Several PFN systems are available on the market, each with unique design features intended to address specific challenges in proximal femoral fracture fixation. Understanding the differences between these systems is important for selecting the most appropriate implant for a given fracture pattern and patient.
Standard PFN
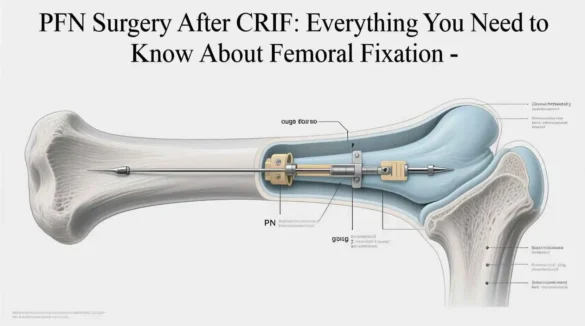
The standard PFN system consists of a main intramedullary nail with a proximal diameter of 15-17 mm and a distal diameter of 10-12 mm. The nail has a proximal angle of 6 degrees to match the anatomy of the proximal femur. The standard PFN uses two proximal screws: a large lag screw (typically 10-11 mm in diameter) for compression and a smaller anti-rotation screw (6.5 mm) to prevent rotation of the femoral head. The distal end of the nail has two options for locking: static or dynamic.
PFN-A (Antirotation)
The PFN-A system was designed to address some of the limitations of the standard PFN, particularly the risk of cut-out and the “Z-effect” phenomenon (where the anti-rotation screw migrates medially while the lag screw migrates laterally). The PFN-A uses a single helical blade instead of the two-screw configuration. The blade has a larger surface area for bone contact, which may provide better purchase in osteoporotic bone. The blade is also designed to compact bone during insertion, potentially increasing stability.
TFN (Trochanteric Fixation Nail)
The TFN system is similar to the PFN but has some design modifications. It uses a helical blade similar to the PFN-A but also offers the option of a two-screw configuration. The TFN has a more proximal starting point and a reduced proximal diameter (13-14 mm), which may reduce the risk of iatrogenic fracture during nail insertion. The TFN also offers a long nail option for fractures that extend into the femoral shaft.
Long PFN
Long PFN systems are designed for fractures that extend into the femoral shaft or for pathological fractures that require stabilization over a longer segment. These nails are available in lengths up to 48 cm and provide the option for multiple distal locking screws. Long PFNs are particularly useful for subtrochanteric fractures or for fractures in patients with osteoporosis or metastatic disease.
Cephalomedullary Nails
Cephalomedullary nails represent a broader category of implants that include PFN systems. These nails are designed to provide fixation in both the femoral head (cephalic) and the femoral shaft (medullary). Examples include the Gamma Nail, Intertan Nail, and various proprietary systems from different manufacturers. Each of these systems has unique design features that may make them more suitable for specific fracture patterns or patient populations.
Table: Comparison of Different PFN Systems
| Feature | Standard PFN | PFN-A | TFN | Long PFN |
| Proximal Fixation | Two screws (lag screw + anti-rotation screw) | Single helical blade | Helical blade or two screws | Two screws (lag screw + anti-rotation screw) |
| Proximal Diameter | 15-17 mm | 15-17 mm | 13-14 mm | 15-17 mm |
| Distal Diameter | 10-12 mm | 10-12 mm | 9-10 mm | 10-12 mm |
| Length Options | Up to 34 cm | Up to 34 cm | Up to 44 cm | Up to 48 cm |
| Distal Locking | Static or dynamic | Static or dynamic | Static or dynamic | Multiple options |
| Special Features | Standard design | Reduced cut-out risk | Reduced iatrogenic fracture risk | Extended stability for shaft fractures |
The choice of PFN system depends on various factors, including the fracture pattern, bone quality, patient anatomy, and surgeon preference. Each system has its advantages and limitations, and the selection should be based on a thorough understanding of these factors.
Postoperative Care and Rehabilitation
Postoperative care and rehabilitation are critical components of the treatment process for patients undergoing CRIF with PFN surgery. A well-structured rehabilitation program can significantly improve outcomes, reduce complications, and facilitate a faster return to functional independence.
Immediate Postoperative Period
In the immediate postoperative period, patients are typically monitored in the recovery room before being transferred to a regular ward or, in some cases, an intensive care unit for close observation. Pain management is a priority, with multimodal analgesia often employed to minimize opioid use and its associated side effects. This may include a combination of acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), regional nerve blocks, and limited opioids as needed.
Antibiotic prophylaxis is usually continued for 24 hours postoperatively to reduce the risk of surgical site infection. Thromboprophylaxis is also initiated, typically with low molecular weight heparin, direct oral anticoagulants, or mechanical prophylaxis such as intermittent pneumatic compression devices.
Wound care involves keeping the surgical incision clean and dry. Dressings are usually changed 24-48 hours after surgery, and staples or sutures are typically removed 10-14 days postoperatively, depending on wound healing.
Early Mobilization
Early mobilization is a cornerstone of postoperative care after CRIF with PFN surgery. Most patients are encouraged to get out of bed and begin weight-bearing as tolerated on the first postoperative day, with the assistance of physical therapists. The extent of weight-bearing depends on the fracture pattern, stability of fixation, and bone quality.
For stable fractures with good fixation, patients may be allowed to bear weight as tolerated immediately. For unstable fractures or those with poor bone quality, a period of protected weight-bearing (touch-down or toe-touch weight-bearing) may be recommended for 4-6 weeks to allow for initial healing.
Physical therapy focuses on exercises to maintain range of motion, strengthen the surrounding muscles, and improve gait mechanics. Occupational therapy may also be involved to help patients adapt their activities of daily living and ensure a safe home environment.
Intermediate Phase (2-6 Weeks)
During the intermediate phase of rehabilitation, the focus shifts to progressive weight-bearing and functional improvement. Patients typically advance from partial to full weight-bearing as tolerated, based on radiographic evidence of healing and clinical assessment.
Physical therapy exercises become more challenging, incorporating resistance training, balance exercises, and functional activities such as stair climbing. The goal is to restore normal gait pattern and improve lower extremity strength.
Follow-up appointments are usually scheduled at 2, 4, and 6 weeks postoperatively to assess clinical progress and obtain radiographs to evaluate fracture healing. Any concerns about pain, swelling, or mobility are addressed during these visits.
Late Phase (6-12 Weeks and Beyond)
In the late phase of rehabilitation, most patients have achieved fracture union and are working toward returning to their pre-injury level of function. Physical therapy focuses on advanced strengthening exercises, endurance training, and sport-specific or work-specific activities as appropriate.
For elderly patients, the emphasis may be on improving balance and preventing falls through targeted exercises and home modifications. For younger patients, the goal may be to return to sports or physically demanding occupations.
Long-term follow-up is typically scheduled at 3, 6, and 12 months postoperatively to assess final outcomes, including fracture union, implant position, and functional status. Some patients may require longer follow-up if there are concerns about implant-related complications or delayed healing.
Rehabilitation Considerations for Specific Populations
The rehabilitation protocol may need to be modified for specific patient populations:
Elderly patients with multiple comorbidities may progress more slowly and require additional support services such as home health nursing or outpatient rehabilitation. Cognitive impairment can also affect rehabilitation progress and may require adaptations to the standard protocol.
Patients with osteoporosis may require longer periods of protected weight-bearing and may benefit from medical management of their bone health, including calcium, vitamin D, and osteoporosis medications.
Younger patients with high-energy trauma may have associated injuries that affect their rehabilitation program. They may also require more intensive therapy to return to higher levels of function.
Table: Typical Rehabilitation Timeline After CRIF With PFN Surgery
| Time Period | Weight-Bearing Status | Physical Therapy Focus | Goals |
| Immediate (0-2 weeks) | Touch-down or partial weight-bearing as tolerated | Bed mobility, transfers, ambulation with assistive device, gentle range of motion exercises | Pain control, prevent complications, early mobilization |
| Early (2-6 weeks) | Progressively increase weight-bearing as tolerated | Progressive strengthening, gait training, balance exercises, activities of daily living | Restore normal gait pattern, improve strength and endurance |
| Intermediate (6-12 weeks) | Weight-bearing as tolerated, progressing to full weight-bearing | Advanced strengthening, proprioceptive training, functional activities | Achieve independent ambulation, return to basic activities |
| Late (12+ weeks) | Full weight-bearing | Sport-specific or work-specific training, high-level strengthening | Return to pre-injury activities, maximize function |
The rehabilitation process after CRIF with PFN surgery should be individualized based on the patient’s specific needs, goals, and rate of progress. A multidisciplinary approach involving orthopedic surgeons, physical therapists, occupational therapists, and primary care providers can optimize outcomes and facilitate a successful recovery.
Potential Complications and Their Management
While CRIF with PFN surgery is generally associated with good outcomes, like any surgical procedure, it carries the risk of potential complications. Understanding these complications and their management strategies is essential for optimizing patient care and outcomes.
Intraoperative Complications
Intraoperative complications during CRIF with PFN surgery can include:
Iatrogenic fracture during nail insertion is a potential complication, particularly in patients with osteoporotic bone or anatomic variations. This can occur at the proximal femur during reaming or nail insertion, or at the distal femur during locking screw placement. Management may involve modifying the surgical technique, using a different implant, or extending the fixation to address the new fracture.
Malpositioning of implants, particularly the lag screw or blade in the femoral head, can compromise fixation stability. If recognized intraoperatively, the implant should be repositioned to ensure optimal placement in the center of the femoral head on both AP and lateral views.
Difficulty with fracture reduction is another potential challenge, particularly in complex fracture patterns. In some cases, open reduction may be necessary if closed reduction cannot achieve an acceptable alignment.
Early Postoperative Complications
Early postoperative complications (within the first few weeks after surgery) can include:
Surgical site infection can occur in 1-5% of cases, depending on patient factors and surgical technique. Superficial infections may be managed with antibiotics and local wound care, while deep infections may require surgical debridement and possibly implant removal.
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are serious complications that can occur after hip fracture surgery. Thromboprophylaxis with anticoagulants and mechanical devices is standard practice to reduce this risk. If DVT or PE is suspected, appropriate diagnostic imaging should be obtained, and treatment with therapeutic anticoagulation should be initiated.
Hematoma formation at the surgical site can cause pain and swelling and may increase the risk of infection. Small hematomas may resolve spontaneously, while larger ones may require drainage.
Late Complications
Late complications (occurring weeks to months after surgery) can include:
Cut-out of the lag screw or blade from the femoral head is one of the most common mechanical complications, occurring in 3-10% of cases. This is more common in elderly patients with osteoporotic bone and in cases where the implant is not optimally positioned. Management may involve revision surgery with a different fixation method or conversion to arthroplasty.
Nonunion or delayed union of the fracture can occur, particularly in unstable fracture patterns or in patients with poor bone quality or comorbidities that impair healing. Treatment may involve bone grafting, exchange nailing, or electrical stimulation to promote healing.
Malunion with varus deformity can occur if the fracture collapses before healing. This can lead to limb shortening, altered gait mechanics, and increased stress on the implant. Significant malunion may require corrective osteotomy.
Implant failure, including breakage of the nail or screws, can occur in cases of nonunion or with excessive weight-bearing before fracture healing. Management typically involves revision surgery with a different fixation method.
Avascular necrosis of the femoral head is a rare but serious complication that can occur if the blood supply to the femoral head is disrupted during the injury or surgery. This may require treatment with core decompression, bone grafting, or conversion to arthroplasty.
Heterotopic ossification, or abnormal bone formation in the soft tissues around the hip, can cause pain and limited range of motion. In severe cases, surgical excision may be necessary.
Table: Potential Complications of CRIF With PFN Surgery and Their Management
| Complication | Incidence | Risk Factors | Management Strategies |
| Surgical site infection | 1-5% | Diabetes, obesity, immunosuppression, prolonged surgery | Antibiotics, wound care, surgical debridement for deep infections |
| Deep vein thrombosis | 2-10% | Advanced age, obesity, immobility, history of DVT | Anticoagulation, inferior vena cava filter for contraindications to anticoagulation |
| Lag screw cut-out | 3-10% | Osteoporosis, poor implant positioning, unstable fracture | Revision fixation or conversion to arthroplasty |
| Nonunion | 2-5% | Comminuted fractures, poor bone quality, smoking, diabetes | Bone grafting, exchange nailing, electrical stimulation |
| Malunion | 2-8% | Unstable fracture, inadequate fixation, early weight-bearing | Observation for mild cases, corrective osteotomy for significant deformity |
| Implant failure | 1-3% | Nonunion, excessive weight-bearing, poor bone quality | Revision surgery with different fixation method |
| Avascular necrosis | 1-2% | Femoral neck fractures, disruption of blood supply | Core decompression, bone grafting, arthroplasty |
Prevention of Complications
Preventing complications is a key aspect of managing patients undergoing CRIF with PFN surgery. Several strategies can help reduce the risk of complications:
Careful patient selection and preoperative optimization can minimize the risk of medical complications. This includes managing comorbidities, optimizing nutrition, and addressing any modifiable risk factors.
Meticulous surgical technique is essential for reducing the risk of mechanical complications. This includes achieving and maintaining anatomic reduction, proper implant positioning, and appropriate selection of implant size and configuration.
Appropriate postoperative management, including thromboprophylaxis, infection prevention, and guided rehabilitation, can help prevent many common complications.
Regular follow-up with clinical assessment and radiographic evaluation allows for early detection and management of complications before they become more serious.
By understanding the potential complications associated with CRIF with PFN surgery and implementing appropriate prevention and management strategies, healthcare providers can optimize outcomes for patients undergoing this procedure.
Outcomes and Prognosis
The outcomes and prognosis following CRIF with PFN surgery are generally favorable, with most patients achieving fracture union and returning to their pre-injury level of function. However, outcomes can vary based on numerous factors, including patient characteristics, fracture pattern, and surgical technique.
Fracture Union Rates
Fracture union rates after CRIF with PFN surgery typically range from 90% to 98%, depending on the fracture pattern and patient population. Stable intertrochanteric fractures generally have higher union rates compared to unstable or subtrochanteric fractures. Factors that can negatively impact union rates include:
- Advanced age
- Osteoporosis
- Comminuted fractures
- Poor fracture reduction
- Inadequate fixation
- Comorbidities such as diabetes
- Smoking
Most fractures heal within 12-16 weeks after surgery, although complete remodeling may take up to a year or more.
Functional Outcomes
Functional outcomes after CRIF with PFN surgery are generally good, with most patients returning to independent ambulation and activities of daily living. However, outcomes can vary significantly based on pre-injury functional status, age, and comorbidities.
In elderly patients, the primary goal is often to return to pre-fracture level of function. Studies have shown that approximately 60-80% of elderly patients regain their pre-fracture mobility status after PFN fixation. However, some patients may require assistive devices such as canes or walkers for ambulation.
In younger patients with high-energy trauma, outcomes are generally excellent, with most patients returning to their previous level of activity, including sports and physically demanding occupations. However, recovery may take 6-12 months or longer, and some patients may have permanent limitations.
Mortality Rates
Mortality after hip fracture surgery is a significant concern, particularly in elderly patients. The 1-year mortality rate after hip fracture ranges from 14% to 36%, with most deaths occurring in the first 3-6 months after surgery. Factors associated with higher mortality include:
- Advanced age
- Male gender
- Multiple comorbidities
- Pre-fracture institutionalization
- Delay to surgery (>48 hours)
- Postoperative complications
It’s important to note that most of these deaths are not directly related to the surgery or fracture but rather to underlying medical conditions and the physiological stress of the injury and surgery.
Quality of Life
Quality of life after CRIF with PFN surgery can be significantly impacted by the fracture and subsequent recovery. Many patients experience temporary reductions in quality of life during the recovery period, with gradual improvement over time.
Studies have shown that most patients return to their pre-fracture quality of life within 6-12 months after surgery, although some may have permanent limitations. Factors associated with poorer quality of life outcomes include:
- Advanced age
- Pre-fracture functional limitations
- Postoperative complications
- Persistent pain
- Loss of independence
Comparison With Other Treatment Modalities
When compared to other treatment modalities for proximal femoral fractures, CRIF with PFN surgery has several advantages:
Compared to sliding hip screw (SHS) fixation, PFN has been shown to have lower rates of reoperation and implant failure, particularly in unstable fracture patterns. However, SHS may be associated with shorter operative times and less blood loss in stable fractures.
Compared to hemiarthroplasty or total hip arthroplasty, PFN preserves the patient’s native hip joint, which may be advantageous in younger patients. However, arthroplasty may be associated with lower reoperation rates in elderly patients with displaced femoral neck fractures.
Compared to non-operative treatment, CRIF with PFN surgery allows for earlier mobilization, reduced pain, and lower rates of complications such as pressure ulcers and pneumonia. Non-operative treatment is generally reserved for non-ambulatory patients or those with prohibitive surgical risks.
Table: Outcomes After CRIF With PFN Surgery by Fracture Type
| Outcome Measure | Stable Intertrochanteric Fractures | Unstable Intertrochanteric Fractures | Subtrochanteric Fractures |
| Union Rate | 95-98% | 90-95% | 85-90% |
| Time to Union | 8-12 weeks | 12-16 weeks | 16-20 weeks |
| Reoperation Rate | 2-5% | 5-10% | 10-15% |
| Return to Pre-fracture Function | 70-80% | 60-70% | 50-60% |
| 1-year Mortality | 14-20% | 20-25% | 15-20% |
Long-term Outcomes
Long-term outcomes after CRIF with PFN surgery are generally favorable, with most patients maintaining good function for many years after surgery. However, some patients may experience late complications or functional decline over time.
Implant-related complications can occur years after surgery, particularly in younger, more active patients. These may include implant failure, stress shielding, or periprosthetic fractures. In some cases, removal of the implant may be necessary if it causes persistent pain or other symptoms.
Osteoarthritis of the hip joint can develop years after surgery, particularly in patients with intra-articular fracture extension or pre-existing degenerative changes. This may require treatment with anti-inflammatory medications, physical therapy, or eventually, conversion to arthroplasty.
Functional decline can occur over time, particularly in elderly patients due to age-related changes, comorbidities, or loss of muscle strength. Ongoing rehabilitation and maintenance exercises can help preserve function and independence.
Overall, CRIF with PFN surgery is associated with good to excellent outcomes for most patients with proximal femoral fractures. Careful patient selection, meticulous surgical technique, and appropriate postoperative management are key factors in optimizing outcomes and prognosis.
Advancements and Future Directions
The field of proximal femoral fracture fixation continues to evolve, with ongoing advancements in implant design, surgical techniques, and postoperative management. These innovations aim to improve outcomes, reduce complications, and enhance the quality of life for patients undergoing CRIF with PFN surgery.
Implant Design Innovations
Recent advancements in PFN design have focused on addressing the limitations of earlier systems and improving outcomes in challenging fracture patterns:
Newer generation PFN systems feature optimized geometries that better match the anatomy of the proximal femur, reducing the risk of iatrogenic fracture during insertion. These nails often have a more proximal starting point and a reduced proximal diameter, which may be particularly beneficial in patients with narrow femoral canals or osteoporotic bone.
Enhanced locking mechanisms have been developed to improve stability and reduce the risk of implant failure. Some systems now offer angular stable locking options, which provide fixed-angle fixation at the proximal and distal ends of the nail, potentially reducing the risk of cut-out and varus collapse.
Biomechanical improvements in PFN design have focused on optimizing load transfer and reducing stress concentrations that can lead to implant failure. Some newer nails feature more flexible distal sections that reduce stress risers and lower the risk of periprosthetic fractures.
Biomaterials and Surface Technologies
Advancements in biomaterials and surface technologies are enhancing the performance of PFN systems:
Newer titanium alloys with improved strength-to-weight ratios are being used in some PFN systems, potentially reducing the risk of implant failure while minimizing stress shielding effects. These alloys also have improved biocompatibility, which may reduce the risk of adverse tissue reactions.
Surface modifications, including porous coatings and hydroxyapatite coatings, are being explored to enhance osseointegration and improve fixation in osteoporotic bone. These coatings may allow for better bone ingrowth and long-term stability, particularly in challenging cases.
Biodegradable materials are being investigated for use in certain components of PFN systems, potentially reducing the need for implant removal surgery and minimizing long-term complications associated with permanent implants.
Surgical Technique Innovations
Innovations in surgical technique are improving the precision and efficiency of CRIF with PFN surgery:
Computer-assisted navigation systems are increasingly being used to guide implant placement, potentially improving the accuracy of lag screw or blade positioning in the femoral head. These systems use intraoperative imaging and real-time tracking to provide the surgeon with detailed guidance during the procedure.
Robotic-assisted surgery is emerging as a potential tool for proximal femoral fracture fixation, offering enhanced precision and potentially reducing the risk of human error. While still in the early stages of adoption, robotic systems may become more commonplace in the future.
Minimally invasive surgical techniques continue to evolve, with smaller incisions, less soft tissue dissection, and reduced blood loss. These approaches may lead to faster recovery times and lower complication rates.
Postoperative Management Advances
Innovations in postoperative management are enhancing recovery and outcomes after CRIF with PFN surgery:
Enhanced recovery after surgery (ERAS) protocols are being implemented for hip fracture patients, standardizing perioperative care and optimizing outcomes. These protocols typically include multimodal pain management, early mobilization, standardized nutritional support, and structured rehabilitation programs.
Remote monitoring technologies, including wearable sensors and mobile applications, are being used to track patient progress during rehabilitation and provide real-time feedback to healthcare providers. These technologies may allow for earlier detection of complications and more personalized rehabilitation programs.
Regenerative medicine approaches, including the use of stem cells, growth factors, and bone graft substitutes, are being investigated to enhance fracture healing, particularly in patients with risk factors for delayed union or nonunion. While still largely experimental, these approaches may become more commonplace in the future.
Future Directions
The future of CRIF with PFN surgery is likely to be shaped by several key trends:
Personalized medicine approaches, including patient-specific implant design and customized rehabilitation protocols, may become more prevalent as our understanding of individual factors affecting outcomes improves. Advanced imaging and 3D printing technologies may enable the creation of implants tailored to individual patient anatomy.
Artificial intelligence and machine learning algorithms may be used to predict outcomes, optimize surgical planning, and guide postoperative management. These tools could help identify patients at risk for complications and suggest personalized treatment strategies.
Preventive strategies, including fall prevention programs, osteoporosis management, and fracture liaison services, are likely to play an increasingly important role in reducing the incidence of proximal femoral fractures and improving outcomes for at-risk patients.
As the population continues to age and the incidence of proximal femoral fractures increases, the importance of advancing the field of CRIF with PFN surgery cannot be overstated. Ongoing research and innovation will be critical to meeting the growing demand for effective fracture fixation and improving outcomes for patients worldwide.
Frequently Asked Questions (FAQs)
1. What is CRIF with PFN surgery?
CRIF with PFN surgery is a minimally invasive surgical procedure used to treat fractures of the proximal femur, particularly intertrochanteric and subtrochanteric fractures. CRIF stands for Closed Reduction Internal Fixation, which means the fracture is aligned without making a large incision, and internal fixation devices are used to hold the bone in place. PFN refers to the Proximal Femoral Nail, which is a metal rod inserted into the femur to stabilize the fracture. This technique allows for early mobilization and has been associated with good outcomes in appropriately selected patients.
2. Who is a candidate for CRIF with PFN surgery?
Candidates for CRIF with PFN surgery include patients with intertrochanteric fractures, subtrochanteric fractures, and certain types of femoral neck fractures. The procedure is particularly suitable for unstable fracture patterns, fractures in patients with osteoporosis, and pathological fractures resulting from metastatic disease. The decision to proceed with CRIF with PFN surgery takes into account various factors, including the patient’s age, bone quality, activity level, comorbidities, and life expectancy. A thorough evaluation by an orthopedic surgeon is necessary to determine if this procedure is appropriate for a specific patient.
3. How long does the CRIF with PFN surgery take?
The duration of CRIF with PFN surgery typically ranges from 60 to 90 minutes, depending on the complexity of the fracture and the experience of the surgical team. Simple fractures with good bone quality may be completed more quickly, while complex fractures with comminution or poor bone quality may require more time. The procedure involves several steps, including patient positioning, closed reduction of the fracture, preparation of the femoral canal, insertion of the nail, and placement of locking screws. Each step must be performed carefully to ensure optimal outcomes, which contributes to the overall duration of the surgery.
4. What type of anesthesia is used for CRIF with PFN surgery?
CRIF with PFN surgery can be performed under general anesthesia, regional anesthesia (spinal or epidural), or a combination of both. The choice of anesthesia depends on various factors, including the patient’s medical condition, preferences, and the anesthesiologist’s recommendation. Regional anesthesia is often preferred in elderly patients as it may be associated with fewer complications such as postoperative cognitive dysfunction. However, general anesthesia may be necessary for patients with contraindications to regional anesthesia or those who prefer to be unconscious during the procedure. The anesthesiologist will discuss the options with the patient prior to surgery.
5. How long is the hospital stay after CRIF with PFN surgery?
The length of hospital stay after CRIF with PFN surgery varies depending on the patient’s age, overall health, functional status, and support system at home. In general, most patients stay in the hospital for 3 to 7 days after surgery. During this time, pain is managed, wound care is provided, and physical therapy is initiated to help the patient regain mobility. Patients who are medically stable, have adequate pain control, and demonstrate the ability to perform basic transfers and ambulate with assistive devices may be discharged earlier. Some patients may require additional time in the hospital or transfer to a rehabilitation facility for more intensive therapy before returning home.
6. What is the recovery time after CRIF with PFN surgery?
The recovery time after CRIF with PFN surgery varies depending on the patient’s age, overall health, fracture pattern, and adherence to rehabilitation protocols. In general, most patients can expect to return to basic activities of daily living within 4 to 6 weeks after surgery. Fracture healing typically occurs within 12 to 16 weeks, although complete remodeling may take up to a year or longer. Younger patients with simpler fractures may recover more quickly, while elderly patients with complex fractures and multiple comorbidities may have a longer recovery period. Full recovery, including return to sports or physically demanding activities, may take 6 to 12 months or longer.
7. How much weight can I bear on my leg after CRIF with PFN surgery?
The weight-bearing status after CRIF with PFN surgery depends on the fracture pattern, stability of fixation, bone quality, and surgeon’s preference. For stable fractures with good fixation, patients may be allowed to bear weight as tolerated immediately after surgery. For unstable fractures or those with poor bone quality, a period of protected weight-bearing (touch-down or toe-touch weight-bearing) may be recommended for 4 to 6 weeks to allow for initial healing. The surgeon will provide specific weight-bearing instructions based on the individual patient’s situation, and these instructions should be followed carefully to optimize healing and reduce the risk of complications.
8. What are the potential risks and complications of CRIF with PFN surgery?
Like any surgical procedure, CRIF with PFN surgery carries potential risks and complications. These can include infection (1-5%), deep vein thrombosis (2-10%), pulmonary embolism, lag screw cut-out (3-10%), nonunion or delayed union (2-5%), malunion (2-8%), implant failure (1-3%), avascular necrosis of the femoral head (1-2%), and heterotopic ossification. Other risks include those associated with anesthesia, such as adverse reactions to medications, respiratory complications, and cardiovascular events. The surgeon will discuss these risks with the patient prior to surgery and take appropriate measures to minimize them.
9. How successful is CRIF with PFN surgery?
CRIF with PFN surgery is generally associated with good outcomes, with success rates ranging from 90% to 98% in terms of fracture union. Functional outcomes are also generally favorable, with most patients returning to their pre-injury level of function or a level close to it. The success of the procedure depends on various factors, including patient selection, fracture pattern, surgical technique, and adherence to postoperative rehabilitation protocols. Complications can occur, but with careful patient selection, meticulous surgical technique, and appropriate postoperative management, the risk of complications can be minimized, and the likelihood of a successful outcome can be maximized.
10. Will I need physical therapy after CRIF with PFN surgery?
Yes, physical therapy is an essential component of the recovery process after CRIF with PFN surgery. Physical therapy typically begins in the hospital within the first day or two after surgery and continues after discharge, either in an outpatient setting, at home, or in a rehabilitation facility. The goals of physical therapy include improving range of motion, strengthening the muscles around the hip and leg, improving balance and coordination, and gradually increasing weight-bearing and functional activities. The physical therapist will work with the patient to develop an individualized rehabilitation program based on their specific needs and goals.
11. How long will I need to use a walker or crutches after CRIF with PFN surgery?
The duration of walker or crutch use after CRIF with PFN surgery varies depending on the patient’s age, overall health, fracture pattern, weight-bearing status, and progress in rehabilitation. In general, most patients use a walker for the first 2 to 4 weeks after surgery, then transition to crutches or a cane for another 2 to 4 weeks. Some patients, particularly elderly individuals or those with balance issues, may need to use an assistive device for a longer period. The physical therapist and surgeon will provide guidance on when it is appropriate to progress from one assistive device to another based on the patient’s strength, balance, and weight-bearing status.
12. When can I drive after CRIF with PFN surgery?
The timing for returning to driving after CRIF with PFN surgery depends on several factors, including which leg was operated on, the patient’s overall recovery, weight-bearing status, and local driving regulations. For patients who had surgery on their right leg (the accelerator leg), driving is typically not recommended until they can bear full weight without pain and have sufficient strength and control to operate the pedals safely. This usually takes at least 6 to 8 weeks after surgery. For patients who had surgery on their left leg (in countries where the driver sits on the left side of the car), driving may be possible sooner, typically 4 to 6 weeks after surgery, once they can comfortably operate the clutch pedal. The patient should consult with their surgeon before resuming driving.
13. Will the implant need to be removed after the fracture heals?
In most cases, the PFN implant does not need to be removed after the fracture heals. The implant is designed to remain in place permanently, and removal surgery carries its own risks and potential complications. However, there are certain situations where implant removal may be considered, including persistent pain or irritation caused by the implant, infection, implant failure, or in young patients who are concerned about the long-term presence of the implant. The decision to remove the implant should be made in consultation with the surgeon, weighing the potential benefits against the risks of additional surgery.
14. Can I develop arthritis in my hip after CRIF with PFN surgery?
While CRIF with PFN surgery is designed to stabilize the fracture and preserve the hip joint, there is a possibility of developing arthritis in the hip after the procedure. This can occur due to several reasons, including damage to the articular cartilage during the initial injury, altered biomechanics of the hip joint after fracture healing, or the natural progression of pre-existing arthritis. The risk of developing arthritis varies depending on the fracture pattern, the accuracy of reduction, and individual patient factors. If arthritis does develop, treatment options include medications, physical therapy, activity modification, and in some cases, conversion to hip replacement surgery.
15. How soon can I return to work after CRIF with PFN surgery?
The timing for returning to work after CRIF with PFN surgery depends on the nature of the patient’s job, the severity of the fracture, the patient’s overall recovery, and the surgeon’s recommendation. For sedentary jobs that involve mostly sitting and minimal walking, patients may be able to return to work within 4 to 6 weeks after surgery, once they can sit comfortably and have adequate pain control. For jobs that require standing, walking, or light physical activity, return to work may take 8 to 12 weeks. For physically demanding jobs that involve heavy lifting, climbing, or strenuous activity, return to work may take 3 to 6 months or longer. The patient should discuss their specific job requirements with their surgeon to determine a safe timeline for returning to work.
16. What are the signs of infection after CRIF with PFN surgery?
Signs of infection after CRIF with PFN surgery can include increased pain at the surgical site, redness, warmth, swelling, pus or drainage from the incision, fever, chills, and generally feeling unwell. In some cases, the infection may be deep and not immediately apparent at the incision site, presenting as persistent pain without obvious signs of superficial infection. If any of these signs or symptoms develop, the patient should contact their surgeon promptly for evaluation. Early diagnosis and treatment of infection are crucial to prevent more serious complications.
17. How can I prevent blood clots after CRIF with PFN surgery?
Preventing blood clots (deep vein thrombosis and pulmonary embolism) after CRIF with PFN surgery is an important aspect of postoperative care. Several strategies can help reduce the risk of blood clots, including:
- Early mobilization and walking as soon as possible after surgery
- Use of compression stockings or intermittent pneumatic compression devices
- Anticoagulant medications as prescribed by the surgeon
- Staying well-hydrated
- Avoiding prolonged periods of immobility
- Performing ankle pumps and other leg exercises as recommended by the physical therapist
The surgeon will typically prescribe a specific thromboprophylaxis regimen based on the patient’s individual risk factors, and it is important to follow these recommendations carefully.
18. What should I do if I experience severe pain after CRIF with PFN surgery?
While some pain is expected after CRIF with PFN surgery, severe or worsening pain should be evaluated promptly. If the pain is sudden, severe, or associated with other symptoms such as fever, chills, redness, swelling, or inability to bear weight, the patient should contact their surgeon or seek immediate medical attention. These could be signs of complications such as infection, implant failure, or fracture displacement. For expected postoperative pain, the surgeon will typically prescribe pain medications, and the patient should take them as directed. It is important to follow the prescribed medication regimen and not exceed the recommended dosage.
19. Can I shower after CRIF with PFN surgery?
Showering after CRIF with PFN surgery depends on the surgeon’s recommendations and the status of the incision. In general, patients should keep the incision dry until it has fully healed, which typically takes 7 to 14 days after surgery. During this time, sponge baths are usually recommended, avoiding getting the incision wet. Once the incision has healed and any staples or sutures have been removed, the patient can typically shower, but should avoid soaking the incision in a bath, hot tub, or swimming pool until the surgeon gives clearance, which is usually 4 to 6 weeks after surgery. The surgeon will provide specific instructions regarding wound care and showering based on the individual patient’s situation.
20. How long will the pain last after CRIF with PFN surgery?
The duration of pain after CRIF with PFN surgery varies depending on the patient’s pain tolerance, the severity of the fracture, the surgical technique, and the effectiveness of pain management strategies. In general, most patients experience significant pain relief within the first week after surgery as the initial surgical pain subsides. However, some degree of pain or discomfort may persist for several weeks or months as the fracture heals and the patient rehabilitates. By 3 to 6 months after surgery, most patients report minimal to no pain during normal activities. Some patients may experience occasional aching or discomfort, particularly with changes in weather or increased activity, which is normal and usually improves with time.
21. What activities should I avoid after CRIF with PFN surgery?
After CRIF with PFN surgery, there are certain activities that should be avoided or modified to protect the healing fracture and prevent complications. These typically include:
- High-impact activities such as running, jumping, or contact sports
- Twisting or pivoting motions at the hip
- Crossing the legs or ankles
- Sitting on low chairs or toilets that cause excessive hip flexion
- Bending forward at the waist beyond 90 degrees
- Heavy lifting (typically defined as anything heavier than 10-15 pounds)
The surgeon and physical therapist will provide specific activity restrictions based on the patient’s individual situation, and these restrictions are typically gradually lifted as the fracture heals and strength improves.
22. Can I fly after CRIF with PFN surgery?
Flying after CRIF with PFN surgery is generally possible once the patient is medically stable and can tolerate the journey. For short flights (less than 2 hours), patients may be able to fly within 2 to 3 weeks after surgery, once they are comfortable sitting for extended periods and have adequate pain control. For longer flights, it is generally recommended to wait at least 4 to 6 weeks after surgery to reduce the risk of blood clots. During the flight, patients should take precautions to reduce the risk of deep vein thrombosis, such as staying well-hydrated, wearing compression stockings, performing ankle pumps and leg exercises, and walking around the cabin periodically when safe to do so. The patient should consult with their surgeon before planning air travel after surgery.
23. How will I know if my fracture is healing properly?
There are several signs that indicate a fracture is healing properly after CRIF with PFN surgery:
- Gradual decrease in pain at the fracture site
- Increasing ability to bear weight on the affected leg
- Improvement in strength and range of motion
- X-rays showing callus formation and bridging bone across the fracture site
The surgeon will monitor the healing process through regular follow-up appointments and periodic X-rays. At these appointments, the surgeon will assess the patient’s clinical progress and review the X-rays to ensure the fracture is healing as expected. If there are concerns about delayed healing or nonunion, the surgeon may order additional tests or recommend interventions to promote healing.
24. What should I do if I think my implant is failing?
If a patient suspects their implant is failing after CRIF with PFN surgery, they should contact their surgeon promptly for evaluation. Signs of potential implant failure can include:
- Sudden increase in pain at the fracture site
- New or worsening deformity of the leg
- Inability to bear weight on the affected leg
- Audible or palpable clicking or grinding at the implant site
- Visible loosening or breakage of the implant on X-ray
The surgeon will typically order X-rays or other imaging studies to assess the position and integrity of the implant and the status of fracture healing. If implant failure is confirmed, additional surgery may be necessary to revise the fixation or address any complications.
25. Can I develop osteoporosis after CRIF with PFN surgery?
CRIF with PFN surgery itself does not cause osteoporosis, but the underlying factors that led to the fracture may be associated with osteoporosis, particularly in elderly patients. In fact, many proximal femoral fractures occur in patients with pre-existing osteoporosis. After surgery, it is important to address any underlying bone health issues to reduce the risk of future fractures. This may include:
- Bone density testing to assess for osteoporosis
- Calcium and vitamin D supplementation
- Prescription medications to treat osteoporosis, such as bisphosphonates
- Weight-bearing exercise to maintain bone density
- Fall prevention strategies
The surgeon may refer the patient to a bone health specialist or endocrinologist for further evaluation and management of osteoporosis.
26. How does CRIF with PFN surgery compare to hip replacement?
CRIF with PFN surgery and hip replacement are different procedures with different indications and outcomes. CRIF with PFN surgery is an internal fixation procedure that stabilizes the fracture while preserving the patient’s native hip joint. It is typically used for fractures where the blood supply to the femoral head is intact and the joint surface is not significantly damaged. Hip replacement, on the other hand, involves replacing the damaged joint with an artificial implant and is typically used for fractures where the blood supply to the femoral head is compromised (such as displaced femoral neck fractures) or in patients with pre-existing arthritis.
Compared to hip replacement, CRIF with PFN surgery is generally associated with less blood loss, shorter operative time, and lower risk of dislocation. However, hip replacement may be associated with lower reoperation rates in certain patient populations, particularly elderly patients with displaced femoral neck fractures. The choice between these procedures depends on various factors, including the fracture pattern, patient age, activity level, and pre-existing joint disease.
27. What is the cost of CRIF with PFN surgery?
The cost of CRIF with PFN surgery varies widely depending on factors such as geographic location, hospital setting, insurance coverage, and the specific implant used. In the United States, the total cost of the procedure, including surgeon fees, hospital fees, anesthesia, and implant costs, can range from $15,000 to $50,000 or more. Patients with health insurance may be responsible for a portion of these costs, depending on their specific plan. It is important for patients to check with their insurance provider to understand their coverage and out-of-pocket costs. For uninsured patients, many hospitals offer financial assistance programs or payment plans to help manage the cost of care.
28. How soon can I resume sexual activity after CRIF with PFN surgery?
Resuming sexual activity after CRIF with PFN surgery depends on the patient’s comfort level, pain control, and the surgeon’s recommendations. In general, patients can resume sexual activity once they can comfortably move their hip without significant pain and have adequate strength and stability, which is typically 4 to 6 weeks after surgery. However, it is important to avoid positions that cause excessive stress on the healing fracture or the implant. The patient should discuss any concerns about sexual activity with their surgeon, who can provide specific guidance based on the individual’s recovery progress.
29. Can I play sports after CRIF with PFN surgery?
Returning to sports after CRIF with PFN surgery depends on the type of sport, the patient’s recovery progress, and the surgeon’s recommendation. In general, low-impact sports such as swimming, golf, and doubles tennis can typically be resumed 3 to 6 months after surgery, once the fracture has fully healed and strength has been restored. High-impact sports such as running, basketball, soccer, and singles tennis may require 6 to 12 months or longer of recovery, and in some cases, may not be recommended, particularly for patients with osteoporosis or other risk factors for re-injury. The patient should discuss their desire to return to sports with their surgeon, who can provide specific guidance based on the individual’s situation.
30. What is the long-term outlook after CRIF with PFN surgery?
The long-term outlook after CRIF with PFN surgery is generally favorable for most patients. Studies have shown that the majority of patients achieve fracture union and return to their pre-injury level of function or a level close to it. The implant is designed to remain in place permanently, and most patients do not require additional surgery related to the fracture or implant. However, the long-term outlook can be influenced by various factors, including the patient’s age, overall health, bone quality, and adherence to rehabilitation protocols. Some patients may experience persistent pain, limited mobility, or other long-term issues, but these are relatively uncommon. Regular follow-up with the surgeon and ongoing attention to bone health and fall prevention can help optimize the long-term outcomes after CRIF with PFN surgery
Medical Disclaimer:
The information provided on this website is for general educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.