part fracture with posteromedial comminution
- Type III: Unstable, four-part fracture with posteromedial and posterolateral comminution
Subtrochanteric fractures occur in the region within 5 cm below the lesser trochanter. These fractures are often classified based on their location and pattern:
- Type I: Fractures at the level of the lesser trochanter
- Type II: Fractures extending from the lesser trochanter to the isthmus
- Type III: Fractures extending below the isthmus
Each type of fracture presents unique challenges in terms of reduction and fixation. The choice of surgical technique, including the decision to use CRIF with PFN, depends on various factors such as fracture stability, patient age, bone quality, and activity level.
Indications for CRIF With PFN Surgery
CRIF with PFN surgery is indicated for a variety of proximal femoral fractures, particularly those that are unstable or have specific characteristics that make this approach advantageous. The primary indications include:
Unstable intertrochanteric fractures (Evans-Jensen Type II and III) are well-suited for PFN fixation due to the nail’s ability to provide stability across the fracture site. The intramedullary location of the nail offers biomechanical advantages in these fracture patterns, reducing the risk of varus collapse and cut-out.
Subtrochanteric fractures are another strong indication for PFN fixation. These fractures are subject to high bending and torsional forces, which can be effectively neutralized by an intramedullary device. The PFN system provides excellent stability in this region, allowing for early weight-bearing in many cases.
Pathological fractures resulting from metastatic disease or other bone-weakening conditions can also be effectively treated with PFN. The nail provides immediate stability and pain relief, which is particularly important in patients with limited life expectancy.
Reverse obliquity fractures, which extend from the greater trochanter to the medial cortex below the lesser trochanter, are particularly well-suited for intramedullary fixation. These fractures are inherently unstable when treated with sliding hip screws due to the medialization of the femoral shaft, a problem effectively addressed by the PFN system.
In selected cases of femoral neck fractures, particularly in younger patients with vertical fracture patterns (Pauwels Type III), PFN may be considered as an alternative to cannulated screw fixation or hemiarthroplasty.
The decision to proceed with CRIF with PFN surgery takes into account various patient factors, including age, bone quality, activity level, comorbidities, and life expectancy. The goal is to provide stable fixation that allows for early mobilization while minimizing the risk of complications.
Contraindications for CRIF With PFN Surgery
While CRIF with PFN surgery is an excellent option for many proximal femoral fractures, certain conditions may contraindicate its use. Understanding these contraindications is essential for optimal patient selection and outcomes.
Absolute contraindications include active infection at the surgical site or systemic infection that could seed to the implant. In these cases, the surgery must be postponed until the infection is adequately treated. Another absolute contraindication is a pre-existing deformity of the femoral canal that prevents proper insertion of the nail.
Relative contrdications include severe osteoporosis with extremely poor bone quality, which may compromise the stability of the fixation. In such cases, alternative fixation methods or prosthetic replacement may be considered. Another relative contraindication is a very small femoral canal that cannot accommodate the smallest available nail size.
Patients with significant medical comorbidities that preclude surgery or anesthesia should be carefully evaluated. The risks of surgery must be weighed against the potential benefits, particularly in elderly patients with multiple health issues.
In cases of femoral neck fractures in elderly patients with pre-existing osteoarthritis or degenerative changes in the hip joint, arthroplasty may be a more appropriate option than internal fixation with PFN.
Certain fracture patterns may also be less suitable for PFN fixation. For example, very low subtrochanteric fractures extending into the femoral shaft may be better treated with a longer reconstruction nail or a different fixation method.
The presence of pre-existing hardware in the femur, such as a previous hip replacement or fracture fixation device, may complicate or preclude the use of PFN. In such cases, careful preoperative planning and consideration of alternative approaches are necessary.
Preoperative Evaluation and Planning
Thorough preoperative evaluation and planning are critical for the success of CRIF with PFN surgery. This comprehensive assessment ensures that the patient is medically optimized for the procedure and that the surgical team is prepared for any potential challenges.
The preoperative evaluation begins with a detailed medical history and physical examination. The history should include the mechanism of injury, pre-injury functional status, comorbidities, medications, allergies, and any previous surgeries. The physical examination should assess the neurovascular status of the affected limb, the degree of deformity, and the presence of any open wounds.
Laboratory tests typically include complete blood count, coagulation profile, basic metabolic panel, and possibly blood type and screen for potential transfusion. For elderly patients or those with significant comorbidities, additional tests such as electrocardiogram, chest X-ray, and arterial blood gas analysis may be necessary.
Imaging studies are crucial for preoperative planning. Standard radiographs should include anteroposterior (AP) view of the pelvis and affected hip, as well as lateral and cross-table lateral views of the proximal femur. These images help determine the fracture pattern, assess bone quality, and plan for appropriate implant sizing. In complex cases, computed tomography (CT) scans may provide additional detail about the fracture configuration and aid in surgical planning.
Preoperative templating involves using the radiographs to estimate the appropriate size and length of the PFN. This step is essential for ensuring that the correct implant is available during surgery and for anticipating any potential challenges that may arise during the procedure.
Medical optimization before surgery is particularly important in elderly patients with multiple comorbidities. This may involve consultation with various specialists, including cardiologists, pulmonologists, and anesthesiologists, to ensure that the patient is in the best possible condition for surgery.
Medication management is another critical aspect of preoperative planning. Anticoagulants and antiplatelet agents may need to be discontinued or managed in consultation with the prescribing physician. Patients with diabetes may require adjustments to their medication regimen to maintain optimal glucose control during the perioperative period.
Finally, patient education and informed consent are essential components of the preoperative process. The patient and their family should understand the nature of the procedure, expected outcomes, potential risks and complications, and the postoperative rehabilitation plan.
Surgical Technique: Step-by-Step Guide
The surgical technique for CRIF with PFN involves a systematic approach that requires precision and attention to detail. The following step-by-step guide outlines the key components of the procedure.
Patient Positioning and Preparation
The patient is typically positioned supine on a fracture table or a radiolucent table. A fracture table allows for traction and manipulation of the limb, facilitating closed reduction of the fracture. The affected limb is prepared and draped in the usual sterile fashion, with the entire leg exposed to allow for manipulation and imaging during the procedure.
Closed Reduction
The first step in CRIF with PFN is achieving a satisfactory closed reduction of the fracture. This is accomplished under fluoroscopic guidance using traction, internal rotation, and sometimes adduction or abduction of the limb. The goal is to restore the normal anatomical alignment of the femur, particularly the neck-shaft angle and length. The reduction is assessed in both AP and lateral views using image intensification.
Entry Point and Guide Wire Insertion
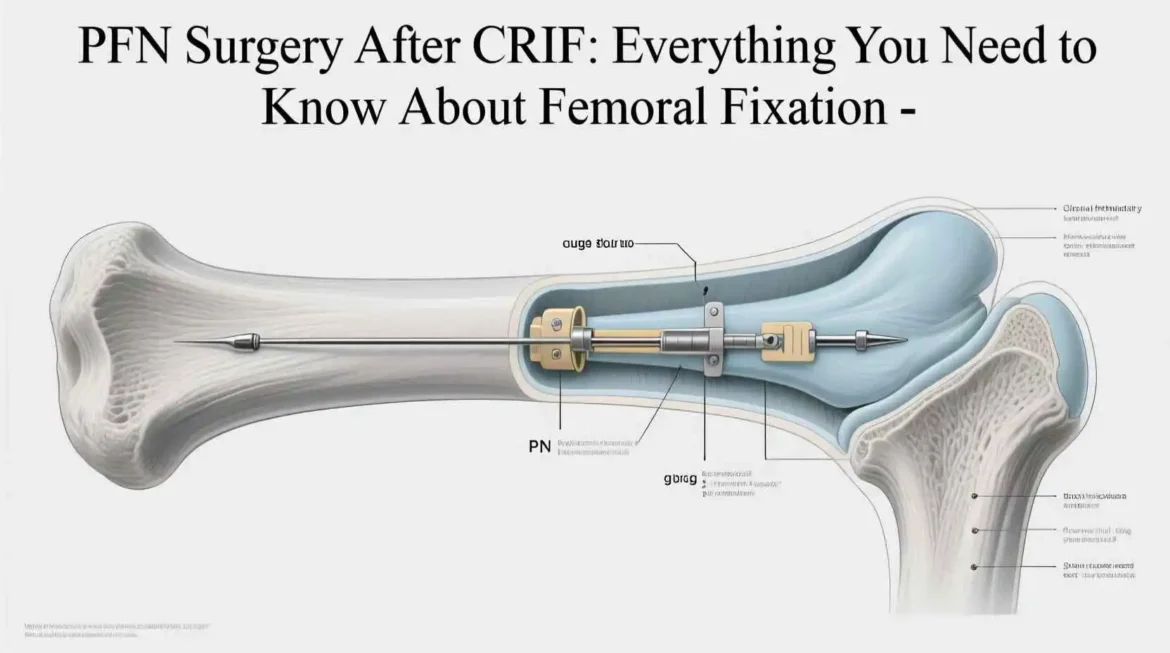
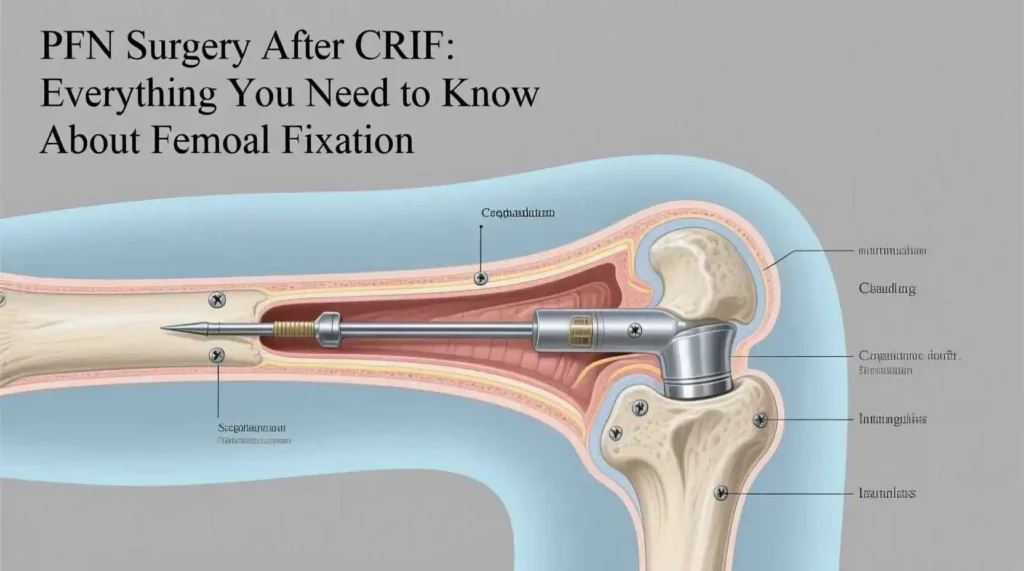
Once an acceptable reduction is achieved, an entry point is established for nail insertion. For most PFN systems, the entry point is located at the tip of the greater trochanter or slightly medial to it. A small incision is made over the entry point, and a guide wire is advanced into the femoral canal under fluoroscopic guidance. The position of the guide wire is confirmed in both AP and lateral views to ensure it is centered within the canal.
Reaming and Nail Insertion
The femoral canal is then prepared using reamers of increasing diameter. The degree of reaming depends on the patient’s bone quality and the size of the nail to be inserted. In osteoporotic bone, minimal reaming may be performed to preserve bone stock. Once the canal is adequately prepared, the appropriate length and diameter of the PFN is selected and inserted over the guide wire. The nail is advanced to the appropriate depth, typically with the proximal end of the nail slightly below the tip of the greater trochanter to avoid soft tissue irritation.
Locking Screw Insertion
After the nail is in position, the locking screws are inserted. Most PFN systems have two proximal screws: a larger lag screw that goes into the femoral neck and head, and a smaller anti-rotation screw that also engages the femoral neck. The lag screw provides compression across the fracture site, while the anti-rotation screw prevents rotation of the femoral head and neck fragment. The position of these screws is critical and must be confirmed in both AP and lateral views. Ideally, the lag screw should be placed in the center of the femoral head on both views, with its tip approximately 5-10 mm from the subchondral bone.
Distal Locking
Distal locking is performed to prevent rotation and shortening of the fracture. Most PFN systems allow for either static or dynamic locking. Static locking involves inserting screws through both holes in the distal part of the nail, completely immobilizing the construct. Dynamic locking uses only one screw, allowing controlled compression at the fracture site during weight-bearing. The choice between static and dynamic locking depends on the fracture pattern and stability.
Wound Closure
Once all implants are in position and their placement has been confirmed fluoroscopically, the wounds are closed in layers. The deep fascia is closed with absorbable sutures, followed by subcutaneous closure and skin closure with staples or sutures. Sterile dressings are applied, and the limb is typically placed in a foam boot or knee immobilizer for comfort and stability.
Intraoperative Imaging
Throughout the procedure, fluoroscopic imaging is used to confirm the reduction, guide wire position, nail placement, and screw positions. Final images should include AP and lateral views of the hip and femur to document the final construct and ensure proper implant positioning.
The entire procedure typically takes 60-90 minutes to perform, depending on the complexity of the fracture and the experience of the surgical team. Meticulous attention to detail during each step of the procedure is essential for achieving optimal outcomes and minimizing complications.
Types of PFN Systems