Phaco Surgery Explained: The Gold Standard in Cataract Treatment
Vision is arguably our most precious sense, allowing us to navigate the world, connect with loved ones, and pursue our passions. However, as we age, many of us will experience a common condition that can gradually diminish this vital sense: cataracts. For decades, cataract removal has been a cornerstone of ophthalmic surgery, and today, the gold standard procedure is Phacoemulsification, commonly known as Phaco surgery. In this comprehensive article, we will delve into what Phaco surgery entails, explore its remarkable features, and understand why it has revolutionized the treatment of cataracts, restoring clear vision for millions worldwide.
Understanding Cataracts: A Precursor to Phaco Surgery
Before we delve into the sophisticated mechanics of Phaco surgery, it’s crucial to first grasp the fundamental nature of the condition it aims to correct. A cataract is not a growth on the eye, but rather a progressive clouding of the eye’s natural lens. This lens, typically clear and flexible, functions much like a camera lens, focusing light onto the retina at the back of the eye, allowing us to see sharp, clear images.
When a cataract develops, the proteins within this once-transparent lens begin to clump together, turning it opaque and hindering the passage of light. Imagine looking through a frosted window or a smudged camera lens – that’s akin to how a cataract affects vision. This clouding causes light to scatter rather than focus cleanly, leading to a range of visual disturbances. Common symptoms include:
- Blurry or Cloudy Vision: The world may appear hazy, foggy, or as if you’re looking through a dirty pane of glass. This is often the most noticeable symptom.
- Glare Sensitivity: Bright lights, particularly headlights at night or sunlight during the day, can cause significant discomfort, halos, or starbursts, making activities like driving hazardous.
- Dulled or Faded Colors: Colors may seem less vibrant, losing their intensity and richness. Blues and purples are often among the first to be affected.
- Difficulty Seeing at Night: Reduced contrast sensitivity and increased glare make night driving especially challenging and often dangerous.
- Frequent Changes in Eyeglass Prescription: As the cataract progresses, the lens’s power can change, leading to a need for more frequent updates to your glasses.
- Double Vision in One Eye: In some cases, a cataract can cause diplopia (double vision) that resolves when the affected eye is covered.
- “Second Sight”: Paradoxically, some individuals with a specific type of cataract (nuclear cataract) may experience a temporary improvement in their near vision, allowing them to read without glasses again, before the vision eventually worsens.
While the vast majority of cataracts are age-related, developing gradually as part of the natural aging process, they can also be triggered or exacerbated by other factors. These include:
- Eye Injury: Traumatic cataracts can form after a direct blow to the eye or penetrating injury.
- Certain Medical Conditions: Diabetes, for instance, can increase the risk and accelerate the development of cataracts due to elevated blood sugar levels affecting the lens. Other conditions like hypocalcemia can also play a role.
- Prolonged Use of Specific Medications: Long-term use of corticosteroids (oral, inhaled, or topical eye drops) is a well-known risk factor for cataract formation.
- Excessive Exposure to Ultraviolet (UV) Light: Unprotected exposure to sunlight over many years is believed to contribute to cataract development, emphasizing the importance of sunglasses.
- Smoking and Alcohol Consumption: Both have been linked to an increased risk of cataracts.
- Previous Eye Surgery: In rare cases, some other eye surgeries can lead to cataract formation.
- Genetics: A family history of cataracts may indicate a higher predisposition.
When visual impairment from cataracts begins to significantly interfere with a person’s daily activities – such as reading, driving, cooking, watching television, or recognizing faces – and detracts from their overall quality of life, surgical removal becomes the necessary and most effective course of action. Unlike vision problems corrected with glasses or contact lenses, cataracts cannot be resolved through non-surgical means.
What is Phaco Surgery? Our Detailed Explanation
Phacoemulsification, more commonly known as Phaco Surgery, stands as the gold standard in modern cataract removal procedures. It is an advanced, highly refined, and minimally invasive surgical technique meticulously designed to restore clear vision by addressing the clouding of the eye’s natural lens – a condition known as a cataract.
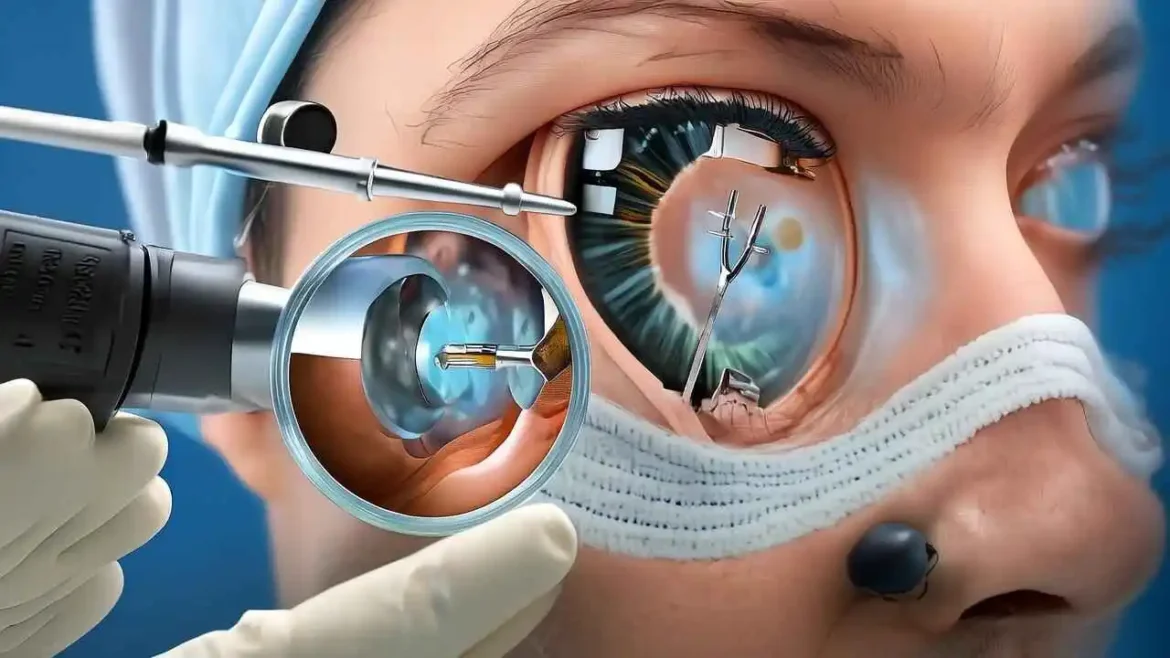
The very name ‘Phacoemulsification’ offers a literal insight into its core function: ‘phako’ is derived from the Greek word for lens, and ’emulsification’ refers to the process of breaking down a substance into a fine, liquid-like suspension or emulsion. True to its name, this procedure employs highly precise, high-frequency ultrasound energy. This energy generates rapid, controlled vibrations that meticulously break up the hardened, cloudy natural lens into micro-fine fragments. These delicate fragments are then gently but efficiently suctioned out of the eye through the same tiny incision, leaving the eye’s internal structures intact and clean.
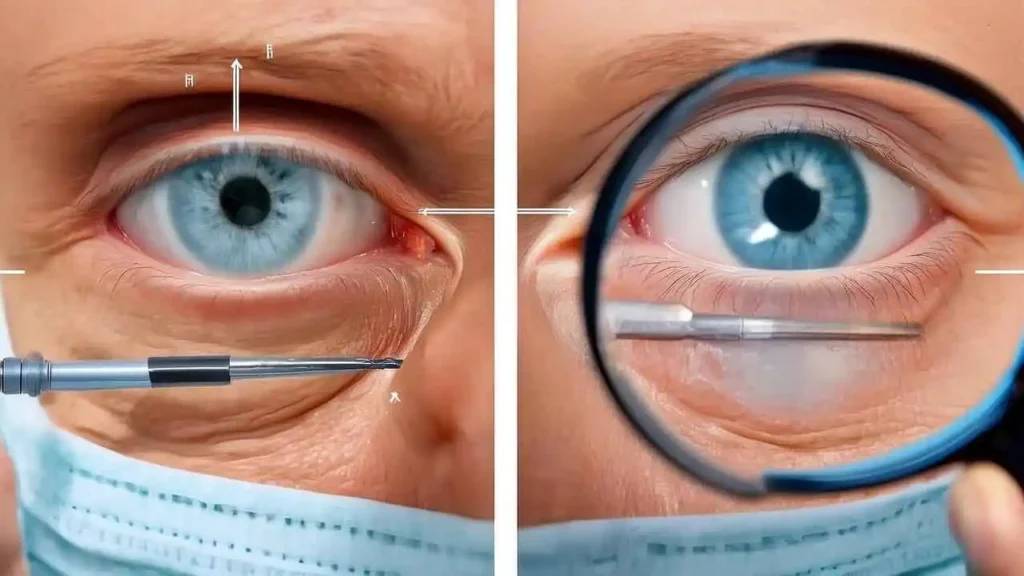
The surgical journey begins with an almost imperceptible incision, typically less than 3 millimeters in size – often no larger than a tiny pinprick – made strategically on the very edge of the cornea, which is the transparent, dome-shaped front surface of the eye. This micro-incision is carefully crafted to be self-sealing, often requiring no stitches to close.
Through this minuscule opening, a specialized, ultra-thin probe is carefully advanced into the eye. This sophisticated probe is the instrument that delivers the controlled ultrasonic waves directly to the cataractous lens. As these precisely calibrated ultrasonic waves are emitted, they work their magic, transforming the dense, opaque lens material into a liquid consistency.
Once the entire cloudy lens has been successfully emulsified and thoroughly removed, the next crucial step involves the meticulous insertion of a clear, biocompatible artificial intraocular lens (IOL). This advanced lens, which is specifically chosen for each patient’s unique visual needs, is typically folded during insertion and then gently unfolded inside the eye, where it permanently takes the place of the previously diseased natural lens. The result is a remarkable restoration of sharp, vibrant vision, often providing immediate and long-lasting clarity that significantly enhances a patient’s quality of life.
Key Features of Phaco Surgery: Why We Consider it the Gold Standard – The Phacoemulsification Process: A Step-by-Step Overview
Phacoemulsification, commonly known as Phaco surgery, stands as the undeniable gold standard for cataract removal worldwide. Its preeminence is not accidental but stems from a meticulously refined approach that incorporates cutting-edge technology and patient-centric design. The following key features are precisely why we consider it the superior choice, consistently delivering excellent outcomes and significantly enhancing our patients’ quality of life:
- Minimally Invasive Approach: This is arguably the cornerstone of Phaco’s success. Unlike older methods that required larger incisions, Phaco surgery employs an incredibly small incision, typically less than 3 millimeters, made at the edge of the cornea. This tiny opening dramatically reduces trauma to the delicate eye tissues, leading to a host of benefits. In many cases, these micro-incisions are designed to be self-sealing, eliminating the need for sutures. This not only minimizes post-operative discomfort but also accelerates the healing process and significantly reduces the risk of surgically induced astigmatism, which can occur with stitches. The smaller incision also means less disruption to the eye’s natural structure and quicker return to normal function.
- High Success Rate: Phacoemulsification boasts an exceptionally high success rate, consistently exceeding 95%, in improving visual acuity and alleviating cataract-related symptoms like blurriness, glare, and faded colors. This remarkable efficacy is a testament to the procedure’s precision and the advanced technology involved. We have witnessed countless patients experience a profound transformation, regaining their independence, resuming hobbies, and enjoying a significantly improved quality of life as their vision is restored to clarity.
- Rapid Visual Recovery: Due to its minimally invasive nature and the advanced techniques employed, patients typically experience a remarkably fast visual recovery compared to older, more invasive cataract removal methods. Many individuals report a noticeable improvement in their vision within mere hours after the procedure, with significant clarity often achieved within a few days. This rapid recovery means patients can quickly return to their daily routines and enjoy the benefits of their improved vision with minimal downtime.
- Reduced Risk of Complications: While no surgical procedure is entirely without risk, the sophisticated technology, unparalleled precision, and controlled environment of Phaco surgery significantly minimize the chances of complications. The small incision size and precise manipulation of the cloudy lens reduce the risk of infection, inflammation, and capsular rupture (damage to the delicate membrane that holds the new lens). Our meticulous techniques and advanced equipment contribute to a safer procedure with predictable and favorable outcomes for the vast majority of patients.
- Outpatient Procedure: Phaco surgery is almost universally performed on an outpatient basis, making it incredibly convenient for patients. This means that after a relatively short procedure, typically lasting 15-30 minutes, patients can return home on the same day. This eliminates the need for an overnight hospital stay, significantly reducing costs, enhancing patient comfort, and minimizing disruption to their personal lives. It underscores the safety and efficiency of the modern Phaco technique.
- Advanced Intraocular Lens (IOL) Options: Once the cataract-clouded natural lens is expertly emulsified and removed, the most remarkable part of the procedure takes place: the implantation of a state-of-the-art Intraocular Lens (IOL). These aren’t just simple replacement lenses; they are marvels of optical engineering designed to correct various refractive errors and provide patients with the best possible post-operative vision, potentially reducing or even eliminating their dependence on glasses. We offer a wide array of choices, tailored to individual needs and lifestyles:
- Monofocal IOLs: These traditional IOLs provide excellent, clear vision at a single focal distance, typically optimized for far vision. While highly effective for distance clarity, patients implanted with monofocal IOLs will generally still require reading glasses for near tasks.
- Multifocal IOLs: Representing an advanced solution, multifocal IOLs are engineered with multiple focal points, similar to progressive eyeglasses. They are designed to provide clear vision at various distances – near, intermediate, and far – potentially freeing patients from the need for reading glasses and distance glasses for most activities.
- Toric IOLs: For patients with astigmatism (an irregularly shaped cornea or lens that causes blurry or distorted vision), Toric IOLs are a revolutionary option. These specialized lenses are precisely oriented within the eye to correct the astigmatism concurrently with cataract removal, leading to significantly sharper and clearer vision.
- Extended Depth of Focus (EDOF) IOLs: Bridging the gap between monofocal and multifocal lenses, EDOF IOLs provide a continuous, elongated range of vision, typically from intermediate to far distances. They offer excellent functional vision across various activities with fewer visual disturbances like halos or glare that some multifocal designs might cause, making them an excellent choice for many.
- Precision and Control: The success of Phaco surgery hinges on the incredible precision and control afforded by the technology. High-frequency ultrasound energy is used to gently emulsify (break up) the cloudy cataract into tiny fragments, which are then meticulously aspirated from the eye through the small incision. This process is performed under the guidance of powerful, high-magnification operating microscopes, allowing the surgeon unparalleled visibility and the ability to target only the diseased lens material while carefully preserving the surrounding healthy ocular tissues. This level of control ensures a safe and effective removal of the cataract.
- Comfort and Safety: Patient comfort and safety are paramount throughout the Phaco procedure. The surgery is typically performed under topical or local anesthesia, meaning the patient remains awake and aware but their eye is completely numb and comfortable. This avoids the risks associated with general anesthesia and allows for a quicker recovery. Throughout the procedure, vital signs are closely monitored by our dedicated medical team to ensure stability and address any concerns immediately, guaranteeing a safe and reassuring experience from beginning to end.
General steps involved in Phaco surgery:
- Preparation: Before the surgery, we administer eye drops to dilate the pupil and often to numb the eye. In some cases, a mild sedative may be given to help us relax and ease any anxiety.
- Incision: We create a minuscule incision, usually between 2 to 3 mm, at the junction of the cornea and sclera (the clear front and white parts of the eye).
- Capsulorhexis: We then create a careful, circular opening in the anterior capsule of the lens, which is the very thin, transparent membrane enclosing the natural lens. This precise opening allows access to the cloudy cataract.
- Phacoemulsification: Our surgeon inserts the ultrasonic probe through the incision. The probe emits high-frequency sound waves that emulsify (break up) the cataract into tiny, manageable pieces. These fragments are simultaneously aspirated (suctioned) out of the eye by the same probe.
- IOL Insertion: Once all the cataractous material is removed, we carefully fold and insert the chosen artificial IOL through the same small incision. The IOL then unfolds gently and settles into its permanent and precise position within the lens capsule.
- Closure: The small corneal incision is often self-sealing due to its specific architecture and doesn’t require stitches. We may hydrate the incision to ensure it seals properly. A protective shield or patch may be placed over the eye to protect it immediately after the procedure.
Benefits of Phaco Surgery: What Our Patients Experience
Beyond the technical features, the true impact of Phaco surgery is reflected in the tangible benefits our patients experience:
- Significantly Improved Vision: The primary benefit is the rapid restoration of clear, sharp vision, often dramatically improving quality of life. Colors appear brighter, and night vision significantly improves, making daily tasks easier and safer.
- Quick Return to Daily Activities: Due to the fast recovery, most patients can resume light, non-strenuous daily activities within a day or two, with full visual recovery typically within a few weeks.
- Minimal Discomfort: The procedure itself is usually pain-free, and most patients report only mild discomfort, a gritty sensation, or slight irritation in the immediate post-operative period.
- Long-Lasting Results: Once successfully implanted, the artificial IOL is a permanent solution for cataracts, meaning the cataract cannot return. The IOL does not wear out or degrade over time.
As Abraham Lincoln once wisely said:
“The best thing about the future is that it comes one day at a time.” And for us, in ophthalmology, this rings true as we continuously strive to bring better vision, one day and one patient at a time, through innovations like Phaco surgery.
Comparison: Phacoemulsification vs. Traditional ECCE