To further appreciate the advancements of Phaco surgery, let’s look at how it compares to older methods like Extracapsular Cataract Extraction (ECCE), which was once the standard:
| Feature | Phacoemulsification (Modern Gold Standard) | Extracapsular Cataract Extraction (Older Method) |
| Incision Size | Small (2-3 mm) | Large (10-12 mm) |
| Sutures Required | Rarely (often self-sealing) | Yes, multiple stitches required |
| Lens Removal Method | Ultrasonic energy emulsifies and suctions lens fragments | Entire lens nucleus removed in one piece, leaving capsule intact |
| Recovery Time | Rapid visual recovery (days to weeks) | Slower visual recovery (weeks to months) |
| Astigmatism Risk | Low, due to small incision | Higher, due to large incision and sutures |
| Outpatient Procedure | Primarily outpatient | Often requires overnight hospital stay |
| Precision | Highly skilled, precise technique with advanced technology | Less technologically advanced, but still requires surgical skill |
| Post-Op Complications | Lower risk of complications like infection, induced astigmatism, and swelling | Higher risk of certain complications due to larger incision and tissue manipulation |
Who is a Candidate for Phaco Surgery (Phacoemulsification)?
Phacoemulsification, commonly known as Phaco surgery, is the most advanced and widely performed cataract removal procedure. Determining candidacy for this surgery is a personalized process that hinges primarily on the degree to which cataracts are impacting an individual’s vision and overall quality of life.
Primary Candidacy Criteria: Symptomatic Visual Impairment
We typically recommend Phaco surgery for individuals whose cataracts have progressed to the point where they are causing significant impairment to their vision and actively interfering with their daily activities. This isn’t solely based on a specific visual acuity reading on an eye chart (though that is a factor), but rather on the patient’s subjective experience and functional limitations.
Common symptoms and functional difficulties that indicate a strong candidacy include:
- Difficulty with Reading: Struggling to read books, newspapers, medication labels, computer screens, or even a smartphone.
- Challenges with Driving: Especially pronounced difficulty with night driving due to increased glare from oncoming headlights, halos around streetlights, reduced contrast, or overall diminished vision in low-light conditions. Daytime driving may also become hazardous.
- Impaired Television Viewing: Finding it hard to see details, distinguish faces, or follow the action on a television screen.
- Difficulty Recognizing Faces: Struggling to identify familiar faces, even at close distances.
- Faded or Dulled Colors: The world may appear less vibrant, as if seen through a yellowed or brownish filter.
- Increased Glare and Light Sensitivity: Experiencing uncomfortable sensitivity to bright lights, sunlight, or indoor lighting, often accompanied by halos or starbursts around light sources.
- Blurry or Cloudy Vision: A general haziness or blur that cannot be corrected with new glasses prescriptions.
- Frequent Changes in Glasses Prescription: Needing more frequent updates to eyeglass prescriptions, but still not achieving satisfactory vision.
- Impact on Hobbies and Work: Inability to perform tasks requiring fine vision, such as sewing, crafting, painting, or specific job-related duties.
The Comprehensive Evaluation Process
To definitively determine if you are a suitable candidate, our experienced ophthalmologist will conduct a thorough and meticulous eye examination. This comprehensive assessment goes beyond a simple vision test and includes:
- Comprehensive Vision Assessment: This includes measuring your visual acuity (what you can see on an eye chart), checking your peripheral vision, and evaluating your vision under various lighting conditions.
- Slit-Lamp Examination: Using a specialized microscope, the ophthalmologist will closely examine the front structures of your eye, including the lens, to precisely assess the type, size, and density of the cataract.
- Dilated Eye Exam: Eye drops will be used to dilate your pupils, allowing the ophthalmologist a clear view of the retina, optic nerve, and other structures at the back of your eye. This helps rule out other co-existing eye conditions that might affect vision or the surgical outcome.
- Measurement of the Eye (Biometry): Precise measurements of your eye’s length, curvature of the cornea, and depth of the anterior chamber are taken. These measurements are crucial for calculating the correct power of the intraocular lens (IOL) that will be implanted during surgery to restore clear vision.
- Discussion of Medical History: We will review your general health, any pre-existing medical conditions (e.g., diabetes, hypertension), and all medications you are currently taking, as these can influence surgical planning and recovery.
- Discussion of Lifestyle and Expectations: Your lifestyle, visual demands (e.g., do you drive a lot, do close-up work, etc.), and what you hope to achieve with surgery are vital considerations.
Beyond Symptoms: Other Considerations
While symptomatic visual impairment is the primary driver, there are instances where surgery might be recommended even with milder symptoms:
- Management of Other Eye Conditions: In some cases, a dense cataract may obscure the view of the retina, making it difficult to diagnose or treat other serious eye conditions like diabetic retinopathy or macular degeneration. Removing the cataract then becomes necessary to monitor and manage these conditions effectively.
- Prevention of Complications: Very advanced, untreated cataracts can sometimes lead to complications such as inflammation or increased eye pressure (glaucoma).
Personalized Decision-Making
Ultimately, the decision to proceed with Phaco surgery is a shared one between you and your ophthalmologist. After a thorough evaluation, your doctor will discuss the best course of action for your specific needs, explaining the benefits, risks, and expected outcomes. Our goal is to enhance your vision, improve your quality of life, and help you regain independence in your daily activities.
Post-Operative Care: Our Recommendations for a Smooth and Successful Recovery
Embarking on the journey to clearer vision after Phaco surgery is an exciting step. To ensure optimal healing and achieve the best possible visual outcome, careful and diligent adherence to our post-operative instructions is absolutely crucial. Your commitment to these guidelines will significantly contribute to a smooth and complication-free recovery. We will provide detailed, personalized guidance during your pre-operative and post-operative consultations, but generally, this vital recovery phase involves:
- Meticulous Eye Drop Administration: Consider these your most potent allies in the healing process. You will be prescribed a specific regimen of eye drops, typically including antibiotics to prevent potential infections and anti-inflammatory drops to reduce swelling, discomfort, and promote optimal healing of the ocular tissues.
- Importance: These drops are vital for preventing serious complications and facilitating successful tissue repair. Missing doses or stopping prematurely can lead to infection, inflammation, and compromise your final visual result.
- Technique: It’s essential to meticulously follow the prescribed schedule and technique. Always wash your hands thoroughly before handling the drops. Tilt your head back, gently pull down your lower eyelid, and administer the drop into the pocket created, avoiding contact between the dropper tip and your eye or eyelashes. Close your eye gently for a moment afterward.
- Duration: Expect to continue using these drops for several weeks, with the frequency gradually tapering down as advised by your ophthalmologist. Never discontinue use prematurely without explicit instructions.
- Consistent Protective Eyewear: A clear plastic shield or specific protective glasses will be provided to you. Wearing this eyewear is a non-negotiable part of your early recovery.
- Purpose: Its primary role is to create a physical barrier, effectively preventing accidental rubbing, bumping, or injury to the delicate operated eye. This is especially critical during sleep, as unconscious movements can inadvertently cause damage.
- When to Wear: You will likely be instructed to wear the shield continuously for the first 24-48 hours, then typically during sleep for at least one to two weeks. It’s also highly recommended to wear it or your protective glasses during the day in environments with dust, wind, or potential for accidental impact.
- Think of it as a temporary guardian safeguarding your healing eye from unforeseen hazards.
- Prudent Activity Restrictions: For the initial few weeks, your eye needs a period of tranquility to heal properly and prevent any complications that could arise from increased pressure or physical strain.
- Heavy Lifting & Strenuous Activities: Strictly avoid any activities that require straining, such as heavy lifting, bending over from the waist (which can increase pressure in the head and eye), vigorous exercise (like jogging, weightlifting, high-impact sports), or any activity that puts undue strain on your body. These can cause a dangerous spike in intraocular pressure, potentially affecting the healing incision or the position of the new lens.
- Water Exposure: Swimming, soaking in hot tubs, and visiting saunas or steam rooms are completely prohibited for several weeks. These activities pose a significant risk of infection from waterborne bacteria and other pathogens entering the healing eye.
- Other Restrictions: Avoid dusty or smoky environments, and refrain from rubbing your eyes. Generally, light walking, reading, watching TV, and light household chores are permissible unless advised otherwise.
- Absolute Avoidance of Eye Rubbing or Pressure: This is perhaps the single most critical instruction for your post-operative period. It is vital not to rub, press on, or apply any form of pressure to the operated eye.
- Why it’s Crucial: The delicate healing incision is still fragile, and the newly implanted intraocular lens (IOL) needs to settle securely into its position. Rubbing or pressing can easily dislodge the IOL, re-open the incision, or introduce infection, leading to serious complications that could compromise your vision and require further intervention.
- If You Experience Irritation: Resist the urge to rub. Instead, you may gently dab around the eye with a clean tissue, or instill artificial tears if advised by your doctor, to alleviate discomfort. Always contact our office if you experience significant irritation or pain.
- Diligent Attendance at Follow-up Appointments: These scheduled visits are the cornerstone of your post-operative care and are just as important as your initial surgery. You will typically have appointments the day after surgery, then one week, one month, and potentially three months later, depending on your individual healing process.
- Purpose: During these appointments, our ophthalmologist will meticulously assess your healing progress, measure your intraocular pressure, check the position of the IOL, and monitor your visual acuity. This allows us to promptly identify and address any potential concerns, adjust your medication regimen as needed, and ensure your vision is progressing as expected.
- Your Role: It’s also an invaluable opportunity for you to ask any questions or voice any concerns you may have about your recovery. Please ensure you attend all scheduled appointments.
By diligently following these guidelines, you are actively participating in your own recovery and significantly enhancing the likelihood of achieving the best possible visual outcome. Our team is here to support you every step of the way, so please do not hesitate to contact us with any questions or concerns during your healing process.
Conclusion
In conclusion, Phacoemulsification surgery stands as a testament to the incredible advancements in modern medicine. We have witnessed firsthand how this sophisticated yet minimally invasive procedure has transformed the lives of millions by safely and effectively removing cataracts and restoring clear vision. Its array of features – from the tiny incision and rapid recovery to the customizable IOL options – solidifies its position as the gold standard in cataract treatment. If you or someone you know is experiencing vision problems due to cataracts, we encourage you to consult with an ophthalmologist. Understanding Phaco surgery and its immense benefits is the first step towards experiencing a brighter, clearer world once again, free from the cloudiness of cataracts.
FAQs
- What is Phaco Surgery?
- Phacoemulsification, or Phaco Surgery, is a minimally invasive surgical technique used to remove cataracts from the eye.
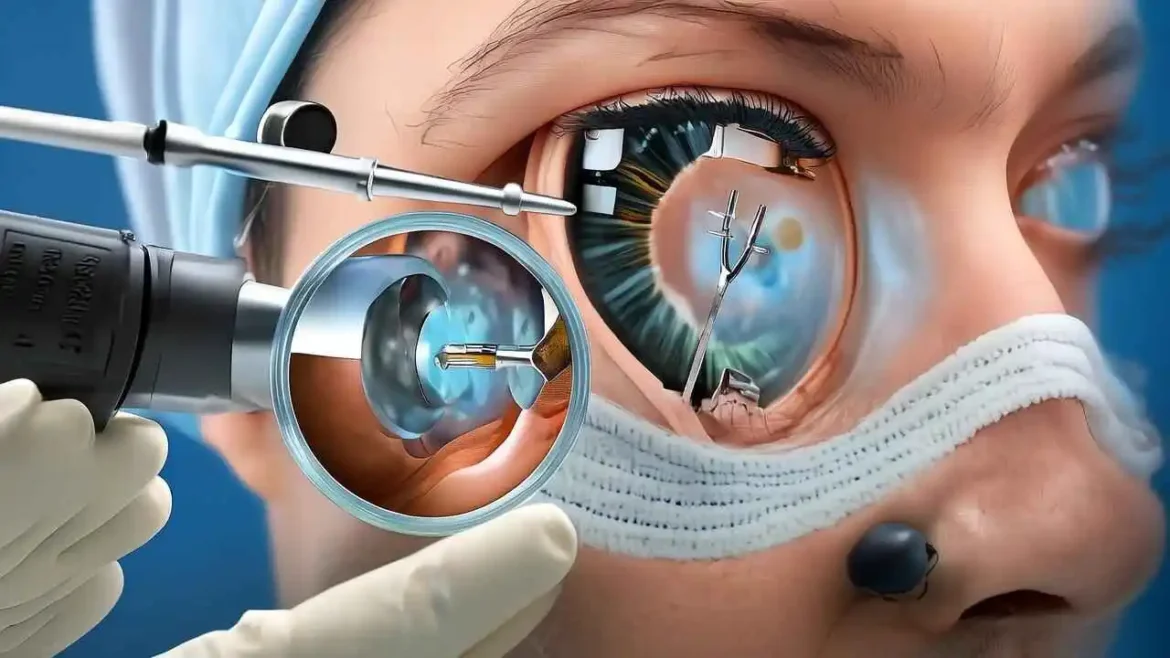
- How does Phaco Surgery work?
- The surgeon uses ultrasound energy to break up the cloudy lens (cataract) into small fragments, which are then suctioned out and replaced with an artificial intraocular lens (IOL).
- Is Phaco Surgery safe?
- Yes, Phaco Surgery is generally considered safe and effective, with a high success rate in restoring vision.
- What are the benefits of Phaco Surgery?
- Benefits include quick recovery, minimal discomfort, and often a rapid improvement in vision.
- Who is a candidate for Phaco Surgery?
- Candidates typically include individuals with significant cataracts affecting their vision, often those over 60 years old.
- How long does the surgery take?
- The actual procedure usually takes about 15 to 30 minutes, but patients should expect to spend several hours at the surgical center.
- Do I need to stay overnight after the surgery?
- Most patients can go home on the same day of the surgery; overnight stays are not typically required.
- What anesthesia is used during Phaco Surgery?
- The procedure usually involves local anesthesia and sedation to ensure comfort without general anesthesia.
- What can I expect during the procedure?
- You will feel mild pressure but should not experience pain. The surgeon will use a microscope to perform the surgery.
- What types of IOLs are available?
- There are various types of IOLs, including monofocal, multifocal, and toric lenses, which cater to different vision needs.
- Is there a risk of complications?
- As with any surgery, there are risks, including infection, bleeding, or retinal detachment, but serious complications are rare.
- How long is the recovery time?
- Most patients notice improved vision within a few days, but full recovery can take several weeks.
- Will I need glasses after surgery?
- Depending on the type of IOL chosen and your vision needs, you may still need glasses for reading or distance vision.
- What precautions should I take after surgery?
- Avoid rubbing your eyes, strenuous activities, and swimming for a few weeks. Follow your surgeon’s specific post-operative instructions.
- Can I drive after Phaco Surgery?
- You may not be able to drive immediately after the procedure. Follow your doctor’s advice and wait until your vision stabilizes.
- How will my vision change after surgery?
- Many patients experience clearer vision, but results can vary, and some may require additional corrections like glasses.
- How often should I attend follow-up appointments?
- Follow-up appointments are usually scheduled within the first week after surgery, and then further evaluation may be done within the month.
- What should I do if I experience pain after surgery?
- Mild discomfort is normal, but if you experience severe pain or sudden vision changes, contact your doctor immediately.
- Does insurance cover Phaco Surgery?
- Most health insurance plans cover Phaco Surgery when cataracts significantly impair vision. Check with your provider for specifics.
- Can cataracts come back after Phaco Surgery?
- While the natural lens removed during surgery cannot grow back, some patients may develop a condition called posterior capsule opacification (PCO).
- What is PCO, and can it be treated?
- PCO is a common secondary cataract condition that can be treated with a quick outpatient procedure called YAG laser capsulotomy.
- Are there alternatives to Phaco Surgery?
- In the early stages of cataracts, vision can sometimes be managed with prescription glasses or contact lenses.
- What should I do to prepare for Phaco Surgery?
- Follow your doctor’s pre-operative instructions, including any special preparations, and arrange for transportation if sedation is used.
- Can I use my regular medications before the surgery?
- Discuss all medications with your doctor, as some may need to be adjusted prior to surgery.
- How can I ensure the best outcome from the surgery?
- Follow all pre-and post-operative instructions, attend follow-up appointments, and communicate any concerns with your healthcare team.
- Is Phaco Surgery performed under sterile conditions?
- Yes, Phaco Surgery is performed in a sterile environment to minimize the risk of infection.
- What technology is used in Phaco Surgery?
- Advanced surgical equipment, including high-frequency ultrasound devices, is used to perform the procedure efficiently and safely.
- What happens if I have other eye conditions along with cataracts?
- Your surgeon will evaluate other eye conditions, as they may impact the approach or outcomes of cataract surgery.
- Can Phaco Surgery correct astigmatism?
- Yes, specialized toric lenses can correct astigmatism during cataract surgery.
- What advancements are being made in Phaco Surgery?
- Continuous advancements include improved IOL technology, enhanced surgical techniques, and better preoperative diagnostic tools.
These FAQs cover common questions and concerns related to Phaco Surgery, providing valuable information for patients considering the procedure. Always consult with a qualified healthcare provider for personalized advice.
Medical Disclaimer:
The information provided on this website is for general educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.